Continuing Education Activity
Nevus sebaceus of Jadassohn also referred to as organoid nevus, is a congenital malformation involving hamartomas of the pilosebaceous follicular unit. These growths most commonly form on the scalp, but may also appear on the forehead, face, or neck. They undergo a growth phase during puberty due to hormonal changes. In adulthood, the growths may develop secondary neoplasms within them, most commonly trichoblastoma. The treatment of these lesions is controversial, with options ranging from observation to early excision in childhood. This activity illustrates the evaluation and treatment of nevus sebaceus of Jadassohn and reviews the role of the interprofessional team in managing those with this condition.
Objectives:
- Identify the typical clinical appearance of nevus sebaceus of Jadassohn.
- Describe the evaluation of nevus sebaceus of Jadassohn.
- Review the management of nevus sebaceus of Jadassohn.
- Summarize a well-coordinated interprofessional team approach to provide effective care to patients affected by nevus sebaceus of Jadassohn.
Introduction
Nevus sebaceus of Jadassohn also referred to as organoid nevus, is a congenital malformation described in 1895 by the dermatologist Josef Jadassohn. These congenital malformations are hamartomas of the pilosebaceous follicular unit. These growths most commonly form on the scalp, but may also appear on the forehead, face, or neck. They undergo a growth phase during puberty due to hormonal changes in the patient's body. In adulthood, the growths may develop secondary neoplasms within them, most commonly trichoblastoma. The treatment of these lesions is controversial, with options ranging from observation to early excision in childhood.[1][2]
Features of the nevus sebaceus syndrome (also known as Schimmelpenning Feuerstein Mims syndrome) include a large or disseminated nevus sebaceus along with abnormalities of the central nervous, skeletal, or ocular systems.[3] A rare condition known as phakomatosis pigmentokeratotica (PPK) is a subclassification of the epidermal nevus syndrome, in which a patient exhibits both a nevus sebaceus and at least one speckled lentiginous nevus.
Etiology
Previously, it was thought that secondary carcinoma was a relatively common phenomenon to occur in nevus sebaceus. However, studies have since suggested that most secondary neoplasms that develop in adulthood have benign origins. Many speculate that the supposed malignant growths that arose in nevus sebaceus were previously misdiagnosed as basal cell carcinoma but were likely trichoblastomas, which can share a very similar histological appearance. The actual incidence of basal cell carcinoma in nevus sebaceus is less than 1%. Trichoblastoma is the most frequently occurring tumor in nevus sebaceus, followed by syringocystadenoma papilliferum. Other common secondary neoplasms include tricholemmoma, sebaceous adenoma, desmoplastic tricholemmoma, apocrine adenoma, and poroma.[4][5][6][7]
Epidemiology
Approximately 0.3% of newborns are affected by nevus sebaceus, and the incidence is equal between male and female patients. The disorder affects all races and ethnicities. Usually, nevus sebaceus appears as a solitary lesion at birth. Sometimes, it may not be identified until after puberty once its classical wart-like appearance has fully developed.
Pathophysiology
Nevus sebaceus is not an inherited skin lesion. It carries postzygotic somatic mutations of the Ras protein family, most commonly HRas. These Ras mutations are also present in commonly occurring secondary tumors of nevus sebaceus such as trichoblastomas.
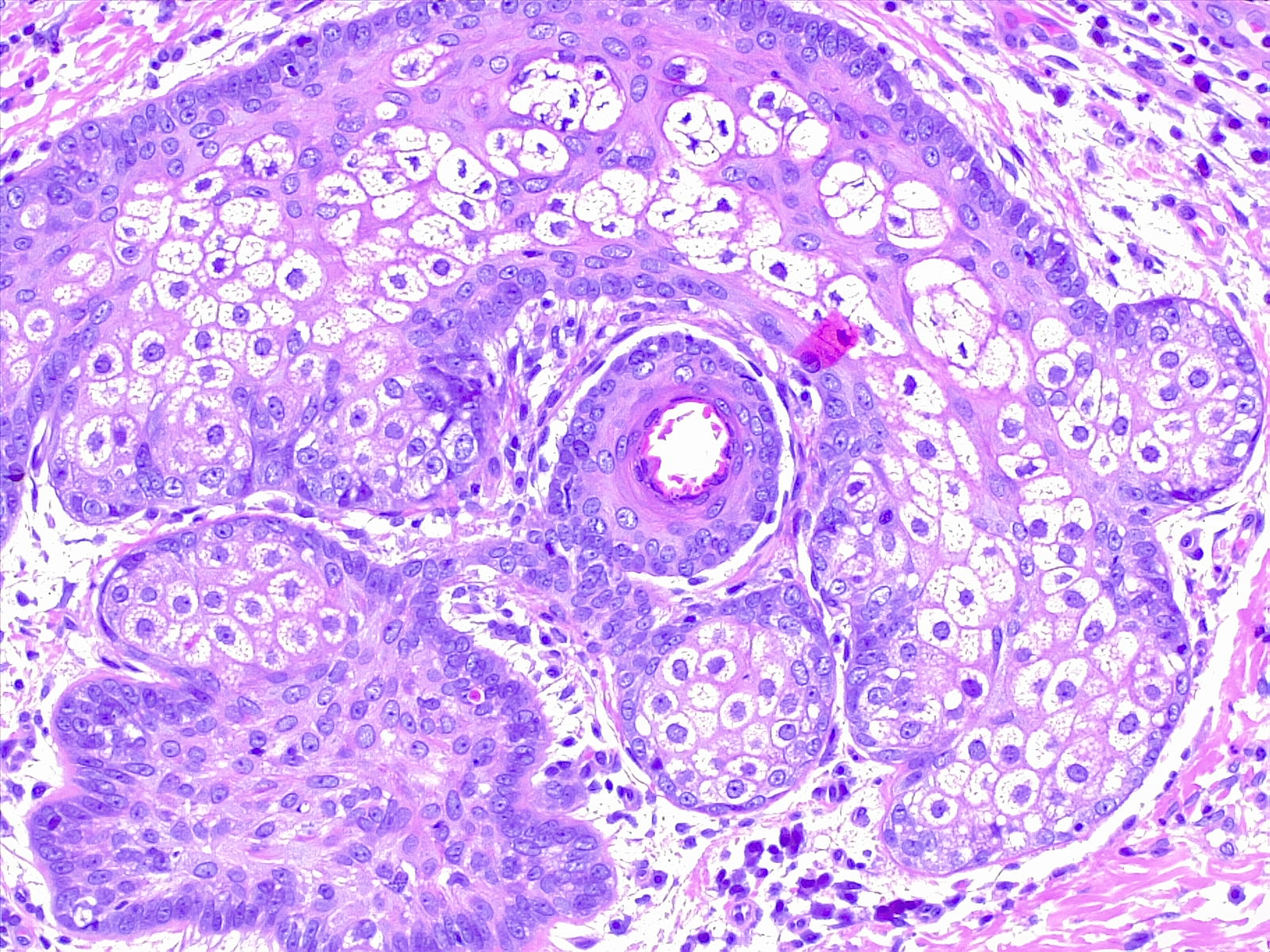
Histopathology
In infancy or early childhood, nevus sebaceus histologically features immature and abnormally formed pilosebaceous units. At this stage of development, epidermal changes may reveal some acanthosis and mild papillomatosis. During puberty, the lesions enlarge clinically as well as microscopically. The sebaceous glands become much more prominent and are located unusually high in the dermis. The number of sebaceous lobules and malformed ducts increases. The hair follicles are typically immature vellus hairs rather than terminal hairs. At this growth phase, the epidermis becomes more papillated and acanthotic. Some lesions may also demonstrate ectopic apocrine glands or eccrine hyperplasia.[8]
History and Physical
The lesions either appear at birth or shortly afterward. They initially present as a solitary smooth, yellow, well-circumscribed plaque with an oval or linear configuration. When multiple, lesions often arise along the lines of Blaschko. Nevus sebaceus is typically asymptomatic. In the scalp, they are classically associated with overlying partial or total alopecia. At puberty, nevus sebaceus becomes more prominent. It takes on a verrucous or mamillated appearance secondary to the hormonal changes of the child. This evolution mirrors the histologic differentiation of normal sebaceous glands of the skin. The patient or their parents may present to the dermatology clinic for evaluation and potential removal due to its clinical appearance.
Although additional extracutaneous findings would be exceedingly rare, a complete physical should be conducted looking for features such as a coloboma, corneal clouding, strabismus, spinal curvature, hip dislocation, or limb deformities. Consultation with an ophthalmologist or orthopedist should be requested; if any of these extracutaneous findings are present, a neurologist should also be consulted as the neurologic sequelae (such as seizures) may not be evident on physical examination.
Evaluation
Nevus sebaceus is a clinical diagnosis; additional workup is typically unnecessary. The exception would be a child with nevus sebaceus syndrome that presents with a large or multifocal lesion that may be associated with extracutaneous involvement of the ocular, skeletal, or central nervous systems. In this case, referral to neurology and other specialists may be indicated if other physical anomalies are present.
Treatment / Management
The management of nevus sebaceus remains a controversial topic. Because nevus sebaceus was previously thought to indicate a high risk for developing secondary carcinomas later in life, prophylactic excision was an acceptable treatment. However, research suggests the risk for developing secondary carcinomas is low, while the risk of developing secondary benign neoplasms is relatively high. Most secondary tumors arising in a nevus sebaceus occur in adults 40 years or older. Surgical excision is considered an acceptable treatment for nevus sebaceus as early as late childhood, once the risk from general anesthesia lessens or the patient is mature enough to tolerate the procedure with local anesthesia. Other factors to consider prior to surgery include the size and location of the lesion. Superficial procedures such as shave removal, dermabrasion, or laser resurfacing are typically unsuccessful as these do not remove the entire lesion.[5][9][10][11]
Differential Diagnosis
The differential diagnosis of nevus sebaceus depends on the stage of development. In early infancy, the differential diagnosis may include aplasia cutis congenita or mastocytoma. Other differential diagnoses in later stages of development include congenital nevus, epidermal nevus, seborrheic keratosis, verruca, and juvenile xanthogranuloma.
Prognosis
Generally, nevus sebaceus will follow a benign course. Rarely, the presence of a secondary malignancy or sequelae of the nevus sebaceus syndrome may portend a variable prognosis.
Complications
The risk of malignancy is minimal and almost nonexistent in children. Besides the development of a basal cell carcinoma, other secondary malignant tumors may very rarely occur and include sebaceous carcinoma, squamous cell carcinoma, microcystic adnexal carcinoma, and melanoma.
Deterrence and Patient Education
Patients should be taught that nevus sebaceus is typically a benign lesion that may present as a warty plaque on the scalp when fully developed. The patient should be advised that an associated malignancy is very rare and would be more likely to present in adulthood. All patients should be asked to see a clinician when there are changes in the color, texture, size, or accompanying symptoms of the lesion.
Enhancing Healthcare Team Outcomes
As the nevus sebaceus tends to appear in infancy, it may be first evaluated by a pediatric primary care provider, such as a physician or nurse practitioner. When a lesion is in its early stage (smooth) and small, reassurance is appropriate. If the lesion is of significant cosmetic concern, or if it appears that a secondary neoplasm has developed within the nevus sebaceus, referral to a dermatologist is warranted. A biopsy or excision may be performed if indicated. When the nevus sebaceus is very large, and reconstruction may be highly complex and involve tissue expansion, for example, a referral to a plastic surgeon should be considered. If there are any of the aforementioned extracutaneous features present on physical examination, a referral to neurology is appropriate to investigate other central nervous system conditions that may manifest as a part of the nevus sebaceus syndrome. Other subspecialists such as an orthopedist or ophthalmologist may be consulted as indicated. The subspecialists should report any relevant diagnoses and recommendations to the primary care provider when longitudinal follow-up is needed.