Structure
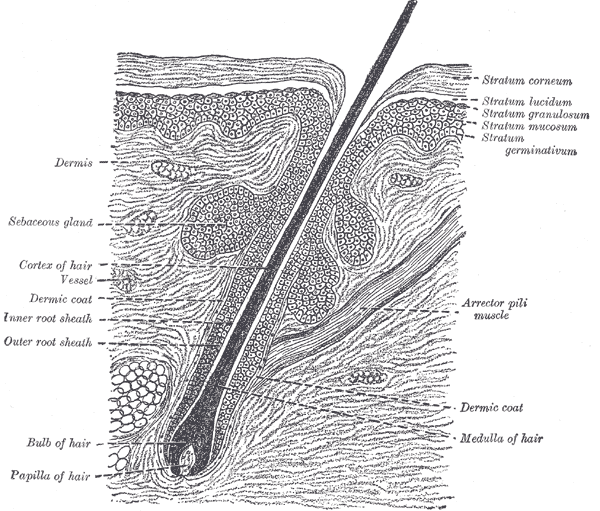
The skin appendages include sweat glands, nails, and the pilosebaceous unit of the skin, comprised of the hair shaft, hair follicle, sebaceous gland, and arrector pili muscle — these appendages derive from a down growth of the epidermis beginning in the third month of fetal life.
The pilosebaceous unit is found in nearly all regions of the skin except for the lips, palmar and plantar surfaces, and is most dense on the scalp.
Hair Structure
The hair structure divides into the hair shaft and hair follicle.
The hair shaft is the portion of the hair that is visible on the outside of the skin. It is made up of cuticle cells that surround the cortex, with a central medulla present in thicker hair. The cortical layer provides the bulk of the hair shaft structure and is comprised of keratin.
The hair follicle is the primary structure for hair growth and divided into three segments:
- Infundibulum
- Isthmus
- Inferior segment
The infundibulum comprises the portion from the epidermal invagination to the level of the ductal opening of the sebaceous gland. The isthmus is the portion from the opening of the sebaceous gland to the insertion of the arrector pili muscle. The bulge area, where stem cells are thought to reside, is located between the ductal opening of the sebaceous gland and the insertion of the arrector pili muscle. The inferior segment is the growing portion of the follicle and, at its base, expands to form the bulb, which is invaginated by a tuft of vascularized loose connective tissue called the dermal papilla, which actively produces hair. The hair bulb contains matrix cells that function to promote the growth of the hair follicle, allowing hair to grow longer. The dermal papilla is surrounded by a dermal sheath that contains progenitor cells that function to regenerate the dermal papilla and participate in wound healing. These regenerative and proliferating regions define the hair cycle, which comes in phases known as anagen, catagen, and telogen (growth, regression, rest).
The hair follicle is further divided histologically into the inner root sheath and outer root sheath.
The Outer Root Sheath encloses the inner root sheath and is continuous with the epidermis. This layer contains multipotent stem cells, melanocytes, and keratinocytes. The melanocytes are pigment (melanin) producing cells that originate from the neural crest and contribute to the color of hair, and keratinocytes are keratin producing cells.
The Inner Root Sheath further divides into the Henle layer, Huxley layer, and the cuticle. This layer only extends up to the level of where the sebaceous gland meets the hair follicle.
- Henley's layer: outermost layer made of cuboidal cells in direct contact with the outer root sheath
- Huxley's layer: the second and middle layer made of two rows of flattened cells that contain granular protoplasm
- Cuticle: the third, innermost layer made of flat overlapping squamous cells that is continuous with the outermost layer of the hair fiber
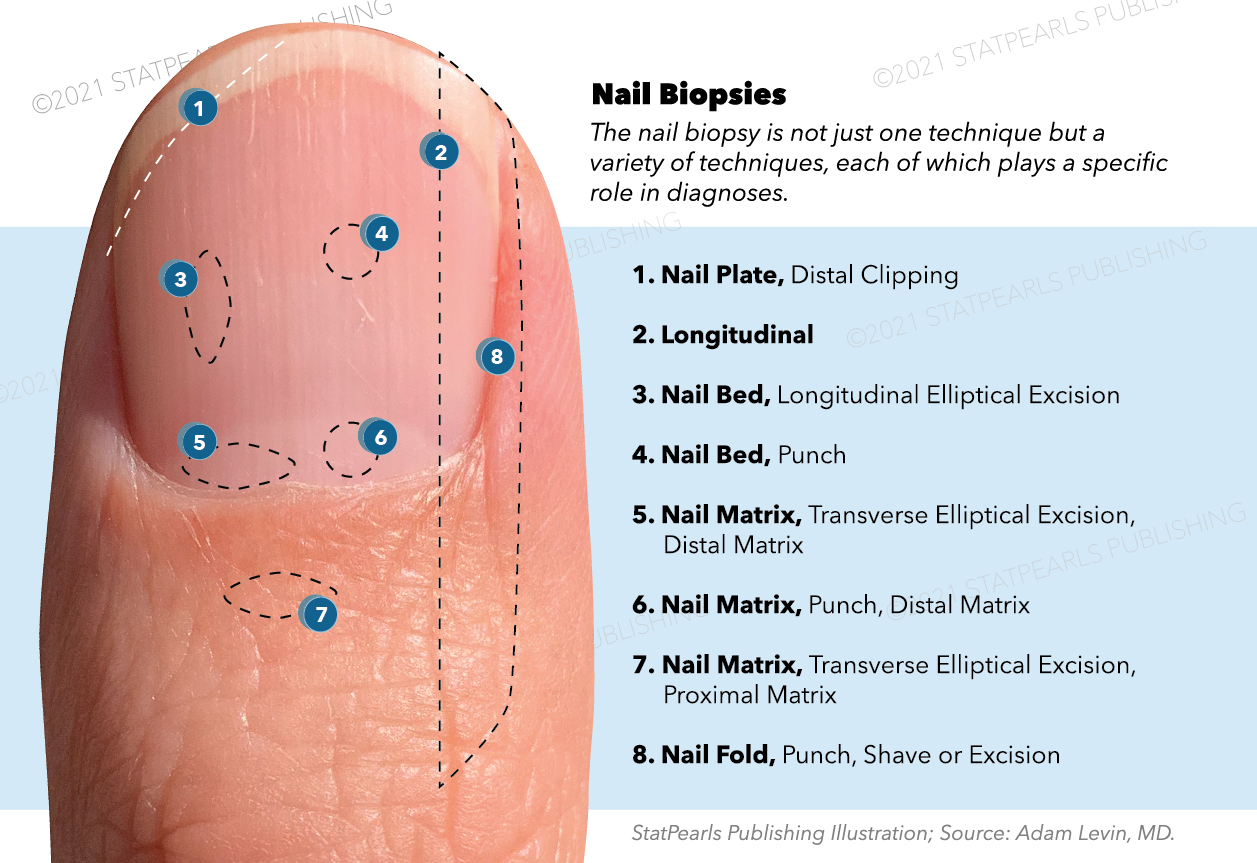
Nail Structure
The nail unit includes the nail plate, eponychium, hyponychium, nail folds, lunula, and nail matrix. The prefix onycho- pertains to the nails.
The nail matrix lacks a granular layer, has a thick stratified squamous epithelium, long rete ridges, and contains melanocytes, epithelial cells, Merkel cells, stem cells, and Langerhans's cells. It is also known as the germinative zone where stem cells divide, migrate, differentiate, and produce keratin for the formation of the nail. At the edge of the lunula, as the epithelium transitions to the nail bed, the epithelium thins.
The nail plate is the visible portion of the nail that is rigid and composed of compact keratinocytes called onychocytes, which are flatter than the corneocytes found in the skin, and do not desquamate. The nail plate is curved and fits tightly into the proximal and lateral nail folds. Histologically, the nail plate is comprised of anucleate keratinocytes and contributes to the translucency of the nail plate. Though the nail plate resembles the stratum corneum of the skin, it has a lower percentage of fat and water and a higher percentage of the amino acid cysteine resulting in strong disulfide bond formation, contributing to its strength.
The hyponychium (nail bed) is the portion of the skin beneath the nail plate and spans from the lunula to the hyponychium. Histologically, its epithelium lacks a stratum granulosum but contains a spinous layer and a monocellular basal layer. It consists of epithelial cells that are continuous with the stratum spinosum and basal, with the nail plate serving as the stratum corneum. The deeper portion of the nail bed is made up of a uniform compartment of collagen bundles and elastic fibers with a rich vascular network. Arteriovenous anastomoses involved in thermoregulation, known as glomus bodies, are found in the dermal portion. The thickened portion at the interface between the hyponychium and the nail plate termed the onychodermal band, which serves as a barrier to pathogens.
The eponychium (cuticle) is the tissue overlapping the nail plate at the most proximal edge made of hard keratin that does not desquamate. Histologically, the epidermis is thin and resembles normal skin. The cuticle is also an important barrier to pathogens.
The lunula is a crescent-shaped white area near the nail root. The color arises from the thick, opaque layer of partially keratinized matrix cells.
Sebaceous Glands
Sebaceous glands are part of the pilosebaceous unit, and there are typically multiple sebaceous glands per hair follicle. Sebaceous glands are made up of lobules and ducts and true exocrine glands found in all areas of the skin except for the palms, soles, lip, and tops of the feet. The lobules are made up of sebocytes that produce sebum, a fatty material that lubricates hair and has bactericidal and fungicidal properties. These "oil glands" are also categorized as holocrine exocrine glands, which means that the entire sebocyte loses its cytoplasm and dies in the process of discharging its contents during the excretory process toward the middle of the gland into its lumen.
These glands are pear-shaped, and their duct, the pilosebaceous canal, opens into the neck (upper third) of the hair follicle. On microscopy, these glands have a foamy appearance because the lipid content is poorly staining.
Sweat Glands (Sudoriferous)
The sweat glands categorize as either eccrine and apocrine glands. Eccrine is the most common of the sweat glands, distributed all over the body except the lips and part of the external genitalia. Apocrine glands are limited to the axilla, areola, nipple, skin around the anus, and external genitalia and have an odor. These glands differ in their mode of secretion. Eccrine glands exhibit merocrine secretion meaning there is no loss of cellular cytoplasm during secretion, and apocrine glands lose a portion of the top of the cell cytoplasm with each apocrine secretion.
Eccrine
Histologically, the eccrine sweat glands are present in the dermis and upper portion of the hypodermis. There is a secretory portion and a duct portion.
The secretory portion appears coiled, with epithelial cells that stain both light (contain watery/electrolyte material) and dark (contain glycoprotein material) on hematoxylin & eosin stain and are either cuboidal or pyramidal in shape. The secretory tubule is surrounded by myoepithelial cells (smooth muscle-like) that contract to help with the secretory process. The myoepithelial cells are oriented obliquely and longitudinally around secretory portions of tubules. The secretory coil divides into the coiled segment, the straight segment that extends into the epidermis, and the intraepidermal segment, which appears between epithelial cells.
The excretory duct portion does not have myoepithelial cells and is lined by a double layer of cuboidal cells, containing microvilli. The basal cells are connected by the microvilli and contain opaque granules.
Apocrine
Histologically, the apocrine glands are not as coiled and found in the dermis and subcutaneous fat. Like the eccrine glands, the apocrine glands have a secretory and excretory duct portion. These glands are hormonally controlled and become active at puberty.
The secretory portion has a lining of simple cuboidal epithelial cells, and the lumen is much larger than that of the eccrine gland lumen. The cells of the secretory portion vary in size depending on the stage of secretion, and the contents are odorous oily, yellow, viscous secretions.
The excretory portion contains a body and an excretory duct that opens into the hair follicle. The body (tubulo-alveoli) is lined by cuboidal and columnar epithelial cells and surrounded by myoepithelial cells in a sac-shaped out pocket. The excretory duct lining is simple cuboidal epithelium. [4][5][6][7][8][9][10][11][12][13]
Function
Hair Function
Hair serves many functions, including protection, body temperature regulation, facilitation of perspiration, sensation, aesthetics, and psychosocial health. Hair protects our skin from UV radiation in areas that are more hair dense. Hair can retain heat when we are cold and stand on end with the contraction of arrector pili muscles, promoting heat loss through sweat production when we are hot. Hair can also contribute to tactile sensation by transmission through the hair follicles. Socially, hair can be a symbol of beauty and health, contributing to confidence in an individual's psychosocial well-being.
Nail Function
The functions of the finger and toenails include protection from injury and infection, help with grasping and manipulating objects, aesthetic and cosmetic purposes, augmentation of sensation. The sheer strength of the nail mediates protection as a direct result of keratinization and the preservation of the cuticle, onychodermal band, and lateral nail folds to prevent infection.
Sebaceous Gland Function
Sebaceous glands are essential for the secretion of sebum that serves to lubricate the skin and protect the skin against friction, but also contribute to the modulation of bacterial and fungal growth by the presence of triglycerides and proteolytic enzymes.
Sebum Secretion
The process of sebum secretion begins with the proliferation of cells at the basal layer (the secretory portion of the gland).
- Cells become pushed to the center of the gland towards the excretory duct.
- Fatty material is then formed and accumulates in the cytoplasm.
- Cells burst and die as they accumulate sebum and are pushed further from the basal layer.
- Sebum empties onto the hair.
- Contraction of arrector pili muscle can speed up secretion.
Sweat Gland Function
Eccrine (cholinergic sympathetic stimulation)
There are three main functions of the eccrine glands:
- Protection: by preserving the skin's acidic composition and protect from microbial overgrowth.
- Thermoregulation: the production of sweat that cools the skin surface and reduces body temperature.
- Excretion: by the excretion of water and electrolytes
Apocrine (adrenergic sympathetic stimulation)
The main functions of the apocrine glands are not fully known, but there is pheromone secretion through sweat, which may influence sexual attraction, secretion of lubricating material assisting with increased frictional resistance, and androgenic activity shown by the activity of 5α-reductase, and stimulation of function at puberty.[4][5][6][7][8][9][10][11][12][13]
Tissue Preparation
Skin Biopsy
Skin biopsy can be completed in multiple ways, including excisional biopsy, incisional biopsy, shave biopsy, punch biopsy, curetting, fine needle aspiration.
- An excisional biopsy: the entire lesion of interest is cut out.
- An incisional biopsy: a segment of a lesion is removed.
- A shave biopsy: a horizontal section is removed.
- A punch biopsy: a round specimen (2 to 6 mm in diameter) is removed, curetting fragments of tissue.
A fine-needle aspiration: drawn from the lesion for direct examination.
The biopsy type is chosen based on the type of lesion.
Following the skin biopsy, the sample must be placed in a fixative solution of neutral buffered formalin to preserve the tissue structure. In the laboratory, the sample is placed in formol saline for at least 24 hours before being processed.
The specimen is then placed in a small cassette initially in fixative, but later in paraffin blocks. The cassette is a support for the paraffin block and helps cut the tissue into thin sections. Alcohol dehydration to eliminate water from the preparation takes place by the use of an automated processor followed by clearance of the alcohol by using dimethyl benzene and allows the tissue to become incorporated in paraffin wax.
The tissue is removed from the cassette, put in a mold, and covered with hot liquid paraffin wax. When the wax cools, it becomes solid and forms the block for sectioning. Finally, the block is sectioned before being stained, typically with hematoxylin & eosin (H&E) with special stains later used if needed. Hematoxylin has bluish hues staining nucleic acids, and eosin will stain cytoplasmic components pink.
Hair and Nail Examination
Hair and nails may be studied in microscopy without performing a biopsy. Usually, a hair sample is collected by either clipping or plucking for microscopy, and clipping for nails. Clipping of hair is recommended when hair shaft disorders are suspected, while plucking is recommended when examination of the root is needed, as in alopecia areata and nails when infectious or immune-mediated conditions are suspected.
There are mainly two types of tissue preparation clinicians use.
- A dry mount: hair samples are put on a glass slide and covered with a coverslip.
- Wet mount: uses KOH for suspected fungal infection (hair and nails).[14]
Microscopy, Light
Light microscope examination serves to light and magnifies a specimen in the investigation of a variety of pathology. The examiner studies the specimen under light microscopy on a glass slide that was prepared, as stated above, in the tissue preparation section of this article.
Skin biopsy with histopathological examination may be indicated in suspected skin cancers, inflammatory conditions, and other potential pathological conditions of the skin appendages.
Nail plate biopsy followed by Periodic Acid Schiff stain may be useful in the diagnosis of onychomycosis (fungal nail infection) with a negative mycological examination. Nail biopsy may also be an option in inflammatory (like lichen planus) or tumoral changes.
Polarized light microscopy is done if anomalies of the hair shaft are suspected. Clinicians typically use dermoscopy (trichoscopy) in the clinical setting.[14][15]
Pathophysiology
There are many inflammatory, immune-mediated, autoimmune, infectious, neoplastic, and traumatic causes of alterations to the normal function of the skin appendages, some of which include the following:
Inflammatory and immune-mediated illnesses may result in damage to the hair follicle and can lead to permanent hair loss if the follicle scars. The follicles can become infected by various pathogens that lead to inflammation and pustule formation seen on the surface of the skin at the opening of the hair follicle. Endocrine-mediated illnesses like congenital adrenal hyperplasia, hypothyroidism, hyperthyroidism, and tumoral processes can affect hair growth and hair cycle.
Trauma to the nail matrix can result in altered growth or even permanent failure of growth. Infections in the nail matrix can also alter nail growth patterns and the appearance of the nail plate. Many nail changes can present, such as pitting, koilonychia, onycholysis, ridging, among others from vitamin and nutrient deficiencies, trauma to the nail unit, psoriasis, alopecia, and many more.
Sebaceous gland overactivity in conjunction with cutibacterium acnes overgrowth can cause acne or seborrheic dermatitis if there is an overgrowth of Malassezia furfur. Sebaceous glands can also become hyperplastic, form cysts, and undergo neoplastic changes.
Sweat glands can become overactive, as seen in hyperhidrosis, and can contribute to excessive malodor, as seen in bromhidrosis. Many chronic conditions can result if the sweat ducts are blocked, like miliaria rubra and Fox-Fordyce disease. They, too, can undergo neoplastic changes and form tumors.[13][16]