Continuing Education Activity
Peripheral nerve injuries frequently occur as a consequence of trauma. They may arise from various mechanisms, including laceration, contusion, stretching, compression, and iatrogenic injury. Although generally not life-threatening, they can significantly affect a patient's daily activities and overall quality of life. Restoration of nerve continuity will aid in functional recovery. Autologous nerve grafting is the gold standard treatment for the reconstruction of a nerve gap. The sural nerve is a valuable source for a nerve graft of good diameter and length, being the most common donor site utilized in current medical practice. This activity aims to describe in detail the surgical technique for sural nerve harvesting.
Objectives:
Summarize the indications and main clinical applications for the use of an autologous nerve graft.
Describe the pertinent anatomy of the sural nerve that will enable the reader to harvest the graft effectively and safely.
Outline the sural nerve graft open harvest technique in a step-by-step fashion and briefly report other harvesting methods.
Identify some interprofessional strategies that will benefit the patient when performing a sural nerve graft procedure.
Introduction
Peripheral nerve injuries frequently occur as a consequence of trauma. They may arise from various mechanisms, including laceration, contusion, stretching, compression, and iatrogenic injury. Although generally not life-threatening, they can significantly affect a patient's daily activities and overall quality of life. Restoration of nerve continuity will aid in functional recovery.
Primary end-to-end neurorrhaphy is the preferred technique for the repair of transected peripheral nerves. Unfortunately, it is not always possible to perform tension-free primary repair due to retraction of nerve stumps, scarring, or destruction of neural tissue; these may result in gaps that cannot be bridged without putting undue tension on the repairs or that cannot be bridged with the remaining tissue at all. Excessive tension across a nerve repair decreases perfusion at the neurorrhaphy site and may reduce the quality of the functional outcome.[1] In this situation, autologous nerve grafting plays a major role, with the sural nerve being a commonly selected donor.[2] Sural nerve harvesting was originally described as an open technique, but surgical technology improvements have led to the development of minimally invasive techniques over the last several years.[3][4][5]
The goal of peripheral nerve reconstruction with a nerve graft is to provide a scaffold that guides the regenerating axons towards the distal nerve stump and permits end-organ reinnervation. The graft also provides Schwann cells that aid in axonal regeneration. Nerve coaptation should be performed under magnification; localization of healthy proximal and distal stumps with a “bread-loafing” technique is preferred before nerve graft interposition, and a tension-free neurorrhaphy should be performed even under a full range of motion of the joint, if applicable. Careful fascicle orientation and alignment is critical to prevent axonal loss and obtain the best results.[2] Under optimal conditions, axonal regeneration within a graft will occur at a speed of 1 mm to 1.5 mm per day.[6]
Although surgical restoration of the nerve may improve the motor, sensory, and autonomic function of the end organ, reinnervation does not invariably produce complete functional recovery. Many factors, including the site of nerve disruption, the timing of reconstruction, the length of nerve gap, and patient characteristics like age and smoking status, will influence the final outcome.[7][8][9] Because it is difficult to optimize all of the variables that affect neural regeneration, complete functional recovery after nerve graft reconstruction remains the exception rather than the norm.
Anatomy and Physiology
The sural nerve is a purely sensory nerve composed of fibers from lumbosacral spinal roots L4-S1. Its origin is classically described as the union of the lateral and medial sural cutaneous nerves, branches of the common peroneal and posterior tibial nerves, respectively.[10]
The medial sural cutaneous nerve descends sub-fascially between the heads of the gastrocnemius muscle, deep to the lesser saphenous vein. At the point of myotendinous union of the gastrocnemius heads, the nerve emerges subcutaneously through the deep fascia, where it joins with the lateral sural cutaneous nerve and forms the sural nerve. The nerve confluence usually occurs at the middle or distal third of the leg.
The sural nerve courses obliquely towards the posterior aspect of the lateral malleolus, where it curves anteriorly. During its final course, the nerve gives off one collateral branch, usually 6 cm proximal to the lateral malleolus: the lateral calcaneal branch. Terminal branches of the sural nerve are located 2 cm distal to the lateral malleolus; one branch turns to the lateral dorsum of the foot and joins with the superficial peroneal nerve. The other branch reaches the lateral border of the foot.
The superficial sural artery and lesser saphenous vein accompany the nerve along its course, usually lying superficial and just posterior to the nerve.
Recent anatomical studies suggest that roughly half of sural nerves (41.4-51.5%) of sural nerves are formed by the confluence of the medial sural cutaneous and peroneal communicating nerves. Less commonly, the sural nerve arises from the union of the medial and lateral sural cutaneous nerves (8.7-31.2%), or the continuation of the medial sural cutaneous nerve in the absence of a peroneal communicating nerve (13.8-34.67%). Still less frequently, the peroneal communicating nerve (0.48-1.8%), the lateral sural cutaneous nerve (0.48-1.1%), or the sciatic nerve (0-0.7%) may become the sural nerve without any additional contributions.[11][12]
Indications
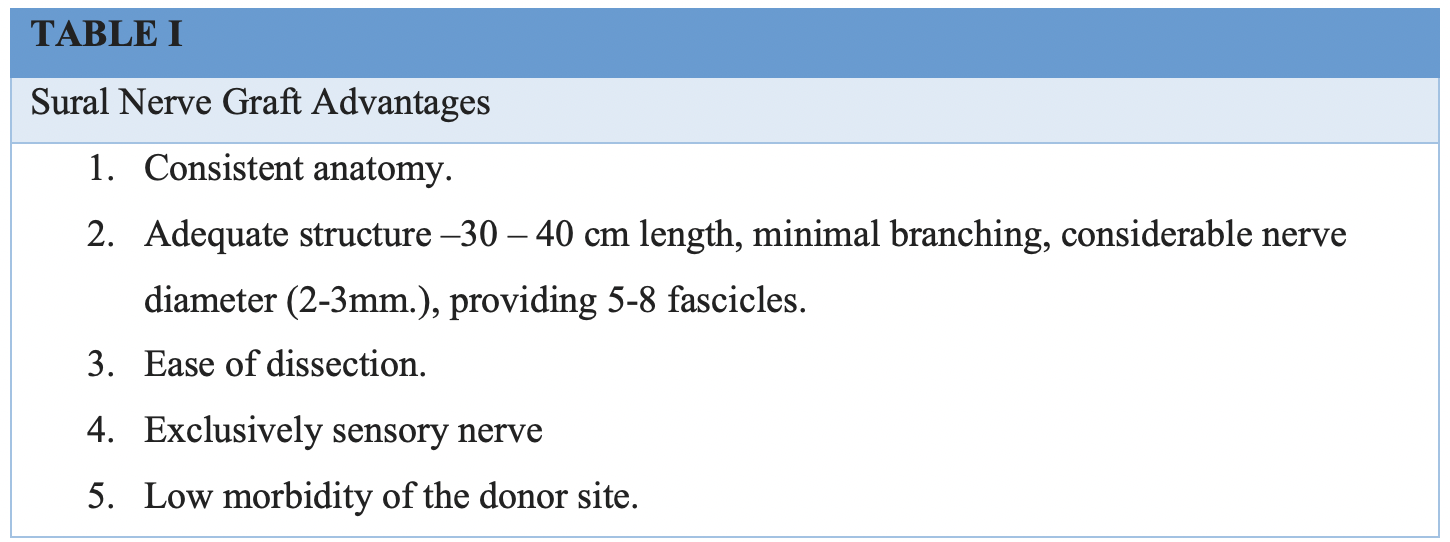
Indications for the use of sural nerve grafts are similar to indications for other nerve grafts. However, due to the advantages sural nerve grafting offers over some other autologous nerve graft options, it is frequently a reconstructive surgeon's preferred choice, particularly when repairing longer defects.[13] See Table. Advantages of Sural Nerve Graft Use for Nerve Gap Reconstruction.
Nerve grafts are commonly employed when there is a segmental loss of a motor or sensory nerve greater than 1 to 2 cm in length because judicious mobilization of the nerve stumps can frequently decrease or eliminate smaller gaps, and hollow conduits only provide reliable results for gaps <5 mm.[14] Successful use of a nerve graft, or even primary repair of a nerve injury, is predicated on the presence of viable proximal and distal nerve stumps. In cases in which no proximal nerve stump is available, for example, skull base injuries, a nerve transfer into the distal stump may provide a better reconstructive option.[15][16] In facial reinnervation, the sural nerve's prodigious length permits cross face grafting from a normal facial nerve proximally to the distal stump of the facial nerve on the paralyzed side.[17][18] The use of sural nerve grafts has also been reported for nerve elongation in the context of brachial plexus injury.[19]
In recent years, nerve grafts have been used for corneal neurotization in patients suffering from neurotrophic keratitis.[20] This condition is characterized by the presence of corneal anesthesia, which in turn produces loss of the blink reflex and tear production. As a consequence, the cornea undergoes subsequent ulceration and scarring, which may ultimately result in opacification. In this context, sural nerve and great auricular nerve grafting may be used to restore corneal sensation by extending a functional sensory nerve, usually the supratrochlear or supraorbital, and redirecting its axons towards the affected cornea.[21]
Contraindications
The primary contraindication for using nerve grafts in motor reinnervation procedures is the absence of functional motor units in the end organ. Over 12 to 18 months, the denervated muscle will atrophy and suffer fibrosis, losing the ability to contract even if the neural input is later restored.[22] For this reason, early surgical intervention is preferred, especially because the comparatively slow rate of axonal regeneration from the point of repair (1 to 1.5 mm/day) means that there will likely be a significant period of time that elapses between when the repair is performed and when the muscle actually receives neural input.[6] Another consideration is that when a nerve defect is longer than 6 cm, or there is significant surrounding soft tissue loss or planned radiation, a free vascularized nerve graft may be preferred to a traditional, non-vascularized graft.[23]
A free vascularized nerve graft may also be considered if the recipient site contains significant scarring or poor perfusion. Previous surgery or trauma involving the posterolateral aspect of the leg may prompt the surgeon to seek a different donor nerve, and nerve function should be documented before proceeding with harvest, particularly in patients with peripheral neuropathies.[24]
Equipment
Sural Nerve Graft Harvest With Tendon Stripper
- #15 blade scalpel
- #3 Bard-Parker scalpel handle
- Small Weitlaner self-retaining retractors
- Petit-point Crile forceps
- DeBakey forceps
- Bipolar electrocautery forceps
- Adson-Brown forceps
- Curved iris scissors
- Halsey needle holder
- Tendon stripper
- Vessel loops
- 4-0 poliglecaprone suture on a small, reverse cutting needle
- 3-0 polyglactin suture on controlled release needles
- Compressive wrap for dressing the leg
- Antibiotic ointment
Graft Inset
- A microvascular instrument set with jeweler forceps, non-locking needle holder, and micro scissors
- Operating microscope
- Microsurgical background
- 9-0 or 10-0 nylon suture on a spatula or cutting needle
- Fibrin glue, if desired
- Nerve conduit/wrap, if desired
Note: As an alternative, the harvest may be accomplished endoscopically through a single incision using a 5 mm 0 degree rigid endoscope, CO2 insufflation, and saphenous vein harvesting instruments.[3]
Personnel
- Surgeon
- Surgical first assist
- Anesthesia provider
- Operating room circulating nurse
- Surgical technologist
Preparation
The procedure requires a thorough explanation to the patient. An understanding of donor site morbidity consisting of anesthesia of the lateral calf and dorsum of the foot is of paramount importance. The presence of scars on the leg, mainly when performing the open harvesting technique, must be discussed prior to performing the procedure.
Technique or Treatment
Sural nerve grafting is performed under general anesthesia. The patient is placed in the supine position. A two-team approach is possible in most cases. Nerve harvesting may be performed under tourniquet control to minimize bleeding during surgery, although this is not mandatory. Optical magnification with 2.5x loupes is an option during the procedure.
The standard preparation is performed with a 10% povidone-iodine solution circumferentially from the foot to the level of the knee in the selected donor leg. Drapes are positioned so that the lateral aspect of the leg is accessible and the leg is mobile. The knee is usually flexed, and a rolled surgical towel is placed under the midfoot to maintain its position during the harvest.
A 2 cm transverse skin incision is made 1 to 2 cm posterior and 1 to 2 cm superior to the lateral malleolus. Blunt dissection then proceeds down to the subcutaneous fat. The lesser saphenous vein is usually encountered at this point, with the sural nerve lying deep and slightly anterior to it. The muscular fascia that underlies the nerve marks the floor of the dissection. It is important to identify and isolate these two structures before significant manipulation occurs, as this will collapse the vein lumen and make visually differentiating the vein and nerve challenging. After the vein is identified, it can be marked with a vessel loop and retracted anteriorly to improve the exposure of the nerve.
Once the nerve is identified, it is isolated and mobilized as far proximally as necessary to achieve the desired length. Because the sensory deficit will not likely increase in a clinically significant fashion if a greater length of the nerve is excised, the maximum length of 30-40 cm is routinely harvested by many surgeons. Blunt digital dissection may reduce trauma to the nerve and potentially improve functional outcomes; however, mobilizing the entire nerve graft this way requires exposure via either a single long incision or 2 or 3 smaller "stair-step" transverse incisions along the course of the nerve, separated by 5 to 10 cm.
At the level of the junction between the middle and upper thirds of the leg, the nerve dives through the muscular fascia, and some resistance may be encountered. Dissection may still proceed proximally past this point.
Finally, the nerve is transected proximally through the original incision and distally through a new transverse incision at the superior limit of the dissection, and then the graft is extracted. The distal end of the nerve is marked with a surgical marker, a suture, or a hemostat. This step is important as the nerve must be reversed during inset to minimize axonal loss through branches.
Once hemostasis is achieved, leg incisions are closed in two layers with deep 3-0 polyglactin and 4-0 subcuticular running poliglecaprone sutures. Antibiotic ointment and a compression wrap are applied over the incision sites.
Variations to the open technique have been described. The use of zig-zag incisions along the entire nerve course has been reported, although they worsen the aesthetic outcome without showing any real benefits in nerve harvesting or grafting results.[25]
More recently, minimally invasive techniques with endoscopic assistance have been described for sural nerve harvesting, similar to the technique used for saphenous vein harvesting for coronary artery bypass grafting. This approach decreases the number and length of incisions at the donor site, improving the cosmetic result but taking substantially more time to complete. Endoscopic visualization also offers a magnified image throughout the procedure.
Endoscopic harvest is performed similarly to the description above, with circumferential preparation and draping of the leg from the foot to the knee level. An identical incision is made posterior and superior to the lateral malleolus, and identification and marking of the lesser saphenous vein and the sural nerve are accomplished through careful dissection with blunt scissors in the subcutaneous plane and silicone loop placement.
Once isolated, the nerve is dissected proximally for a length of 1 to 2 cm, providing sufficient space for the endoscope placement. A rigid 5 mm endoscope is then introduced into the wound. Dissection proceeds proximally around the nerve for the required length and is assisted by endoscopic instrumentation. Once completely mobilized, the proximal end of the nerve is transected endoscopically; the nerve can then be extracted through the distal incision and transected proximally. Closure and dressing are performed in the same fashion as in the open approach.
If endoscopic equipment is unavailable, a nerve or tendon stripper may be used to dissect the nerve quickly and requires only two incisions: distal and proximal. Use of a stripper requires transecting the nerve proximally to thread the nerve through the stripper, and it is critical to place a clamp on the proximal end of the nerve after threading the stripper so that counter tension can be applied to prevent tangling the nerve and transecting it prematurely.
Complications
Sural nerve graft harvesting may be complicated by problems common to many surgical procedures. Poor wound healing and hypertrophic scarring may occur, as can hematoma formation. The development of a painful neuroma is rare but may cause patients activity-limiting discomfort.[26]
Postoperative anesthesia of the dorsum and lateral aspect of the foot should be considered an expected consequence of sural nerve harvesting rather than a complication.[27] This finding often improves over a period of one or two years due to collateral sprouting of adjacent sensory nerves.
Clinical Significance
Traumatic disruption of peripheral nerves is a common problem faced by plastic surgeons, orthopedic surgeons, head and neck surgeons, and oral-maxillofacial surgeons. While many of these injuries can and should be repaired primarily, longer defects will require the use of autografts, such as the sural nerve. Understanding the indications, contraindications, relevant anatomy, and operative technique will allow the surgeon to harvest the nerve safely, minimizing trauma to the graft and maximizing functional outcomes.
Enhancing Healthcare Team Outcomes
Postoperative care is an important aspect of nerve grafting. Hospital stays are typically brief, and patients are often discharged the same day as surgery or the next morning. Analgesics are prescribed to manage any post-operative discomfort. To optimize post=procedural patient outcomes requires an interprofessional team approach, including the surgeon, family clinician, nursing staff, and physical therapist, coordinating activity and sharing open communication so that all team members share a common operating picture. Each step of the patient's recovery needs to be documented, and any setbacks addressed promptly. [Level 5]
Immobilization with splints is usually necessary for a period of 3 to 4 weeks to avoid any traction on the healing nerve ends if the neurorrhaphy has been performed in an extremity. No such precautions are required in head and neck or facial surgery.
The patient must understand the goals of the surgery and the expected timeline for functional recovery. Effective communication between the surgeon and the physical therapist is critical because rehabilitation is essential to achieve optimal results from motor nerve repair. Patient compliance with postoperative care and rehabilitation regimens is also essential in order to maximize results. Due to the long and slow nature of neural function recovery, patients must be persistent and patient, which will require significant support from physicians and nursing staff during this time period.