[1]
Mesulam MM. Slowly progressive aphasia without generalized dementia. Annals of neurology. 1982 Jun:11(6):592-8
[PubMed PMID: 7114808]
[2]
Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, Ogar JM, Rohrer JD, Black S, Boeve BF, Manes F, Dronkers NF, Vandenberghe R, Rascovsky K, Patterson K, Miller BL, Knopman DS, Hodges JR, Mesulam MM, Grossman M. Classification of primary progressive aphasia and its variants. Neurology. 2011 Mar 15:76(11):1006-14. doi: 10.1212/WNL.0b013e31821103e6. Epub 2011 Feb 16
[PubMed PMID: 21325651]
[3]
Rogalski E, Mesulam M. An update on primary progressive aphasia. Current neurology and neuroscience reports. 2007 Sep:7(5):388-92
[PubMed PMID: 17764628]
[4]
Habib M, Pelletier J, Khalil R. [Primary progressive aphasia (Mesulam syndrome)]. Presse medicale (Paris, France : 1983). 1993 May 1-8:22(16):757-64
[PubMed PMID: 8316530]
[5]
Bonner MF, Ash S, Grossman M. The new classification of primary progressive aphasia into semantic, logopenic, or nonfluent/agrammatic variants. Current neurology and neuroscience reports. 2010 Nov:10(6):484-90. doi: 10.1007/s11910-010-0140-4. Epub
[PubMed PMID: 20809401]
[6]
Botha H, Josephs KA. Primary Progressive Aphasias and Apraxia of Speech. Continuum (Minneapolis, Minn.). 2019 Feb:25(1):101-127. doi: 10.1212/CON.0000000000000699. Epub
[PubMed PMID: 30707189]
[7]
Ulugut H, Pijnenburg YAL. Frontotemporal dementia: Past, present, and future. Alzheimer's & dementia : the journal of the Alzheimer's Association. 2023 Nov:19(11):5253-5263. doi: 10.1002/alz.13363. Epub 2023 Jun 28
[PubMed PMID: 37379561]
[8]
Chu M, Jiang D, Li D, Yan S, Liu L, Nan H, Wang Y, Wang Y, Yue A, Ren L, Chen K, Rosa-Neto P, Lu J, Wu L. Atrophy network mapping of clinical subtypes and main symptoms in frontotemporal dementia. Brain : a journal of neurology. 2024 Mar 1:():. pii: awae067. doi: 10.1093/brain/awae067. Epub 2024 Mar 1
[PubMed PMID: 38426222]
[9]
Spinelli EG, Mandelli ML, Miller ZA, Santos-Santos MA, Wilson SM, Agosta F, Grinberg LT, Huang EJ, Trojanowski JQ, Meyer M, Henry ML, Comi G, Rabinovici G, Rosen HJ, Filippi M, Miller BL, Seeley WW, Gorno-Tempini ML. Typical and atypical pathology in primary progressive aphasia variants. Annals of neurology. 2017 Mar:81(3):430-443. doi: 10.1002/ana.24885. Epub 2017 Mar 20
[PubMed PMID: 28133816]
[10]
Josephs KA, Hodges JR, Snowden JS, Mackenzie IR, Neumann M, Mann DM, Dickson DW. Neuropathological background of phenotypical variability in frontotemporal dementia. Acta neuropathologica. 2011 Aug:122(2):137-53. doi: 10.1007/s00401-011-0839-6. Epub 2011 May 26
[PubMed PMID: 21614463]
[11]
Chare L, Hodges JR, Leyton CE, McGinley C, Tan RH, Kril JJ, Halliday GM. New criteria for frontotemporal dementia syndromes: clinical and pathological diagnostic implications. Journal of neurology, neurosurgery, and psychiatry. 2014 Aug:85(8):865-70. doi: 10.1136/jnnp-2013-306948. Epub 2014 Jan 13
[PubMed PMID: 24421286]
[12]
Cioffi SM, Galimberti D, Barocco F, Spallazzi M, Fenoglio C, Serpente M, Arcaro M, Gardini S, Scarpini E, Caffarra P. Non Fluent Variant of Primary Progressive Aphasia Due to the Novel GRN g.9543delA(IVS3-2delA) Mutation. Journal of Alzheimer's disease : JAD. 2016 Sep 6:54(2):717-21. doi: 10.3233/JAD-160185. Epub
[PubMed PMID: 27567822]
[13]
Grossman M. The non-fluent/agrammatic variant of primary progressive aphasia. The Lancet. Neurology. 2012 Jun:11(6):545-55. doi: 10.1016/S1474-4422(12)70099-6. Epub 2012 May 16
[PubMed PMID: 22608668]
[14]
Mesulam M, Johnson N, Krefft TA, Gass JM, Cannon AD, Adamson JL, Bigio EH, Weintraub S, Dickson DW, Hutton ML, Graff-Radford NR. Progranulin mutations in primary progressive aphasia: the PPA1 and PPA3 families. Archives of neurology. 2007 Jan:64(1):43-7
[PubMed PMID: 17210807]
[15]
Clark DG, Charuvastra A, Miller BL, Shapira JS, Mendez MF. Fluent versus nonfluent primary progressive aphasia: a comparison of clinical and functional neuroimaging features. Brain and language. 2005 Jul:94(1):54-60
[PubMed PMID: 15896383]
[16]
Santos-Santos MA, Rabinovici GD, Iaccarino L, Ayakta N, Tammewar G, Lobach I, Henry ML, Hubbard I, Mandelli ML, Spinelli E, Miller ZA, Pressman PS, O'Neil JP, Ghosh P, Lazaris A, Meyer M, Watson C, Yoon SJ, Rosen HJ, Grinberg L, Seeley WW, Miller BL, Jagust WJ, Gorno-Tempini ML. Rates of Amyloid Imaging Positivity in Patients With Primary Progressive Aphasia. JAMA neurology. 2018 Mar 1:75(3):342-352. doi: 10.1001/jamaneurol.2017.4309. Epub
[PubMed PMID: 29309493]
[17]
Teichmann M, Migliaccio R, Kas A, Dubois B. Logopenic progressive aphasia beyond Alzheimer's--an evolution towards dementia with Lewy bodies. Journal of neurology, neurosurgery, and psychiatry. 2013 Jan:84(1):113-4. doi: 10.1136/jnnp-2012-302638. Epub 2012 Sep 11
[PubMed PMID: 22967721]
[18]
Bekkhus-Wetterberg P, Brækhus A, Müller EG, Norvik MI, Winsnes IE, Wyller TB. Primary progressive aphasia. Tidsskrift for den Norske laegeforening : tidsskrift for praktisk medicin, ny raekke. 2022 Nov 22:142(17):. doi: 10.4045/tidsskr.22.0100. Epub 2022 Nov 21
[PubMed PMID: 36416646]
[19]
Mouton A, Plonka A, Fabre R, Tran TM, Robert P, Macoir J, Manera V, Gros A. The course of primary progressive aphasia diagnosis: a cross-sectional study. Alzheimer's research & therapy. 2022 May 10:14(1):64. doi: 10.1186/s13195-022-01007-6. Epub 2022 May 10
[PubMed PMID: 35538502]
Level 2 (mid-level) evidence
[20]
Pengo M, Alberici A, Libri I, Benussi A, Gadola Y, Ashton NJ, Zetterberg H, Blennow K, Borroni B. Sex influences clinical phenotype in frontotemporal dementia. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2022 Sep:43(9):5281-5287. doi: 10.1007/s10072-022-06185-7. Epub 2022 Jun 8
[PubMed PMID: 35672480]
[21]
Marshall CR, Hardy CJD, Volkmer A, Russell LL, Bond RL, Fletcher PD, Clark CN, Mummery CJ, Schott JM, Rossor MN, Fox NC, Crutch SJ, Rohrer JD, Warren JD. Primary progressive aphasia: a clinical approach. Journal of neurology. 2018 Jun:265(6):1474-1490. doi: 10.1007/s00415-018-8762-6. Epub 2018 Feb 1
[PubMed PMID: 29392464]
[22]
Ogar JM, Dronkers NF, Brambati SM, Miller BL, Gorno-Tempini ML. Progressive nonfluent aphasia and its characteristic motor speech deficits. Alzheimer disease and associated disorders. 2007 Oct-Dec:21(4):S23-30
[PubMed PMID: 18090419]
[23]
Ash S, Evans E, O'Shea J, Powers J, Boller A, Weinberg D, Haley J, McMillan C, Irwin DJ, Rascovsky K, Grossman M. Differentiating primary progressive aphasias in a brief sample of connected speech. Neurology. 2013 Jul 23:81(4):329-36. doi: 10.1212/WNL.0b013e31829c5d0e. Epub 2013 Jun 21
[PubMed PMID: 23794681]
[24]
Ash S, McMillan C, Gunawardena D, Avants B, Morgan B, Khan A, Moore P, Gee J, Grossman M. Speech errors in progressive non-fluent aphasia. Brain and language. 2010 Apr:113(1):13-20. doi: 10.1016/j.bandl.2009.12.001. Epub 2010 Jan 13
[PubMed PMID: 20074786]
[25]
Wilson SM, Henry ML, Besbris M, Ogar JM, Dronkers NF, Jarrold W, Miller BL, Gorno-Tempini ML. Connected speech production in three variants of primary progressive aphasia. Brain : a journal of neurology. 2010 Jul:133(Pt 7):2069-88. doi: 10.1093/brain/awq129. Epub 2010 Jun 11
[PubMed PMID: 20542982]
[26]
Rosen HJ, Allison SC, Ogar JM, Amici S, Rose K, Dronkers N, Miller BL, Gorno-Tempini ML. Behavioral features in semantic dementia vs other forms of progressive aphasias. Neurology. 2006 Nov 28:67(10):1752-6
[PubMed PMID: 17130406]
[27]
Caine D, Breen N, Patterson K. Emergence and progression of 'non-semantic' deficits in semantic dementia. Cortex; a journal devoted to the study of the nervous system and behavior. 2009 Apr:45(4):483-94. doi: 10.1016/j.cortex.2007.07.005. Epub 2008 Feb 20
[PubMed PMID: 19231477]
[28]
Garrard P, Rentoumi V, Gesierich B, Miller B, Gorno-Tempini ML. Machine learning approaches to diagnosis and laterality effects in semantic dementia discourse. Cortex; a journal devoted to the study of the nervous system and behavior. 2014 Jun:55():122-9. doi: 10.1016/j.cortex.2013.05.008. Epub 2013 Jun 14
[PubMed PMID: 23876449]
[29]
Yi HA, Moore P, Grossman M. Reversal of the concreteness effect for verbs in patients with semantic dementia. Neuropsychology. 2007 Jan:21(1):9-19
[PubMed PMID: 17201526]
[30]
Irish M, Bunk S, Tu S, Kamminga J, Hodges JR, Hornberger M, Piguet O. Preservation of episodic memory in semantic dementia: The importance of regions beyond the medial temporal lobes. Neuropsychologia. 2016 Jan 29:81():50-60. doi: 10.1016/j.neuropsychologia.2015.12.005. Epub 2015 Dec 9
[PubMed PMID: 26683384]
[31]
Irish M, Hodges JR, Piguet O. Right anterior temporal lobe dysfunction underlies theory of mind impairments in semantic dementia. Brain : a journal of neurology. 2014 Apr:137(Pt 4):1241-53. doi: 10.1093/brain/awu003. Epub 2014 Feb 12
[PubMed PMID: 24523434]
[32]
Gorno-Tempini ML, Brambati SM, Ginex V, Ogar J, Dronkers NF, Marcone A, Perani D, Garibotto V, Cappa SF, Miller BL. The logopenic/phonological variant of primary progressive aphasia. Neurology. 2008 Oct 14:71(16):1227-34. doi: 10.1212/01.wnl.0000320506.79811.da. Epub 2008 Jul 16
[PubMed PMID: 18633132]
[33]
Leyton CE, Hsieh S, Mioshi E, Hodges JR. Cognitive decline in logopenic aphasia: more than losing words. Neurology. 2013 Mar 5:80(10):897-903. doi: 10.1212/WNL.0b013e318285c15b. Epub 2013 Feb 6
[PubMed PMID: 23390170]
[34]
Vinogradova OM, Serov VV, Sivakov AE. [Clinico-morphologic characteristics of periodic disease]. Arkhiv patologii. 1975:37(2):70-5
[PubMed PMID: 1131061]
[35]
Henry ML, Grasso SM. Assessment of Individuals with Primary Progressive Aphasia. Seminars in speech and language. 2018 Jul:39(3):231-241. doi: 10.1055/s-0038-1660782. Epub 2018 Jun 22
[PubMed PMID: 29933490]
[36]
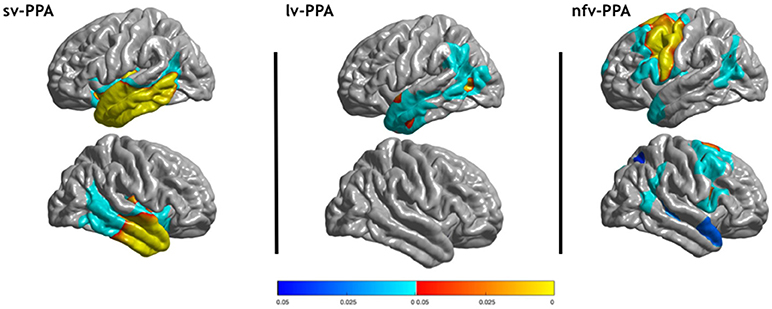
Mandelli ML, Vilaplana E, Brown JA, Hubbard HI, Binney RJ, Attygalle S, Santos-Santos MA, Miller ZA, Pakvasa M, Henry ML, Rosen HJ, Henry RG, Rabinovici GD, Miller BL, Seeley WW, Gorno-Tempini ML. Healthy brain connectivity predicts atrophy progression in non-fluent variant of primary progressive aphasia. Brain : a journal of neurology. 2016 Oct:139(Pt 10):2778-2791
[PubMed PMID: 27497488]
[37]
Mandelli ML, Vitali P, Santos M, Henry M, Gola K, Rosenberg L, Dronkers N, Miller B, Seeley WW, Gorno-Tempini ML. Two insular regions are differentially involved in behavioral variant FTD and nonfluent/agrammatic variant PPA. Cortex; a journal devoted to the study of the nervous system and behavior. 2016 Jan:74():149-57. doi: 10.1016/j.cortex.2015.10.012. Epub 2015 Nov 14
[PubMed PMID: 26673947]
[38]
Mandelli ML, Caverzasi E, Binney RJ, Henry ML, Lobach I, Block N, Amirbekian B, Dronkers N, Miller BL, Henry RG, Gorno-Tempini ML. Frontal white matter tracts sustaining speech production in primary progressive aphasia. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2014 Jul 16:34(29):9754-67. doi: 10.1523/JNEUROSCI.3464-13.2014. Epub
[PubMed PMID: 25031413]
[39]
Galton CJ, Patterson K, Graham K, Lambon-Ralph MA, Williams G, Antoun N, Sahakian BJ, Hodges JR. Differing patterns of temporal atrophy in Alzheimer's disease and semantic dementia. Neurology. 2001 Jul 24:57(2):216-25
[PubMed PMID: 11468305]
[40]
Yang J, Pan P, Song W, Shang HF. Quantitative meta-analysis of gray matter abnormalities in semantic dementia. Journal of Alzheimer's disease : JAD. 2012:31(4):827-33. doi: 10.3233/JAD-2012-120736. Epub
[PubMed PMID: 22699847]
Level 1 (high-level) evidence
[41]
Gorno-Tempini ML, Murray RC, Rankin KP, Weiner MW, Miller BL. Clinical, cognitive and anatomical evolution from nonfluent progressive aphasia to corticobasal syndrome: a case report. Neurocase. 2004 Dec:10(6):426-36
[PubMed PMID: 15788282]
Level 3 (low-level) evidence
[42]
Gorno-Tempini ML, Dronkers NF, Rankin KP, Ogar JM, Phengrasamy L, Rosen HJ, Johnson JK, Weiner MW, Miller BL. Cognition and anatomy in three variants of primary progressive aphasia. Annals of neurology. 2004 Mar:55(3):335-46
[PubMed PMID: 14991811]
[43]
Migliaccio R, Agosta F, Rascovsky K, Karydas A, Bonasera S, Rabinovici GD, Miller BL, Gorno-Tempini ML. Clinical syndromes associated with posterior atrophy: early age at onset AD spectrum. Neurology. 2009 Nov 10:73(19):1571-8. doi: 10.1212/WNL.0b013e3181c0d427. Epub
[PubMed PMID: 19901249]
[44]
Cadório I, Lousada M, Martins P, Figueiredo D. Generalization and maintenance of treatment gains in primary progressive aphasia (PPA): a systematic review. International journal of language & communication disorders. 2017 Sep:52(5):543-560. doi: 10.1111/1460-6984.12310. Epub 2017 Jan 24
[PubMed PMID: 28120406]
Level 1 (high-level) evidence
[45]
Tippett DC, Hillis AE, Tsapkini K. Treatment of Primary Progressive Aphasia. Current treatment options in neurology. 2015 Aug:17(8):362. doi: 10.1007/s11940-015-0362-5. Epub
[PubMed PMID: 26062526]
[46]
Mesulam MM. Primary progressive aphasia--differentiation from Alzheimer's disease. Annals of neurology. 1987 Oct:22(4):533-4
[PubMed PMID: 3324947]
[47]
Tastevin M, Lavoie M, de la Sablonnière J, Carrier-Auclair J, Laforce R Jr. Survival in the Three Common Variants of Primary Progressive Aphasia: A Retrospective Study in a Tertiary Memory Clinic. Brain sciences. 2021 Aug 24:11(9):. doi: 10.3390/brainsci11091113. Epub 2021 Aug 24
[PubMed PMID: 34573135]
Level 2 (mid-level) evidence