Introduction
The submental triangle is the only unpaired triangle of the anterior triangle of the neck. It is limited by the body of the hyoid bone and the anterior bellies of the digastric muscle. The mylohyoid muscles form the floor of the submental space. However, the submental triangle can be absent or distorted because the anterior belly of the digastric muscle varies in anatomy and may be absent [1]. This area is clinically relevant as it contains essential anatomical structures, such as the submental lymph nodes that may serve as good indicators to determine metastasis [1].
Structure and Function
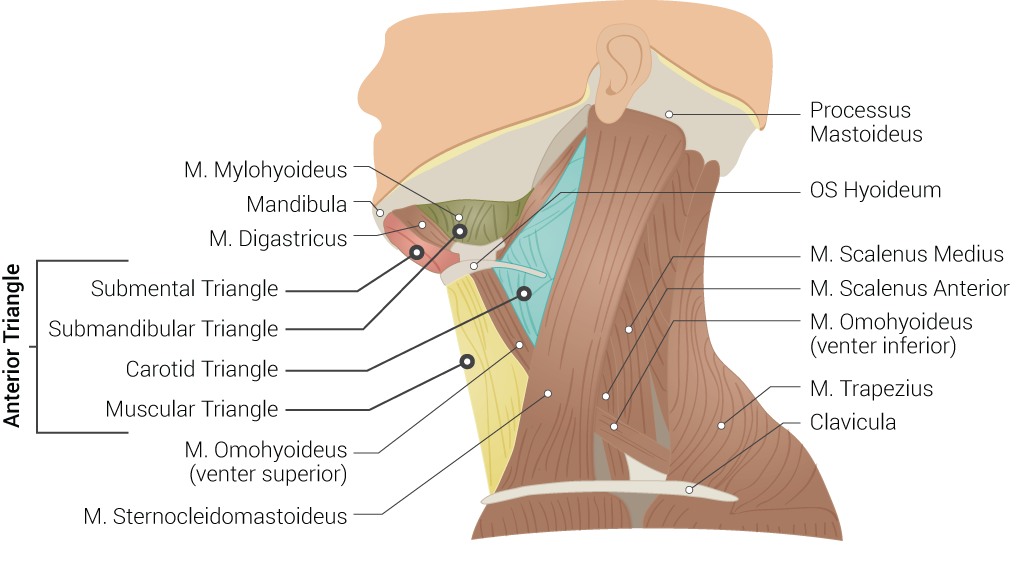
The neck is anatomically bounded by the inferior border of the mandible, the superior border of the clavicle, the midline, and the anterior border of the trapezius muscle. Two main cervical triangles are described between these limits, anterior and posterior. The posterior triangle is divided into an occipital and a supraclavicular triangle; the anterior triangle contains three paired triangles (muscular, carotid, and submandibular) and one unpaired space: the submental triangle. The neck also harbors the vertebral artery and scalene triangles in its deep layers, and Lesser's, Pirogov's, Farabeuf's, and Béclard's triangles [1].
The boundaries of the anterior cervical triangle include the anterior margin of the sternocleidomastoid muscle, the midline of the neck, and the inferior border of the mandible [1]. The submental triangle situates within this region and is differentiated from the other triangles because it is unpaired. The apex of the triangle is the chin, the base is the body of the hyoid bone, and the sides are formed by the anterior bellies of the digastric muscle. Furthermore, the left and right mylohyoid muscles constitute the floor. They insert to the mylohyoid line of the mandible and run medially and downward to attach to the body of the hyoid bone. The submental triangle harbors the submental lymph nodes that drain the mental region, the tip of the tongue, inferior lip, and incisor teeth. Also, the mylohyoid nerve and veins that drain into the anterior jugular vein traverse this region [2]. The anterior bellies of the digastric muscle, which attach to the digastric fossa, separate the submental from the submandibular triangle.
Embryology
The anterior belly of the digastric muscle starts embryonic development in the fourth week of gestation from the first pharyngeal arch [2]. Likewise, the mylohyoid muscle develops in the fourth week of gestation from the first pharyngeal arch.
Blood Supply and Lymphatics
The submental lymph nodes collect lymph from the central area of the lower lip, the skin of the mental region, the tip of the tongue, and the incisor teeth. Next, they drain into the submandibular lymph nodes and the deep cervical group, which eventually drains into the jugular lymph trunk.
The submental artery is the largest of the cervical branches of the facial artery. It emerges just after the facial artery exits from the submandibular gland. The submental artery delivers vascular supply to the skin of the submental area and the muscles that border the submental triangle, and it anastomoses with the inferior alveolar artery and the sublingual artery. It runs between the mylohyoid muscle and the mandible; it travels either deep or superficial relative to the anterior belly of the digastric muscle [3].
Nerves
The mylohyoid nerve and the lingual nerve may communicate in the submental triangle. The mylohyoid nerve penetrates the mylohyoid muscle; then, it runs parallel to the submental artery and the submental vein. The submental nerve runs beneath the submental artery and the submental vein [4].
Muscles
The mylohyoid muscle is formed by two units, left and right. It originates from the mylohyoid line located on the mandibular bone's internal surface, and both segments meet in the mylohyoid raphe in the midline. The insertion point of this muscle is located on the body of the hyoid bone. The mylohyoid muscle also separates the submandibular from the sublingual areas. Furthermore, it supports and elevates the mouth's floor and elevates the hyoid bone [5].
The digastric muscles are paired muscles formed by an anterior and a posterior belly linking the temporal bone, mandible, and hyoid bone. The anterior belly originates from the digastric fossa of the mandible and attaches to the hyoid bone, where it meets the posterior belly at the intermediate tendon. The posterior belly originates from the mastoid notch on the medial aspect of the mastoid process of the temporal bone. Then, it runs towards the hyoid bone to meet the anterior belly. The anterior bellies line the lateral sides of the submandibular triangle, open the mouth (by lowering the mandible), and elevate the hyoid bone [6].
The mylohyoid nerve, a branch of the inferior alveolar nerve, innervates the muscles that bound the submental triangle: the anterior belly of the digastric muscle and the mylohyoid muscle [2][6]. However, the anterior belly of the digastric muscle may also receive innervation from the facial nerve [7].
The submental and facial arteries are responsible for the blood supply of the anterior belly of the digastric muscle [6]. In contrast, the mylohyoid muscles are irrigated by the mylohyoid artery, a branch of the inferior alveolar artery [5].
Physiologic Variants
Researchers have found supernumerary muscle bundles in some cadavers that ran across the midline of the submental triangle. The mylohyoid nerve innervated these supernumerary muscle bundles. The researchers believed that these supernumerary muscle bundles were a combination of the anterior belly of the digastric muscle and the primordial remnants of the mylohyoid muscle [8].
Surgical Considerations
A deficiency in the differentiation of the first pharyngeal arch is responsible for some variations of the anterior belly of the digastric muscle. These variations must be taken into consideration while performing surgery in the submental triangle region [2].
When performing surgery to remove the anterior belly of the digastric muscle from the mylohyoid muscle, the lingual nerve and the hypoglossal nerve must be considered because they often present in a complicated arrangement in both the submental triangle and the submandibular triangle [4].
Clinical Significance
The submental triangle is clinically relevant because tumors and cysts develop within its limits, and abscesses from other regions extend to the area. Furthermore, swollen submental lymph nodes raise suspicion about malignant lesions in their tributary regions. However, lesions of the submental triangle usually develop from a local and benign pathology of the head and neck [9].
A study of 24 masses found in the submental triangle revealed various entities, including lipoma, sarcoidosis, non-Hodgkin lymphoma, hemangioma, abscess, dermoid cyst, and reactive lymphoid hyperplasia [9]. They also found that the submental triangle masses can be complicated by dental presentations and cheilitis [9]. Masses confined to the submental triangle are diagnosed by fine-needle aspiration, and the mainstay treatment is surgical excision except in abscesses that are treated with drainage and systemic antibiotics. Such is the case of odontogenic infections that can sometimes extend to the submental space and form an abscess. If required, the clinician will drain it via percutaneous incisions, and since the triangle lacks arteries and only contains few structures, the risk of damage during the incisions is low [1].
A congenital lymphatic malformation can manifest as a submental space mass, which is suggested by clear fluid in the fine needle aspiration and low flow lesion in ultrasonography with Doppler [10].
The submental lymph nodes are commonly involved in the metastasis of oral cavity cancer [11]. But, they are an uncommon site of tuberculous cervical lymphadenitis [12].
Submental Lymph Nodes Assessment
The cut-off value of the size of the submental lymph nodes by measuring the short axis to the long axis ratio is 0.5 [13]. There is a satisfactory level of reproducibility for the submental lymph node measurements using 3-D ultrasound [14]. Ultrasonography is sensitive and specific for assessing the submental lymph nodes. In contrast, CT scans are not particularly sensitive for determining the status of submental lymph nodes but have specificity [15].