[1]
Sonthalia S, Pasquali P, Agrawal M, Sharma P, Jha AK, Errichetti E, Lallas A, Sehgal VN. Dermoscopy Update: Review of Its Extradiagnostic and Expanding Indications and Future Prospects. Dermatology practical & conceptual. 2019 Oct:9(4):253-264. doi: 10.5826/dpc.0904a02. Epub 2019 Oct 31
[PubMed PMID: 31723457]
[2]
Carlioz V, Perier-Muzet M, Debarbieux S, Amini-Adle M, Dalle S, Duru G, Thomas L. Intraoperative dermoscopy features of subungual squamous cell carcinoma: a study of 53 cases. Clinical and experimental dermatology. 2021 Jan:46(1):82-88. doi: 10.1111/ced.14345. Epub 2020 Sep 12
[PubMed PMID: 32569407]
Level 3 (low-level) evidence
[3]
Lencastre A, Lamas A, Sá D, Tosti A. Onychoscopy. Clinics in dermatology. 2013 Sep-Oct:31(5):587-93. doi: 10.1016/j.clindermatol.2013.06.016. Epub
[PubMed PMID: 24079588]
[4]
Hirata SH, Yamada S, Almeida FA, Tomomori-Yamashita J, Enokihara MY, Paschoal FM, Enokihara MM, Outi CM, Michalany NS. Dermoscopy of the nail bed and matrix to assess melanonychia striata. Journal of the American Academy of Dermatology. 2005 Nov:53(5):884-6
[PubMed PMID: 16243149]
[5]
Di Chiacchio ND, Farias DC, Piraccini BM, Hirata SH, Richert B, Zaiac M, Daniel R, Fanti PA, Andre J, Ruben BS, Fleckman P, Rich P, Haneke E, Chang P, Cherit JD, Scher R, Tosti A. Consensus on melanonychia nail plate dermoscopy. Anais brasileiros de dermatologia. 2013 Mar-Apr:88(2):309-13. doi: 10.1590/S0365-05962013000200029. Epub
[PubMed PMID: 23739699]
Level 3 (low-level) evidence
[6]
Iorizzo M, Rubin AI, Starace M. Nail lichen striatus: Is dermoscopy useful for the diagnosis? Pediatric dermatology. 2019 Nov:36(6):859-863. doi: 10.1111/pde.13916. Epub 2019 Jul 30
[PubMed PMID: 31359464]
[7]
Gao J, Fei W, Shen C, Shen X, Sun M, Xu N, Li Q, Huang C, Zhang T, Ko R, Cui Y, Yang C. Dermoscopic Features Summarization and Comparison of Four Types of Cutaneous Vascular Anomalies. Frontiers in medicine. 2021:8():692060. doi: 10.3389/fmed.2021.692060. Epub 2021 Jun 28
[PubMed PMID: 34262918]
[8]
Lake A, Jones B. Dermoscopy: to cross-polarize, or not to cross-polarize, that is the question. Journal of visual communication in medicine. 2015 Jun:38(1-2):36-50. doi: 10.3109/17453054.2015.1046371. Epub
[PubMed PMID: 26203939]
[9]
Weber P, Tschandl P, Sinz C, Kittler H. Dermatoscopy of Neoplastic Skin Lesions: Recent Advances, Updates, and Revisions. Current treatment options in oncology. 2018 Sep 20:19(11):56. doi: 10.1007/s11864-018-0573-6. Epub 2018 Sep 20
[PubMed PMID: 30238167]
Level 3 (low-level) evidence
[10]
Pulawska-Czub A, Pieczonka TD, Mazurek P, Kobielak K. The Potential of Nail Mini-Organ Stem Cells in Skin, Nail and Digit Tips Regeneration. International journal of molecular sciences. 2021 Mar 11:22(6):. doi: 10.3390/ijms22062864. Epub 2021 Mar 11
[PubMed PMID: 33799809]
[11]
de Berker D. Nail anatomy. Clinics in dermatology. 2013 Sep-Oct:31(5):509-15. doi: 10.1016/j.clindermatol.2013.06.006. Epub
[PubMed PMID: 24079579]
[12]
Haneke E. Nail psoriasis: clinical features, pathogenesis, differential diagnoses, and management. Psoriasis (Auckland, N.Z.). 2017:7():51-63. doi: 10.2147/PTT.S126281. Epub 2017 Oct 16
[PubMed PMID: 29387608]
[13]
TERRY RB. The onychodermal band in health and disease. Lancet (London, England). 1955 Jan 22:268(6856):179-81
[PubMed PMID: 13234317]
[14]
Oiso N, Kurokawa I, Kawada A. Nail isthmus: a distinct region of the nail apparatus. Dermatology research and practice. 2012:2012():925023. doi: 10.1155/2012/925023. Epub 2012 Feb 9
[PubMed PMID: 22454634]
[15]
Baltz JO, Jellinek NJ. Nail Surgery: Six Essential Techniques. Dermatologic clinics. 2021 Apr:39(2):305-318. doi: 10.1016/j.det.2020.12.015. Epub 2021 Feb 11
[PubMed PMID: 33745642]
[16]
Papaioannou I, Pantazidou G, Repantis T, Mousafeiris VK, Kalyva N. Late-Onset Hematoma Due to Bleeding of a Small Branch of the Lateral Circumflex Femoral Artery Following Proximal Femur Intramedullary Nailing. Cureus. 2022 Mar:14(3):e23513. doi: 10.7759/cureus.23513. Epub 2022 Mar 26
[PubMed PMID: 35495014]
[17]
Grover C, Jakhar D, Mishra A, Singal A. Nail-fold capillaroscopy for the dermatologists. Indian journal of dermatology, venereology and leprology. 2022 May-Jun:88(3):300-312. doi: 10.25259/IJDVL_514_20. Epub
[PubMed PMID: 34877857]
[18]
Lambova SN, Müller-Ladner U. The specificity of capillaroscopic pattern in connective autoimmune diseases. A comparison with microvascular changes in diseases of social importance: arterial hypertension and diabetes mellitus. Modern rheumatology. 2009:19(6):600-5. doi: 10.1007/s10165-009-0221-x. Epub
[PubMed PMID: 19779765]
[19]
Shinohara T, Hirata H. Glomus Tumor Originating from a Digital Nerve. Plastic and reconstructive surgery. Global open. 2019 Jun:7(6):e2053. doi: 10.1097/GOX.0000000000002053. Epub 2019 Jun 5
[PubMed PMID: 31624656]
[20]
Lee JK, Kim TS, Kim DW, Han SH. Multiple glomus tumours in multidigit nail bed. Handchirurgie, Mikrochirurgie, plastische Chirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Handchirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Mikrochirurgie der Peripheren Nerven und Gefasse : Organ der V.... 2017 Oct:49(5):321-325. doi: 10.1055/s-0043-115115. Epub 2017 Oct 17
[PubMed PMID: 29041022]
[21]
Kumar S, Tiwary SK, More R, Kumar P, Khanna AK. Digital glomus tumor: An experience of 57 cases over 20 years. Journal of family medicine and primary care. 2020 Jul:9(7):3514-3517. doi: 10.4103/jfmpc.jfmpc_446_20. Epub 2020 Jul 30
[PubMed PMID: 33102323]
Level 3 (low-level) evidence
[22]
Güneş P, Göktay F. Melanocytic Lesions of the Nail Unit. Dermatopathology (Basel, Switzerland). 2018 Jul-Sep:5(3):98-107. doi: 10.1159/000490557. Epub 2018 Jul 24
[PubMed PMID: 30197884]
[24]
Prevezas C, Triantafyllopoulou I, Belyayeva H, Sgouros D, Konstantoudakis S, Panayiotides I, Rigopoulos D. Giant Onychomatricoma of the Great Toenail: Case Report and Review Focusing on Less Common Variants. Skin appendage disorders. 2016 May:1(4):202-8. doi: 10.1159/000445386. Epub 2016 Apr 20
[PubMed PMID: 27386467]
Level 3 (low-level) evidence
[25]
Perrin C, Baran R, Pisani A, Ortonne JP, Michiels JF. The onychomatricoma: additional histologic criteria and immunohistochemical study. The American Journal of dermatopathology. 2002 Jun:24(3):199-203
[PubMed PMID: 12140434]
[26]
Ríos-Viñuela E, Manrique-Silva E, Nagore E, Nájera-Botello L, Requena L, Requena C. Subungual Melanocytic Lesions in Pediatric Patients. Actas dermo-sifiliograficas. 2022 Apr:113(4):388-400. doi: 10.1016/j.ad.2021.10.007. Epub 2021 Nov 11
[PubMed PMID: 35623729]
[27]
Güldiken G, Göktay F, Atış G, Güneş P. Evaluation of the Demographic and Clinical Features of Patients With Digital Myxoid Pseudocysts and Their Response to Treatment. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2022 Jun 1:48(6):625-630. doi: 10.1097/DSS.0000000000003433. Epub 2022 Mar 23
[PubMed PMID: 35333205]
[28]
Bae TH, Kim HS, Lee JS. Eponychial flap elevation method for surgical excision of a subungual glomus tumor. Dermatologic therapy. 2020 Nov:33(6):e14330. doi: 10.1111/dth.14330. Epub 2020 Oct 7
[PubMed PMID: 32975348]
[29]
Shin JO, Roh D, Son JH, Shin K, Kim HS, Ko HC, Kim BS, Kim MB. Onychophagia: detailed clinical characteristics. International journal of dermatology. 2022 Mar:61(3):331-336. doi: 10.1111/ijd.15861. Epub 2021 Aug 20
[PubMed PMID: 34416026]
[30]
Oiso N, Narita T, Tsuruta D, Kawara S, Kawada A. Pterygium inversum unguis: aberrantly regulated keratinization in the nail isthmus. Clinical and experimental dermatology. 2009 Oct:34(7):e514-5. doi: 10.1111/j.1365-2230.2009.03601.x. Epub
[PubMed PMID: 19747338]
[31]
Oiso N, Kurokawa I, Tsuruta D, Narita T, Chikugo T, Tsubura A, Kimura M, Baran R, Kawada A. The histopathological feature of the nail isthmus in an ectopic nail. The American Journal of dermatopathology. 2011 Dec:33(8):841-4. doi: 10.1097/DAD.0b013e3181f96bce. Epub
[PubMed PMID: 21885945]
[32]
Starace M, Alessandrini A, Piraccini BM. Dermoscopy of the Nail Unit. Dermatologic clinics. 2021 Apr:39(2):293-304. doi: 10.1016/j.det.2020.12.008. Epub 2021 Feb 10
[PubMed PMID: 33745641]
[33]
Lee DK, Lipner SR. Optimal diagnosis and management of common nail disorders. Annals of medicine. 2022 Dec:54(1):694-712. doi: 10.1080/07853890.2022.2044511. Epub
[PubMed PMID: 35238267]
[34]
Lee DK, Chang MJ, Desai AD, Lipner SR. Clinical and dermoscopic findings of benign longitudinal melanonychia due to melanocytic activation differ by skin type and predict likelihood of nail matrix biopsy. Journal of the American Academy of Dermatology. 2022 Oct:87(4):792-799. doi: 10.1016/j.jaad.2022.06.1165. Epub 2022 Jun 22
[PubMed PMID: 35752275]
[35]
Zhou Y, Chen W, Liu ZR, Liu J, Huang FR, Wang DG. Modified shave surgery combined with nail window technique for the treatment of longitudinal melanonychia: Evaluation of the method on a series of 67 cases. Journal of the American Academy of Dermatology. 2019 Sep:81(3):717-722. doi: 10.1016/j.jaad.2019.03.065. Epub 2019 Mar 28
[PubMed PMID: 30930088]
Level 3 (low-level) evidence
[36]
Dellatorre G, Gadens GA, Polo Silveira L, Kose K, Marghoob AA. Video-based wide area digital dermoscopy. Journal of the American Academy of Dermatology. 2022 Oct:87(4):e125-e126. doi: 10.1016/j.jaad.2021.06.842. Epub 2021 Jun 17
[PubMed PMID: 34146617]
[37]
Piraccini BM, Alessandrini A, Starace M. Onychoscopy: Dermoscopy of the Nails. Dermatologic clinics. 2018 Oct:36(4):431-438. doi: 10.1016/j.det.2018.05.010. Epub
[PubMed PMID: 30201152]
[38]
Campos-do-Carmo G, Ramos-e-Silva M. Dermoscopy: basic concepts. International journal of dermatology. 2008 Jul:47(7):712-9. doi: 10.1111/j.1365-4632.2008.03556.x. Epub
[PubMed PMID: 18613881]
[39]
Jakhar D, Kaur I, Kaul S. Art of performing dermoscopy during the times of coronavirus disease (COVID-19): simple change in approach can save the day! Journal of the European Academy of Dermatology and Venereology : JEADV. 2020 Jun:34(6):e242-e244. doi: 10.1111/jdv.16412. Epub 2020 Apr 27
[PubMed PMID: 32223004]
[40]
González Cortés LF, Prada L, Bonilla JD, Gómez Lopez MT, Rueda LJ, Ibañez E. Onychoscopy in a Colombian population with a diagnosis of toenail onychomycosis: an evaluation study for this diagnostic test. Clinical and experimental dermatology. 2021 Dec:46(8):1427-1433. doi: 10.1111/ced.14706. Epub 2021 Jun 29
[PubMed PMID: 33899948]
[41]
Pan Y, Gareau DS, Scope A, Rajadhyaksha M, Mullani NA, Marghoob AA. Polarized and nonpolarized dermoscopy: the explanation for the observed differences. Archives of dermatology. 2008 Jun:144(6):828-9. doi: 10.1001/archderm.144.6.828. Epub
[PubMed PMID: 18559791]
[42]
Hazarika N, Chauhan P, Divyalakshmi C, Kansal NK, Bahurupi Y. Onychoscopy: a quick and effective tool for diagnosing onychomycosis in a resource-poor setting. Acta dermatovenerologica Alpina, Pannonica, et Adriatica. 2021 Mar:30(1):11-14
[PubMed PMID: 33765751]
[43]
Tasli L, Oguz O. The role of various immersion liquids at digital dermoscopy in structural analysis. Indian journal of dermatology, venereology and leprology. 2011 Jan-Feb:77(1):110. doi: 10.4103/0378-6323.74981. Epub
[PubMed PMID: 21220902]
[44]
Grover C, Jakhar D. Onychoscopy: A practical guide. Indian journal of dermatology, venereology and leprology. 2017 Sep-Oct:83(5):536-549. doi: 10.4103/ijdvl.IJDVL_242_16. Epub
[PubMed PMID: 28485306]
[45]
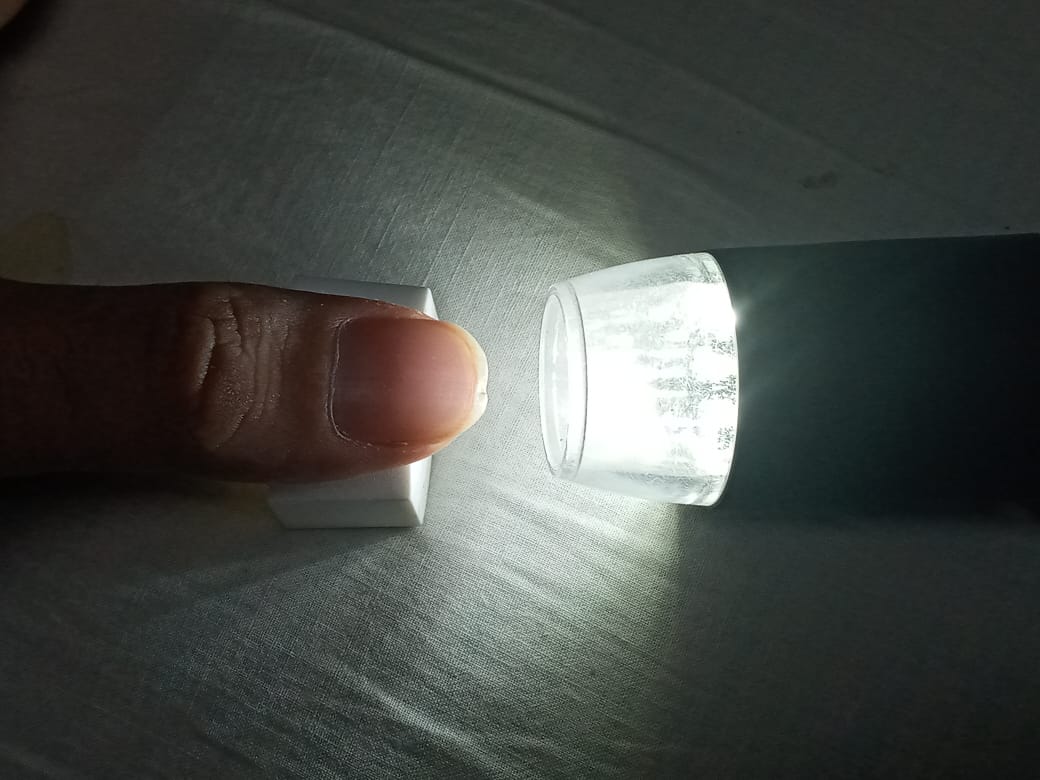
Jakhar D, Kaur I. Transillumination dermoscopy for nail bed pathology. Journal of the American Academy of Dermatology. 2021 Sep:85(3):e137-e138. doi: 10.1016/j.jaad.2017.12.045. Epub 2017 Dec 27
[PubMed PMID: 29288098]
[46]
Di Chiacchio N, Hirata SH, Enokihara MY, Michalany NS, Fabbrocini G, Tosti A. Dermatologists' accuracy in early diagnosis of melanoma of the nail matrix. Archives of dermatology. 2010 Apr:146(4):382-7. doi: 10.1001/archdermatol.2010.27. Epub
[PubMed PMID: 20404227]
[47]
Tosti A, Piraccini BM, de Farias DC. Dealing with melanonychia. Seminars in cutaneous medicine and surgery. 2009 Mar:28(1):49-54. doi: 10.1016/j.sder.2008.12.004. Epub
[PubMed PMID: 19341943]
[48]
Kungvalpivat P, Rojhirunsakool S, Chayavichitsilp P, Suchonwanit P, Wichayachakorn CT, Rutnin S. Clinical and Onychoscopic Features of Benign and Malignant Conditions in Longitudinal Melanonychia in the Thai Population: A Comparative Analysis. Clinical, cosmetic and investigational dermatology. 2020:13():857-865. doi: 10.2147/CCID.S283112. Epub 2020 Nov 19
[PubMed PMID: 33244251]
Level 2 (mid-level) evidence
[49]
Kawabata Y, Ohara K, Hino H, Tamaki K. Two kinds of Hutchinson's sign, benign and malignant. Journal of the American Academy of Dermatology. 2001 Feb:44(2):305-7
[PubMed PMID: 11174394]
[50]
Starace M, Alessandrini A, Bruni F, Piraccini BM. Trachyonychia: a retrospective study of 122 patients in a period of 30 years. Journal of the European Academy of Dermatology and Venereology : JEADV. 2020 Apr:34(4):880-884. doi: 10.1111/jdv.16186. Epub 2020 Jan 30
[PubMed PMID: 31923322]
Level 2 (mid-level) evidence
[51]
Braun RP, Baran R, Saurat JH, Thomas L. Surgical Pearl: Dermoscopy of the free edge of the nail to determine the level of nail plate pigmentation and the location of its probable origin in the proximal or distal nail matrix. Journal of the American Academy of Dermatology. 2006 Sep:55(3):512-3
[PubMed PMID: 16908362]
[52]
Baran R, Simon C. Longitudinal melanonychia: a symptom of Bowen's disease. Journal of the American Academy of Dermatology. 1988 Jun:18(6):1359-60
[PubMed PMID: 3385047]
[53]
Giacomel J, Lallas A, Zalaudek I, Argenziano G. Periungual Bowen disease mimicking chronic paronychia and diagnosed by dermoscopy. Journal of the American Academy of Dermatology. 2014 Sep:71(3):e65-7. doi: 10.1016/j.jaad.2014.01.894. Epub
[PubMed PMID: 25128126]
[54]
Braun RP, Baran R, Le Gal FA, Dalle S, Ronger S, Pandolfi R, Gaide O, French LE, Laugier P, Saurat JH, Marghoob AA, Thomas L. Diagnosis and management of nail pigmentations. Journal of the American Academy of Dermatology. 2007 May:56(5):835-47
[PubMed PMID: 17320240]
[55]
Iorizzo M, Starace M, Di Altobrando A, Alessandrini A, Veneziano L, Piraccini BM. The value of dermoscopy of the nail plate free edge and hyponychium. Journal of the European Academy of Dermatology and Venereology : JEADV. 2021 Dec:35(12):2361-2366. doi: 10.1111/jdv.17521. Epub 2021 Sep 14
[PubMed PMID: 34255894]
[56]
Sato T, Tanaka M. The reason for red streaks on dermoscopy in the distal part of a subungual hemorrhage. Dermatology practical & conceptual. 2014 Apr:4(2):83-5. doi: 10.5826/dpc.0402a18. Epub 2014 Apr 30
[PubMed PMID: 24855582]
[57]
Chiriac A, Brzezinski P, Foia L, Marincu I. Chloronychia: green nail syndrome caused by Pseudomonas aeruginosa in elderly persons. Clinical interventions in aging. 2015:10():265-7. doi: 10.2147/CIA.S75525. Epub 2015 Jan 14
[PubMed PMID: 25609938]
[58]
Baran R, Perrin C. Transverse leukonychia of toenails due to repeated microtrauma. The British journal of dermatology. 1995 Aug:133(2):267-9
[PubMed PMID: 7547396]
[59]
Yorulmaz A, Yalcin B. Dermoscopy as a first step in the diagnosis of onychomycosis. Postepy dermatologii i alergologii. 2018 Jun:35(3):251-258. doi: 10.5114/ada.2018.76220. Epub 2018 Jun 18
[PubMed PMID: 30008642]
[60]
Bhat YJ, Mir MA, Keen A, Hassan I. Onychoscopy: an observational study in 237 patients from the Kashmir Valley of North India. Dermatology practical & conceptual. 2018 Oct:8(4):283-291. doi: 10.5826/dpc.0804a06. Epub 2018 Oct 31
[PubMed PMID: 30479856]
Level 2 (mid-level) evidence
[61]
Bel B, Jeudy G, Vabres P. Dermoscopy of longitudinal leukonychia in Hailey-Hailey disease. Archives of dermatology. 2010 Oct:146(10):1204. doi: 10.1001/archdermatol.2010.226. Epub
[PubMed PMID: 20956678]
[62]
Göktay F, Güldiken G, Altan Ferhatoğlu Z, Güneş P, Atış G, Haneke E. The role of dermoscopy in the diagnosis of subungual glomus tumors. International journal of dermatology. 2022 Jul:61(7):826-832. doi: 10.1111/ijd.16042. Epub 2022 Jan 24
[PubMed PMID: 35073425]
[63]
Bet DL, Reis AL, Di Chiacchio N, Belda Junior W. Dermoscopy and Onychomycosis: guided nail abrasion for mycological samples. Anais brasileiros de dermatologia. 2015 Nov-Dec:90(6):904-6. doi: 10.1590/abd1806-4841.20154615. Epub
[PubMed PMID: 26734877]
[64]
Jesús-Silva MA, Fernández-Martínez R, Roldán-Marín R, Arenas R. Dermoscopic patterns in patients with a clinical diagnosis of onychomycosis-results of a prospective study including data of potassium hydroxide (KOH) and culture examination. Dermatology practical & conceptual. 2015 Apr:5(2):39-44. doi: 10.5826/dpc.0502a05. Epub 2015 Apr 30
[PubMed PMID: 26114050]
[65]
De Crignis G, Valgas N, Rezende P, Leverone A, Nakamura R. Dermatoscopy of onychomycosis. International journal of dermatology. 2014 Feb:53(2):e97-9. doi: 10.1111/ijd.12104. Epub 2013 Jun 20
[PubMed PMID: 23786765]
[66]
Piraccini BM, Starace M, Rubin AI, Di Chiacchio NG, Iorizzo M, Rigopoulos D, A working group of the European Nail Society. Onychomycosis: Recommendations for Diagnosis, Assessment of Treatment Efficacy, and Specialist Referral. The CONSONANCE Consensus Project. Dermatology and therapy. 2022 Apr:12(4):885-898. doi: 10.1007/s13555-022-00698-x. Epub 2022 Mar 9
[PubMed PMID: 35262878]
Level 3 (low-level) evidence
[67]
Gupta AK, Cooper EA. Update in antifungal therapy of dermatophytosis. Mycopathologia. 2008 Nov-Dec:166(5-6):353-67. doi: 10.1007/s11046-008-9109-0. Epub 2008 May 14
[PubMed PMID: 18478357]
[68]
de Berker D. Clinical practice. Fungal nail disease. The New England journal of medicine. 2009 May 14:360(20):2108-16. doi: 10.1056/NEJMcp0804878. Epub
[PubMed PMID: 19439745]
[69]
Murdan S. Drug delivery to the nail following topical application. International journal of pharmaceutics. 2002 Apr 2:236(1-2):1-26
[PubMed PMID: 11891066]
[70]
Zaias N, Escovar SX, Zaiac MN. Finger and toenail onycholysis. Journal of the European Academy of Dermatology and Venereology : JEADV. 2015 May:29(5):848-53. doi: 10.1111/jdv.12862. Epub 2014 Dec 16
[PubMed PMID: 25512134]
[71]
Bodman MA. Point-of-Care Diagnosis of Onychomycosis by Dermoscopy. Journal of the American Podiatric Medical Association. 2017 Sep:107(5):413-418. doi: 10.7547/16-183. Epub
[PubMed PMID: 29077504]
[72]
Ankad BS, Gupta A, Alekhya R, Saipriya M. Dermoscopy of Onycholysis Due to Nail Psoriasis, Onychomycosis and Trauma: A Cross Sectional Study in Skin of Color. Indian dermatology online journal. 2020 Sep-Oct:11(5):777-783. doi: 10.4103/idoj.IDOJ_475_19. Epub 2020 Sep 19
[PubMed PMID: 33235845]
[73]
Piraccini BM, Balestri R, Starace M, Rech G. Nail digital dermoscopy (onychoscopy) in the diagnosis of onychomycosis. Journal of the European Academy of Dermatology and Venereology : JEADV. 2013 Apr:27(4):509-13. doi: 10.1111/j.1468-3083.2011.04323.x. Epub 2011 Nov 1
[PubMed PMID: 22040510]
[74]
Monteagudo-Sánchez B, Luiña-Méndez L, Mosquera-Fernández A. Dermoscopic Features of a Digital Myxoid Cyst. Acta dermatovenerologica Croatica : ADC. 2019 Jun:27(2):129-130
[PubMed PMID: 31351511]
[75]
Kilinc Karaarslan I, Acar A, Aytimur D, Akalin T, Ozdemir F. Dermoscopic features in fungal melanonychia. Clinical and experimental dermatology. 2015 Apr:40(3):271-8. doi: 10.1111/ced.12552. Epub 2014 Dec 16
[PubMed PMID: 25511570]
[76]
Kim HJ, Kim TW, Park SM, Lee HJ, Kim GW, Kim HS, Kim BS, Kim MB, Ko HC. Clinical and Dermoscopic Features of Fungal Melanonychia: Differentiating from Subungual Melanoma. Annals of dermatology. 2020 Dec:32(6):460-465. doi: 10.5021/ad.2020.32.6.460. Epub 2020 Nov 11
[PubMed PMID: 33911788]
[77]
Nagar R, Nayak CS, Deshpande S, Gadkari RP, Shastri J. Subungual hyperkeratosis nail biopsy: a better diagnostic tool for onychomycosis. Indian journal of dermatology, venereology and leprology. 2012 Sep-Oct:78(5):620-4. doi: 10.4103/0378-6323.100579. Epub
[PubMed PMID: 22960819]
[78]
Subhadarshani S, Sarangi J, Verma KK. Dermoscopy of Subungual Wart. Dermatology practical & conceptual. 2019 Jan:9(1):22-23. doi: 10.5826/dpc.0901a06. Epub 2019 Jan 31
[PubMed PMID: 30775143]
[79]
Yorulmaz A, Artuz F. A study of dermoscopic features of nail psoriasis. Postepy dermatologii i alergologii. 2017 Feb:34(1):28-35. doi: 10.5114/ada.2017.65618. Epub 2017 Feb 7
[PubMed PMID: 28286468]
[80]
Yadav TA, Khopkar US. Dermoscopy to Detect Signs of Subclinical Nail Involvement in Chronic Plaque Psoriasis: A Study of 68 Patients. Indian journal of dermatology. 2015 May-Jun:60(3):272-5. doi: 10.4103/0019-5154.156377. Epub
[PubMed PMID: 26120154]
[81]
Farias DC, Tosti A, Chiacchio ND, Hirata SH. [Dermoscopy in nail psoriasis]. Anais brasileiros de dermatologia. 2010 Jan-Feb:85(1):101-3
[PubMed PMID: 20464097]
[82]
Ribeiro CF, Siqueira EB, Holler AP, Fabrício L, Skare TL. Periungual capillaroscopy in psoriasis. Anais brasileiros de dermatologia. 2012 Jul-Aug:87(4):550-3
[PubMed PMID: 22892767]
[83]
Ohtsuka T, Yamakage A, Miyachi Y. Statistical definition of nailfold capillary pattern in patients with psoriasis. International journal of dermatology. 1994 Nov:33(11):779-82
[PubMed PMID: 7822081]
[84]
Rajaei A, Dehghan P, Amiri A. Nailfold capillaroscopy in 430 patients with rheumatoid arthritis. Caspian journal of internal medicine. 2017 Fall:8(4):269-274. doi: 10.22088/cjim.8.4.269. Epub
[PubMed PMID: 29201317]
[85]
Altomonte L, Zoli A, Galossi A, Mirone L, Tulli A, Martone FR, Morini P, Laraia P, Magarò M. Microvascular capillaroscopic abnormalities in rheumatoid arthritis patients. Clinical and experimental rheumatology. 1995 Jan-Feb:13(1):83-6
[PubMed PMID: 7774109]
[86]
Nakamura R, Broce AA, Palencia DP, Ortiz NI, Leverone A. Dermatoscopy of nail lichen planus. International journal of dermatology. 2013 Jun:52(6):684-7. doi: 10.1111/j.1365-4632.2011.05283.x. Epub 2013 Feb 22
[PubMed PMID: 23432149]
[87]
Friedman P, Sabban EC, Marcucci C, Peralta R, Cabo H. Dermoscopic findings in different clinical variants of lichen planus. Is dermoscopy useful? Dermatology practical & conceptual. 2015 Oct:5(4):51-5. doi: 10.5826/dpc.0504a13. Epub 2015 Oct 31
[PubMed PMID: 26693092]
[88]
Nakamura RC, Costa MC. Dermatoscopic findings in the most frequent onychopathies: descriptive analysis of 500 cases. International journal of dermatology. 2012 Apr:51(4):483-5. doi: 10.1111/j.1365-4632.2010.04720.x. Epub
[PubMed PMID: 22435443]
Level 3 (low-level) evidence
[89]
McGill NW, Gow PJ. Nailfold capillaroscopy: a blinded study of its discriminatory value in scleroderma, systemic lupus erythematosus, and rheumatoid arthritis. Australian and New Zealand journal of medicine. 1986 Aug:16(4):457-60
[PubMed PMID: 3467690]
[90]
Cutolo M, Sulli A, Pizzorni C, Accardo S. Nailfold videocapillaroscopy assessment of microvascular damage in systemic sclerosis. The Journal of rheumatology. 2000 Jan:27(1):155-60
[PubMed PMID: 10648032]
[91]
Herrick AL, Cutolo M. Clinical implications from capillaroscopic analysis in patients with Raynaud's phenomenon and systemic sclerosis. Arthritis and rheumatism. 2010 Sep:62(9):2595-604. doi: 10.1002/art.27543. Epub
[PubMed PMID: 20506306]
[92]
Bergman R, Sharony L, Schapira D, Nahir MA, Balbir-Gurman A. The handheld dermatoscope as a nail-fold capillaroscopic instrument. Archives of dermatology. 2003 Aug:139(8):1027-30
[PubMed PMID: 12925391]
[93]
Tani C, Carli L, Vagnani S, Talarico R, Baldini C, Mosca M, Bombardieri S. The diagnosis and classification of mixed connective tissue disease. Journal of autoimmunity. 2014 Feb-Mar:48-49():46-9. doi: 10.1016/j.jaut.2014.01.008. Epub 2014 Jan 22
[PubMed PMID: 24461387]
[94]
Statham BN, Rowell NR. Quantification of the nail fold capillary abnormalities in systemic sclerosis and Raynaud's syndrome. Acta dermato-venereologica. 1986:66(2):139-43
[PubMed PMID: 2424237]
[95]
Shenavandeh S, Zarei Nezhad M. Association of nailfold capillary changes with disease activity, clinical and laboratory findings in patients with dermatomyositis. Medical journal of the Islamic Republic of Iran. 2015:29():233
[PubMed PMID: 26793626]
[96]
Lee P, Leung FY, Alderdice C, Armstrong SK. Nailfold capillary microscopy in the connective tissue diseases: a semiquantitative assessment. The Journal of rheumatology. 1983 Dec:10(6):930-8
[PubMed PMID: 6663597]
[97]
Manfredi A, Sebastiani M, Cassone G, Pipitone N, Giuggioli D, Colaci M, Salvarani C, Ferri C. Nailfold capillaroscopic changes in dermatomyositis and polymyositis. Clinical rheumatology. 2015 Feb:34(2):279-84. doi: 10.1007/s10067-014-2795-8. Epub 2014 Oct 17
[PubMed PMID: 25318613]
[98]
Tosti A, Schneider SL, Ramirez-Quizon MN, Zaiac M, Miteva M. Clinical, dermoscopic, and pathologic features of onychopapilloma: A review of 47 cases. Journal of the American Academy of Dermatology. 2016 Mar:74(3):521-6. doi: 10.1016/j.jaad.2015.08.053. Epub 2015 Oct 27
[PubMed PMID: 26518173]
Level 3 (low-level) evidence
[99]
Duarte AF, Correia O, Barreiros H, Haneke E. Giant subungual glomus tumor: clinical, dermoscopy, imagiologic and surgery details. Dermatology online journal. 2016 Oct 15:22(10):. pii: 13030/qt66f7b8wt. Epub 2016 Oct 15
[PubMed PMID: 28329592]
[100]
Mutsaers ER, Genders R, van Es N, Kukutsch N. Dermoscopy of glomus tumor: More white than pink. Journal of the American Academy of Dermatology. 2016 Jul:75(1):e17-8. doi: 10.1016/j.jaad.2016.01.049. Epub
[PubMed PMID: 27317535]
[101]
Kallis P, Miteva M, Patel T, Zaiac M, Tosti A. Onychomatricoma with Concomitant Subungual Glomus Tumor. Skin appendage disorders. 2015 Mar:1(1):14-7. doi: 10.1159/000371582. Epub 2015 Feb 3
[PubMed PMID: 27172169]
[102]
Ekin A, Ozkan M, Kabaklioglu T. Subungual glomus tumours: a different approach to diagnosis and treatment. Journal of hand surgery (Edinburgh, Scotland). 1997 Apr:22(2):228-9
[PubMed PMID: 9149994]
[103]
Thatte SS, Chikhalkar SB, Khopkar US. "Pink glow": A new sign for the diagnosis of glomus tumor on ultraviolet light dermoscopy. Indian dermatology online journal. 2015 Dec:6(Suppl 1):S21-3. doi: 10.4103/2229-5178.171041. Epub
[PubMed PMID: 26904443]
[104]
Lesort C, Debarbieux S, Duru G, Dalle S, Poulhalon N, Thomas L. Dermoscopic Features of Onychomatricoma: A Study of 34 Cases. Dermatology (Basel, Switzerland). 2015:231(2):177-83. doi: 10.1159/000431315. Epub 2015 Jun 20
[PubMed PMID: 26111574]
Level 3 (low-level) evidence
[105]
Ginoux E, Perier Muzet M, Poulalhon N, Debarbieux S, Dalle S, Thomas L. Intraoperative dermoscopic features of onychomatricoma: a review of 10 cases. Clinical and experimental dermatology. 2017 Jun:42(4):395-399. doi: 10.1111/ced.13077. Epub 2017 Feb 28
[PubMed PMID: 28244123]
Level 3 (low-level) evidence
[106]
Jha AK, Sonthalia S, Khopkar U. Dermoscopy of Pyogenic Granuloma. Indian dermatology online journal. 2017 Nov-Dec:8(6):523-524. doi: 10.4103/idoj.IDOJ_389_16. Epub
[PubMed PMID: 29204415]
[107]
Zaballos P, Rodero J, Serrano P, Cuellar F, Guionnet N, Vives JM. Pyogenic granuloma clinically and dermoscopically mimicking pigmented melanoma. Dermatology online journal. 2009 Oct 15:15(10):10
[PubMed PMID: 19951628]
[108]
Maddy AJ, Tosti A. Dermoscopic features of onychotillomania: A study of 36 cases. Journal of the American Academy of Dermatology. 2018 Oct:79(4):702-705. doi: 10.1016/j.jaad.2018.04.015. Epub 2018 Apr 14
[PubMed PMID: 29660424]
Level 3 (low-level) evidence
[109]
Halteh P, Scher RK, Lipner SR. Onychotillomania: Diagnosis and Management. American journal of clinical dermatology. 2017 Dec:18(6):763-770. doi: 10.1007/s40257-017-0289-6. Epub
[PubMed PMID: 28488241]
[110]
Ning AY, Levoska MA, Zheng DX, Carroll BT, Wong CY. Treatment Options and Outcomes for Squamous Cell Carcinoma of the Nail Unit: A Systematic Review. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2022 Mar 1:48(3):267-273. doi: 10.1097/DSS.0000000000003319. Epub
[PubMed PMID: 34889218]
Level 1 (high-level) evidence