Introduction
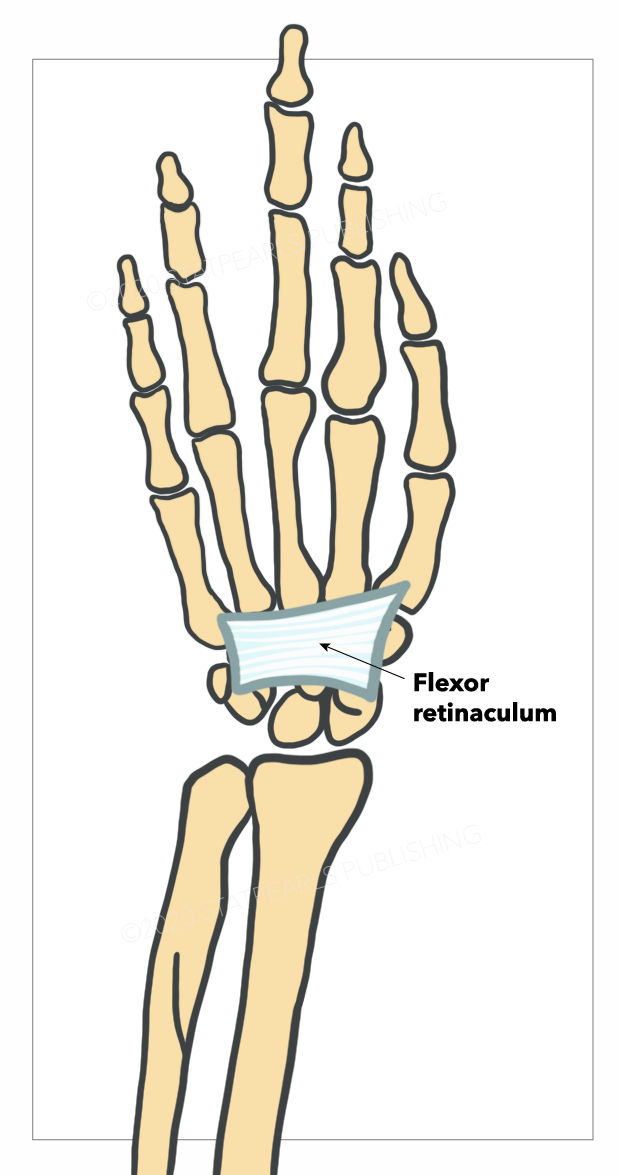
The flexor retinaculum is a fibrous connective tissue band that forms the anterior roof of the carpal tunnel (see Image. Flexor Retinaculum of the Wrist). Many experts consider the flexor retinaculum synonymous with the transverse carpal and annular ligaments. The flexor retinaculum protects 9 forearm flexor tendons and the median nerve as they pass through the carpal tunnel.[1]
Structure and Function
The flexor retinaculum begins when the longitudinally oriented antebrachial fascial fibers abruptly thicken and assume a transverse orientation. The flexor retinaculum progressively thickens from 1.5 mm to 6.0 mm distally.[1] It is about 3 cm long and 2.5 cm wide.
The flexor retinaculum attaches laterally and medially to the carpal bones, specifically:[2]
- Radial (lateral) side: scaphoid tuberosity and trapezial ridge
- Ulnar (medial) side: pisiform and hook of the hamate
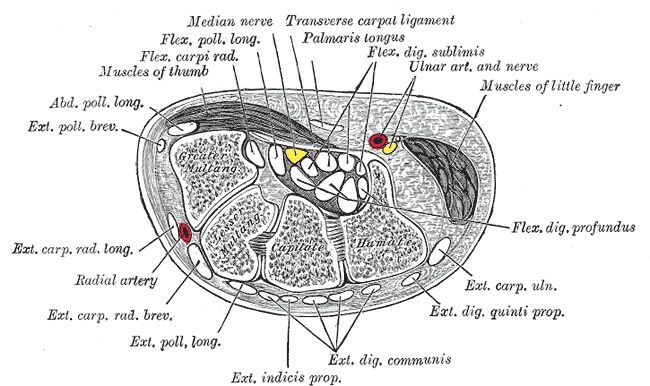
The flexor retinaculum forms the carpal tunnel's volar (anterior) boundary, while the carpal bones comprise the dorsal boundary. Posterior to the flexor retinaculum within the carpal tunnel are the 4 flexor digitorum superficialis tendons, 4 flexor digitorum profundus tendons, the lone flexor pollicis tendon, and the median nerve.[1]
The median nerve is subject to compression as it passes through the carpal tunnel. This nerve has a number of branches in the wrist and hand, the most important of which is the recurrent branch (see Image. Carpal Tunnel Cross Section).
The recurrent median nerve branch emerges inferiorly after the median nerve passes through the carpal tunnel. It then innervates the thenar muscles, which include the following:
- Abductor pollicis brevis
- Flexor pollicis brevis
- Opponens pollicis
Note that thumb motions are oriented differently from the rest of the body as this digit rotates 90° at the carpometacarpal joint. For example, arm, forearm, and finger flexion and extension occur along the sagittal plane. In contrast, thumb flexion and extension take place along the coronal plane. Thumb abduction and adduction occur along the sagittal plane.
The anterior surface of the flexor retinaculum connects with some of the tendons of the thenar and hypothenar muscles. The palmaris longus tendon adheres to the flexor retinaculum, although this muscle is absent in approximately 14% of the population.[3] The upper margin of the flexor retinaculum continues to the palmar carpal ligament, while the lower margin merges with the palmar aponeurosis. The flexor retinaculum serves as a pulley for the carpal flexor muscles and stabilizes the morphology of the carpal system.
Embryology
The flexor retinaculum is composed mainly of collagen fibers, which originate from the mesodermal leaflet (hypaxial myotome).
Blood Supply and Lymphatics
The ulnar artery is one of the branches of the brachial artery. This artery enters the hand, passing anterior to the flexor retinaculum and lateral to the flexor carpi ulnaris muscle and ulnar nerve. The ulnar artery supplies the medial aspect of the forearm and forms the superficial palmar arch in the hand.[4] In some patients, a branch of the ulnar artery passes over the flexor retinaculum.[5] The ulnar nerve passes through Guyon's canal, but the artery does not.
Nerves
The flexor retinaculum is best known for sheltering the median nerve in the carpal tunnel. The median nerve originates from the cervical spinal cord roots C5-C7 and C8-T1.[6] These cervical roots merge to form the medial and lateral cords of the brachial plexus, ultimately giving rise to the median nerve.
The median nerve then courses down the anterior arm, forearm, and into the hand. It travels down the forearm between the flexor digitorum superficialis and flexor digitorum profundus, then deep to the flexor retinaculum and through the carpal tunnel.[6]
The ulnar nerve also lies near the flexor retinaculum inside the Guyon canal, which is formed by the hook of the hamate and the pisiform bone. The pisohamate ligament serves as the anterior cover of the Guyon canal.
Hook of the hamate fractures can damage the ulnar nerve, weakening the abductor digiti minimi, flexor digiti minimi, opponens digiti minimi, and palmar and dorsal interossei. The Guyon canal is located superficial to the flexor retinaculum on its medial edge.[7]
The inability to touch the thumb with the little finger indicates paralysis of either the opponens pollicis or opponens digiti minimi. Paralysis of the little finger signifies ulnar nerve damage. Weak thumb opposition could mean injury to the median nerve or its recurrent branch. Dorsal interossei function can be tested by asking the patient to abduct the fingers against force. Loss of dorsal interossei strength is a sign of ulnar nerve damage.
Injury to the ulnar nerve is more likely to occur near the medial epicondyle or at the Guyon canal, where it is more superficial than in the forearm. Deep puncture wounds of the hand also risk ulnar nerve damage.
Muscles
The 4 tendons of the flexor digitorum superficialis and the flexor digitorum superficialis pass deep to the flexor retinaculum. The flexor digitorum superficialis originates from the medial humeral epicondyle and parts of the radius and ulna. It lies in the anterior compartment of the forearm and inserts on the base of the 2nd to 5th middle phalanges.
The median nerve innervates the flexor digitorum superficialis. It also gives rise to the anterior interosseus nerve, which innervates the lateral half of the flexor digitorum profundus (1st and 2nd digits).
The flexor digitorum superficialis muscle protects the median nerve in the forearm as it passes deep to the flexor digitorum superficialis. The primary function of this muscle is to flex the phalanges at the proximal interphalangeal joints.
Deep to the flexor digitorum superficialis is the flexor digitorum profundus, which originates from the proximal anteromedial surface of the ulna and inserts on the distal interphalangeal joints of the phalanges.[8]
The flexor digitorum profundus is innervated medially by the ulnar nerve. The distal tendons of this muscle insert on the distal phalanges of the 3rd and 4th fingers. Its main action is to flex the distal phalanges at the distal interphalangeal joints. It also flexes the proximal interphalangeal joints, metacarpal phalangeal joints, and wrist.
The flexor pollicis longus lies inferior to the flexor retinaculum and lateral to the flexor digitorum superficialis. It originates from the middle half of the volar (anterior) radius and inserts on the base of the thumb's distal phalanx.[8] The anterior interosseous nerve innervates the flexor pollicis longus.
One clinical test of the flexor pollicis longus (anterior interosseus nerve) and the adductor pollicis (ulnar nerve) is to have the patient hold a piece of paper between the thumb and index finger. If the patient cannot perform the task successfully, the problem could be with the ulnar nerve (adductor pollicis) or the anterior interosseus nerve (flexor pollicis longus). The thumb will flex at the distal phalanx if the problem is with the adductor pollicis (ulnar nerve). If distal flexion is not observed, then the problem is likely with the flexor pollicis longus (anterior interosseus nerve).
Physiologic Variants
The main anatomical variations concerning the flexor retinaculum involve the median nerve, which enters the carpal tunnel deep to the flexor retinaculum. A bifid median nerve, or when the nerve splits proximally rather than distally to the flexor retinaculum, occurs in some individuals.[2] The motor branch of the median nerve also displays a wide range of variations, which may explain why median nerve compression symptoms vary from person to person.[2][9]
Surgical Considerations
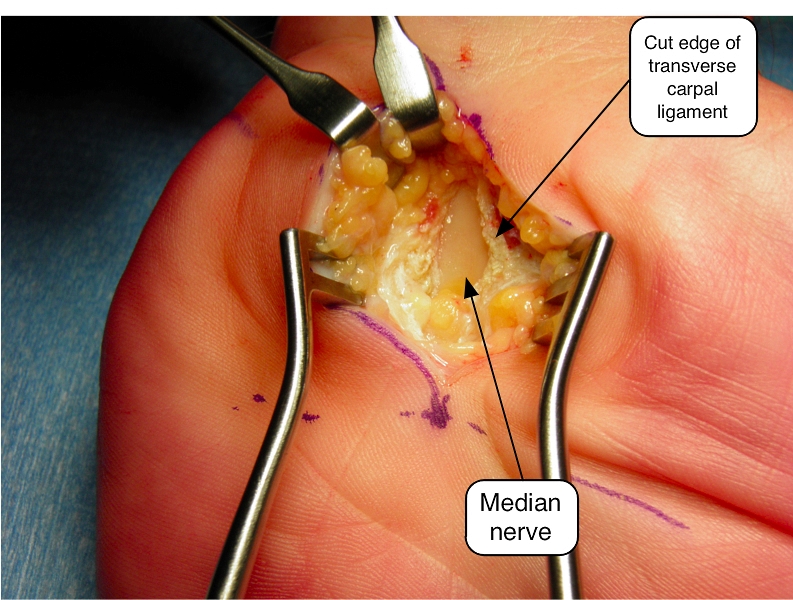
Surgical intervention is warranted if carpal tunnel syndrome symptoms do not improve with conservative management. Often, it involves cutting or releasing the flexor retinaculum to ease the pressure on the median nerve and alleviate the symptoms (see Image. Transverse Carpal Ligament Surgery). Thorough knowledge of carpal tunnel anatomy helps avoid surgical complications. Recurrence after surgery is likely if a systemic disease contributes to the development of carpal tunnel syndrome.[1][10]
Clinical Significance
The flexor retinaculum can entrap and compress the median nerve, causing carpal tunnel syndrome. This condition is the most common compression neuropathy in the upper extremity. Possible causes include occupationally related repetitive wrist motion, space-occupying lesions, and systemic conditions like diabetes mellitus and hypothyroidism.[11]
Clinically, patients may present with paresthesias in the radial 3 digits and difficulty holding objects. Patients report dropping items often. Symptoms are usually worse at night. Thenar atrophy and subsequent weakness can develop over time.[11]
The Tinel test is a classic physical exam maneuver used to diagnose carpal tunnel syndrome. This is performed by repeatedly tapping the flexor retinaculum, which elicits a pins-and-needles sensation over the median nerve's distribution area.
Carpal tunnel syndrome treatments include wrist splinting, work-related ergonomic modification, NSAIDs, steroid injections, and surgical management.
Other Issues
Myoblast proliferation may play a role early in the course of carpal tunnel syndrome, eliciting inflammatory responses and reducing tissue elasticity. Carpal tunnel syndrome is more common in women than men, owing to women's smaller carpal tunnel cross-sectional areas.