[2]
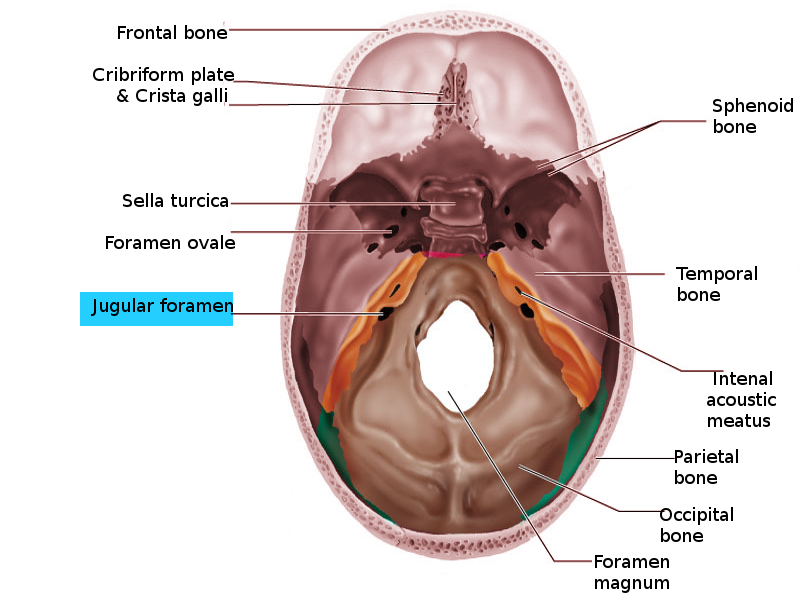
Caldemeyer KS, Mathews VP, Azzarelli B, Smith RR. The jugular foramen: a review of anatomy, masses, and imaging characteristics. Radiographics : a review publication of the Radiological Society of North America, Inc. 1997 Sep-Oct:17(5):1123-39
[PubMed PMID: 9308106]
[3]
Erol FS, Kaplan M, Kavakli A, Ozveren MF. Jugular foramen syndrome caused by choleastatoma. Clinical neurology and neurosurgery. 2005 Jun:107(4):342-6
[PubMed PMID: 15885397]
[4]
Lee M, Heo Y, Kim T. Vernet's Syndrome Associated with Internal Jugular Vein Thrombosis. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2019 Feb:28(2):344-346. doi: 10.1016/j.jstrokecerebrovasdis.2018.10.008. Epub 2018 Nov 2
[PubMed PMID: 30396840]
[5]
Amano M, Ishikawa E, Kujiraoka Y, Watanabe S, Ashizawa K, Oguni E, Saito A, Nakai Y, Ikeda H, Abe T, Uekusa Y, Matsumura A. Vernet's syndrome caused by large mycotic aneurysm of the extracranial internal carotid artery after acute otitis media--case report. Neurologia medico-chirurgica. 2010 Jan:50(1):45-8
[PubMed PMID: 20098025]
Level 3 (low-level) evidence
[6]
Cherin P, De Gennes C, Bletry O, Lamas A, Launay M, Dubs A, Godeau P. Ischemic Vernet's syndrome in giant cell arteritis: first two cases. The American journal of medicine. 1992 Sep:93(3):349-52
[PubMed PMID: 1524092]
Level 3 (low-level) evidence
[7]
Ferreira J,Franco A,Teodoro T,Coelho M,Albuquerque L, Vernet syndrome resulting from varicella zoster virus infection-a very rare clinical presentation of a common viral infection. Journal of neurovirology. 2018 Jun;
[PubMed PMID: 29532442]
[8]
Ono N,Sakabe A,Nakajima M, [Herpes zoster oticus-associated jugular foramen syndrome]. Brain and nerve = Shinkei kenkyu no shinpo. 2010 Jan;
[PubMed PMID: 20112795]
[9]
Thomasen I, Peitersen E, Peitersen B. [Parapharyngeal abscess complicated by the jugular foramen syndrome. Report of a child aged 2]. Ugeskrift for laeger. 1987 Jul 20:149(30):2023
[PubMed PMID: 3433427]
[10]
Dqbrowska A, Jałowiński R, Tarnowska C, Stankiewicz J, Deptuła-Jarosz M. [Paralysis of vocal fold as the first symptom of Vernet's syndrome in the course of jugular chemodectoma]. Otolaryngologia polska = The Polish otolaryngology. 2006:60(5):773-7
[PubMed PMID: 17263253]
[11]
Binns PM, Jugular foramen syndrome caused by meningioma. Transactions - American Academy of Ophthalmology and Otolaryngology. American Academy of Ophthalmology and Otolaryngology. 1972 Sep-Oct;
[PubMed PMID: 4666587]
[12]
Aghaghazvini L,Sedighi N,Karami P,Yeganeh O, Skull base aneurysmal bone cyst presented with foramen jugular syndrome and multi-osseous involvement. Iranian journal of radiology : a quarterly journal published by the Iranian Radiological Society. 2012 Sep;
[PubMed PMID: 23329983]
[13]
Rupa V, Rajshekhar V, Bhanu TS, Chandi SM. Primary chondroid chordoma of the base of the petrous temporal bone. The Journal of laryngology and otology. 1989 Aug:103(8):771-3
[PubMed PMID: 2769048]
[14]
Schweinfurth JM,Johnson JT,Weissman J, Jugular foramen syndrome as a complication of metastatic melanoma. American journal of otolaryngology. 1993 May-Jun;
[PubMed PMID: 8338200]
[15]
Alberio N,Cultrera F,Antonelli V,Servadei F, Isolated glossopharyngeal and vagus nerves palsy due to fracture involving the left jugular foramen. Acta neurochirurgica. 2005 Jul;
[PubMed PMID: 15891807]
[16]
Hayward D, Morgan C, Emami B, Biller J, Prabhu VC. Jugular foramen syndrome as initial presentation of metastatic lung cancer. Journal of neurological surgery reports. 2012 Oct:73(1):14-8. doi: 10.1055/s-0032-1301406. Epub 2012 Feb 17
[PubMed PMID: 23946920]
[17]
Greenberg HS, Deck MD, Vikram B, Chu FC, Posner JB. Metastasis to the base of the skull: clinical findings in 43 patients. Neurology. 1981 May:31(5):530-7
[PubMed PMID: 6972014]
[18]
Fayad JN, Keles B, Brackmann DE. Jugular foramen tumors: clinical characteristics and treatment outcomes. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2010 Feb:31(2):299-305. doi: 10.1097/MAO.0b013e3181be6495. Epub
[PubMed PMID: 19779386]
[19]
Ciavarro G,Bozzetti F,Falcioni M, Jugular Foramen Metastasis from Lung Cancer: A Case of
[PubMed PMID: 31257193]
Level 3 (low-level) evidence
[20]
Jo YR, Chung CW, Lee JS, Park HJ. Vernet syndrome by varicella-zoster virus. Annals of rehabilitation medicine. 2013 Jun:37(3):449-52. doi: 10.5535/arm.2013.37.3.449. Epub 2013 Jun 30
[PubMed PMID: 23869347]
[21]
Wilson M, Browne JD, Martin T, Geer C. Case report: atypical presentation of jugular foramen mass. American journal of otolaryngology. 2012 May-Jun:33(3):370-4. doi: 10.1016/j.amjoto.2011.10.006. Epub 2011 Dec 6
[PubMed PMID: 22154064]
Level 3 (low-level) evidence
[22]
Saman Y,Whitehead D,Gleeson M, Jugular foramen schwannoma presenting with glossopharyngeal neuralgia syncope syndrome. The Journal of laryngology and otology. 2010 Dec;
[PubMed PMID: 20602849]
[23]
Gandía-González ML, Kusak ME, Moreno NM, Sárraga JG, Rey G, Álvarez RM. Jugulotympanic paragangliomas treated with Gamma Knife radiosurgery: a single-center review of 58 cases. Journal of neurosurgery. 2014 Nov:121(5):1158-65. doi: 10.3171/2014.5.JNS131880. Epub 2014 Jun 13
[PubMed PMID: 24926654]
Level 3 (low-level) evidence