Learning Outcome
After reading this article you will be able to:
- Describe the presentation of acute cholecystitis.
- Recall the nursing diagnosis of acute cholecystitis.
- Summarize the treatment of acute cholecystitis.

After reading this article you will be able to:
the term of Cholecystitis it is referred to inflammation in the gallbladder and it is considered as a surgical condition. This condition can be associated with or without the presence of gallstones. It is also classified as acute or chronic. It is found both in men and women but may have a propensity for certain populations. It may also present with certain classic signs and symptoms. It may also be confused with other illnesses such as peptic ulcer disease, irritable bowel disease, and cardiac disease. Chronic and acute pancreatitis can also mimic gallbladder disease.[1][2][3]
A malfunctioning gallbladder causes cholecystitis. Bile is made in the liver and travels down the bile duct and is stored in the gallbladder. After eating certain foods, especially spicy or greasy foods, the gallbladder is stimulated to empty the bile out of the gallbladder, through the cystic duct, down the bile duct into the duodenum. This process aids in food digestion. If the gallbladder is not functioning properly, for various reasons, the bile may not empty completely. This may lead to stone formation. Gallstones can cause mechanical blockage of the cystic duct. A poorly functioning gallbladder without formation of stones causes acalculous cholecystitis.[4][5]
Gallbladder disease occurs in men and women. Certain populations are more prone to gallbladder disease. The risk of gallbladder disease increases in women, obese patients, pregnant women, and patients in their 40s. Drastic weight loss or acute illnesses may also increase the risk. There is also a family propensity for this condition and the formation of gallstones. Other conditions that cause breakdown of blood cells, for example, sickle cell disease, also increase the incidence of gallstones.
Cases of chronic cholecystitis present with progressing right upper abdominal pain with bloating, food intolerances (especially greasy and spicy foods), increased gas, nausea, and vomiting. Pain in the midback or shoulder may also occur. This pain could be present for years until diagnosis. Cases of acute cholecystitis have similar symptoms only more severe. Often symptoms are mistaken for cardiac issues. The finding of right upper abdominal pain with deep palpation, Murphy's sign, is usually classic for this disease. Often, there is a specific dietary event leading to the acute attack, "I ate pork chops and gravy last night."
A physical exam with a comprehensive history is paramount in making the diagnosis of cholecystitis. A complete blood count (CBC) and a comprehensive metabolic panel are also important. In cases of chronic cholecystitis, these results may be normal. In acute cholecystitis or severe disease, white blood cell count (WBC) may be elevated. Liver enzymes may also be elevated. If there is a high bilirubin level above 2, then consider a possible common bile duct stone. Note that even in the presence of severe gallbladder disease, lab values may be normal. Amylase and lipase must also be checked to rule out pancreatitis. Often a CT scan is ordered in the emergency department as the first test in the work up. Findings of cholecystitis and gallstones can often be seen on this imaging. A gallbladder ultrasound is the best test to evaluate gallbladder disease initially. A thickened gallbladder wall and gallstones are common findings with this condition. In cases of acute cholecystitis, a hepatobiliary (HIDA) scan is recommended. This scan will diagnose gallbladder function or cystic duct obstruction. The addition of cholecystokinin (CCK) in cases of no gallstones may also diagnose acalculous cholecystitis. This is indicated by an ejection fracture less than 35%.[6][7]
The best treatment for cholecystitis is laparoscopic cholecystectomy. There are low morbidity and mortality rates with quick recovery. This can also be done with an open technique in cases where the patient is not a good laparoscopic candidate. In situations in which the patient is acutely ill and considered a poor surgical candidate, he or she may be treated with temporizing percutaneous drainage of the gallbladder. Milder cases of chronic cholecystitis in patients considered poor surgical candidates, they may be treated with dietary adjustments of low-fat and low-spice diets. Results of this treatment vary. Medical treatment of gallstones with ursodiol also has been reported to have occasional success.[8][9][3]
Managing acute cholecystitis is now routine, and most patients have an excellent prognosis. However, problems arise in patients with acalculous cholecystitis and when there are bile duct stones. Patients with acalculous cholecystitis are often managed in the ICU and may undergo an initial aspiration procedure until they are fit to undergo formal surgery. Since many of these patients have high comorbidity, monitoring them is critical. Educating the patient and family is vital since the condition does carry a high mortality. The other group of patients who may have a prolonged stay are those with a bile duct stone. These patients require an ERCP prior to the cholecystectomy. Again ERCP is not a benign procedure, and patients need to be educated about the procedure and potential complications.
Patients with numerous comorbid factors need to be evaluated by the cardiologist prior to general anesthesia. The preoperative nurse should ensure that the patient has the requisite clearance, ECG, Chest x-ray, and blood work prior to the surgery.[10][11][12] (level V)
Outcomes
For patients with uncomplicated acute cholecystitis, the prognosis is excellent. The mortality rates are very low. Perforation or gangrene of the gallbladder may occur in delayed cases.
Patients with acalculous cholecystitis have high mortality varying from 20-50%.
In severe cases of acute cholecystitis, the intense inflammation can make surgery difficult, resulting in injury to the bile duct, which has substantial morbidity.[13][14] (Level V)
Once the gallbladder has been removed, most patients can be discharged on the same day.
The pain is minimal and can be managed by over the counter analgesics. The patient may complain of severe shoulder pain due to retained CO2 from laparoscopic insufflation and should be explained that such pain will dissipate as patient moves and gas is slowly absorbed, which can take up to three days.
Prior to discharge, the patient should be advised on possible intolerance to greasy food, which may cause bloating or diarrhea. This can be temporary or, at some degree permanent, due to the decreased speed of fat emulsification by the loss of stored bile in the gallbladder. Most patients will have an up-regulation in bile production by the liver and will see improvement in symptoms with time.
Follow up time is between 3-4 weeks from operation.
Laparoscopic cholecystectomy is now the standard of care for gallstones.
Cholecystitis can occur in the very young and very old, but the highest incidence is in the fourth decade. The classic mantra of "fat, forty, fertile, and flatulent" often applies. Food intolerances are usually the initiating factor of nausea, vomiting, and bloating, but as this condition progresses, there may be persistent symptoms even when the patient has not eaten. The preferred recommended treatment is the removal of the gallbladder. In the past, this was done through an open laparotomy incision. Now laparoscopic cholecystectomy is the procedure of choice. This procedure has low mortality and morbidity, a quick recovery time (usually one week), and good results. At times, patients present to the primary care practitioner with mild symptoms of cholecystitis and gallstones. This can present a challenge to the physician to know what is the appropriate treatment. Often conservative medical management is recommended. This would include low-fat diet modification and possible weight loss. Unfortunately, for surgeons, these patients often present to the emergency department with symptoms of acute cholecystitis and undergo urgent surgery. This situation also increases operative morbidity rates. Therefore, general surgeons usually recommend patients undergo elective laparoscopic cholecystectomy earlier than later in the course of the disease. Other considerations would be the passing of gallstones into the bile duct causing biliary obstruction and possible pancreatitis.
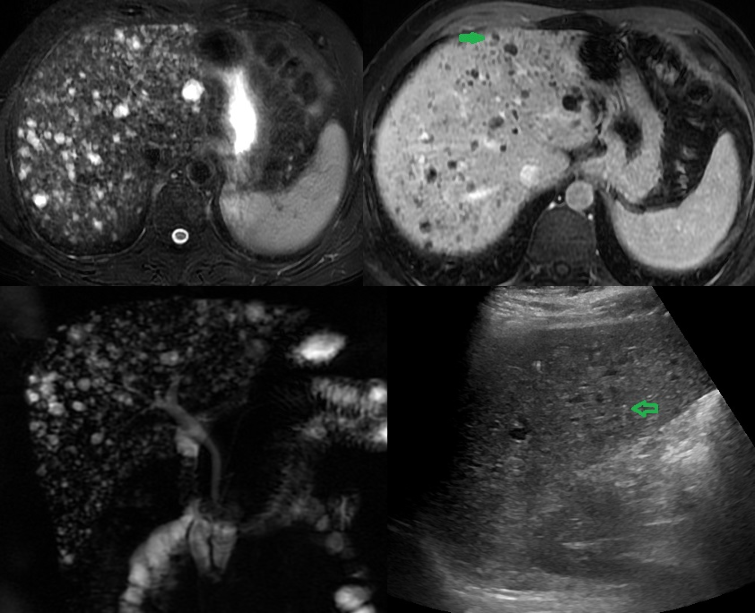
Multiple Biliary Hamartoma. Ultrasound of a 37-year-old female diagnosed with gallstones with acute cholecystitis. The incidental findings: (A) US image shows multiple hypoechoic lesions, some of them with comet-tail artifacts, raising the possibility of multiple biliary hamartoma. (B) T2-weighted MRI shows numerous cystic lesions with a signal similar to CSF. (C) Post-contrast T2 weighted MRI shows some of these lesions with enhancing mural nodule, highly specific for biliary hamartoma. (D) MRCP 3D projection image has more lesions and demonstrates no communication with normal caliber biliary duct.
Contributed by A Borhani, MD
Burmeister G, Hinz S, Schafmayer C. [Acute Cholecystitis]. Zentralblatt fur Chirurgie. 2018 Aug:143(4):392-399. doi: 10.1055/a-0631-9463. Epub 2018 Aug 22 [PubMed PMID: 30134498]
Walsh K, Goutos I, Dheansa B. Acute Acalculous Cholecystitis in Burns: A Review. Journal of burn care & research : official publication of the American Burn Association. 2018 Aug 17:39(5):724-728. doi: 10.1093/jbcr/irx055. Epub [PubMed PMID: 29931066]
Kohga A, Suzuki K, Okumura T, Yamashita K, Isogaki J, Kawabe A, Kimura T. Is postponed laparoscopic cholecystectomy justified for acute cholecystitis appearing early after onset? Asian journal of endoscopic surgery. 2019 Jan:12(1):69-73. doi: 10.1111/ases.12482. Epub 2018 Mar 25 [PubMed PMID: 29577610]
Yun SP, Seo HI. Clinical aspects of bile culture in patients undergoing laparoscopic cholecystectomy. Medicine. 2018 Jun:97(26):e11234. doi: 10.1097/MD.0000000000011234. Epub [PubMed PMID: 29952986]
Wilkins T, Agabin E, Varghese J, Talukder A. Gallbladder Dysfunction: Cholecystitis, Choledocholithiasis, Cholangitis, and Biliary Dyskinesia. Primary care. 2017 Dec:44(4):575-597. doi: 10.1016/j.pop.2017.07.002. Epub 2017 Oct 5 [PubMed PMID: 29132521]
Halpin V. Acute cholecystitis. BMJ clinical evidence. 2014 Aug 20:2014():. pii: 0411. Epub 2014 Aug 20 [PubMed PMID: 25144428]
Behari A, Kapoor VK. Asymptomatic Gallstones (AsGS) - To Treat or Not to? The Indian journal of surgery. 2012 Feb:74(1):4-12. doi: 10.1007/s12262-011-0376-5. Epub 2011 Dec 3 [PubMed PMID: 23372301]
Apolo Romero EX, Gálvez Salazar PF, Estrada Chandi JA, González Andrade F, Molina Proaño GA, Mesías Andrade FC, Cadena Baquero JC. Gallbladder duplication and cholecystitis. Journal of surgical case reports. 2018 Jul:2018(7):rjy158. doi: 10.1093/jscr/rjy158. Epub 2018 Jul 3 [PubMed PMID: 29992010]
Sureka B, Rastogi A, Mukund A, Thapar S, Bhadoria AS, Chattopadhyay TK. Gangrenous cholecystitis: Analysis of imaging findings in histopathologically confirmed cases. The Indian journal of radiology & imaging. 2018 Jan-Mar:28(1):49-54. doi: 10.4103/ijri.IJRI_421_16. Epub [PubMed PMID: 29692527]
Tootian Tourghabe J, Arabikhan HR, Alamdaran A, Zamani Moghadam H. Emergency Medicine Resident versus Radiologist in Detecting the Ultrasonographic Signs of Acute Cholecystitis; a Diagnostic Accuracy Study. Emergency (Tehran, Iran). 2018:6(1):e19 [PubMed PMID: 30009221]
Joshi G, Crawford KA, Hanna TN, Herr KD, Dahiya N, Menias CO. US of Right Upper Quadrant Pain in the Emergency Department: Diagnosing beyond Gallbladder and Biliary Disease. Radiographics : a review publication of the Radiological Society of North America, Inc. 2018 May-Jun:38(3):766-793. doi: 10.1148/rg.2018170149. Epub [PubMed PMID: 29757718]
Thangavelu A, Rosenbaum S, Thangavelu D. Timing of Cholecystectomy in Acute Cholecystitis. The Journal of emergency medicine. 2018 Jun:54(6):892-897. doi: 10.1016/j.jemermed.2018.02.045. Epub 2018 May 8 [PubMed PMID: 29752150]
Ke CW, Wu SD. Comparison of Emergency Cholecystectomy with Delayed Cholecystectomy After Percutaneous Transhepatic Gallbladder Drainage in Patients with Moderate Acute Cholecystitis. Journal of laparoendoscopic & advanced surgical techniques. Part A. 2018 Jun:28(6):705-712. doi: 10.1089/lap.2017.0502. Epub 2018 Apr 16 [PubMed PMID: 29658839]
Yeh DD, Chang Y, Tabrizi MB, Yu L, Cropano C, Fagenholz P, King DR, Kaafarani HMA, de Moya M, Velmahos G. Derivation and validation of a practical Bedside Score for the diagnosis of cholecystitis. The American journal of emergency medicine. 2019 Jan:37(1):61-66. doi: 10.1016/j.ajem.2018.04.051. Epub 2018 Apr 25 [PubMed PMID: 29724580]
Gulaya K, Desai SS, Sato K. Percutaneous Cholecystostomy: Evidence-Based Current Clinical Practice. Seminars in interventional radiology. 2016 Dec:33(4):291-296 [PubMed PMID: 27904248]
Bagla P, Sarria JC, Riall TS. Management of acute cholecystitis. Current opinion in infectious diseases. 2016 Oct:29(5):508-13. doi: 10.1097/QCO.0000000000000297. Epub [PubMed PMID: 27429137]
Kohga A, Suzuki K, Okumura T, Yamashita K, Isogaki J, Kawabe A, Kimura T. Outcomes of early versus delayed laparoscopic cholecystectomy for acute cholecystitis performed at a single institution. Asian journal of endoscopic surgery. 2019 Jan:12(1):74-80. doi: 10.1111/ases.12487. Epub 2018 Apr 3 [PubMed PMID: 29611896]
Ahmed O, Rogers AC, Bolger JC, Mastrosimone A, Lee MJ, Keeling AN, Cheriyan D, Robb WB. Meta-analysis of outcomes of endoscopic ultrasound-guided gallbladder drainage versus percutaneous cholecystostomy for the management of acute cholecystitis. Surgical endoscopy. 2018 Apr:32(4):1627-1635. doi: 10.1007/s00464-018-6041-3. Epub 2018 Feb 5 [PubMed PMID: 29404731]