Continuing Education Activity
A conjunctival concretion is a benign entity characterized by single or multiple discrete yellowish-white deposits of varying size. They may be idiopathic and are generally noted in elderly individuals or secondary to chronic conjunctival inflammation like in trachoma. Treatment is observation or removal. This activity outlines the evaluation and treatment of conjunctival concretion and highlights the role of the healthcare team in evaluating and managing patients with this condition.
Objectives:
- Describe the pathophysiology of conjunctival concretion.
- Explain the physical exam findings associated with conjunctival concretion.
- Summarize the treatment considerations for patients with conjunctival concretion.
- Review the importance of improving care co-ordination amongst the interprofessional team to enhance the delivery of care for patients affected by conjunctival concretion.
Introduction
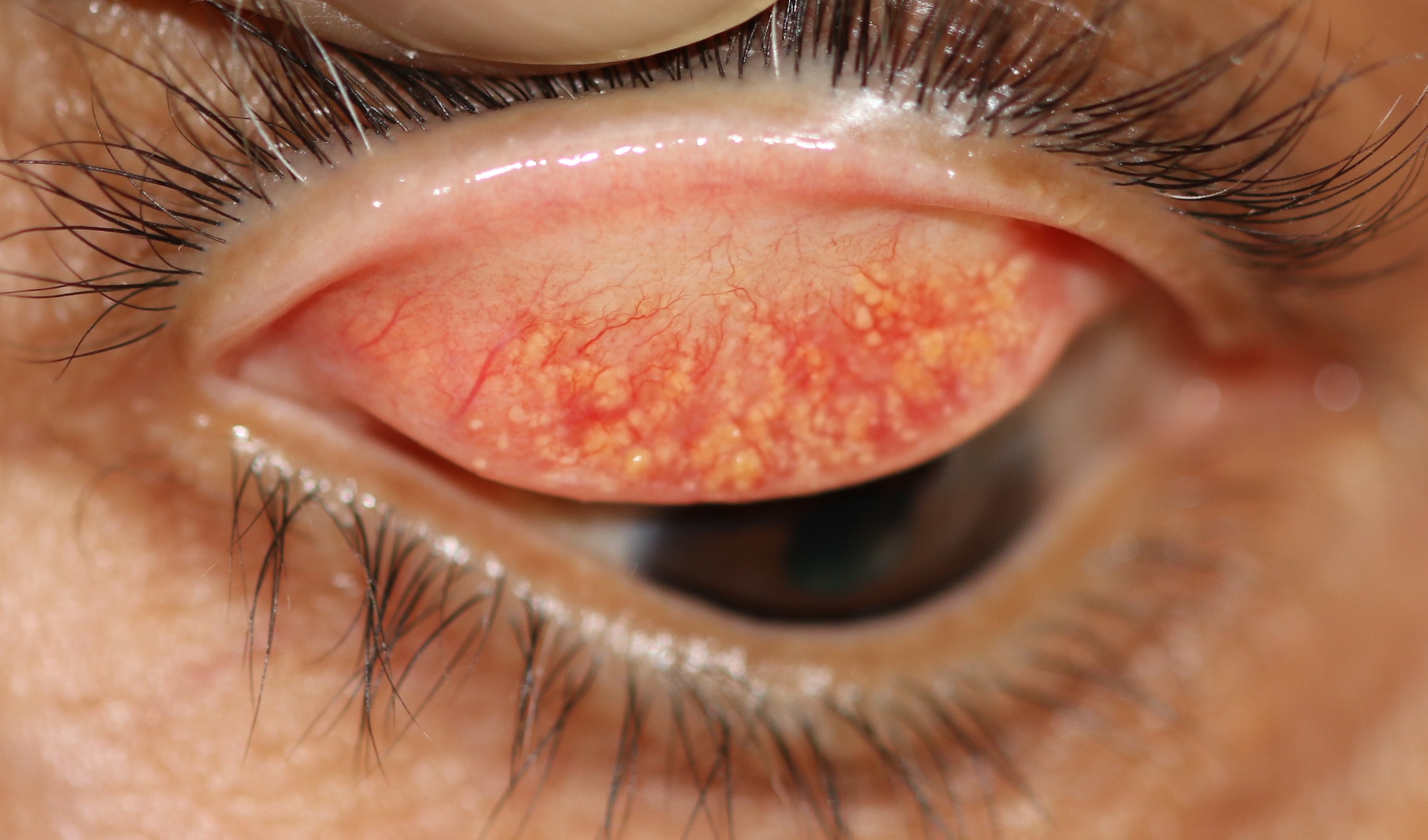
A conjunctival concretion is a benign entity characterized by single or multiple discrete yellowish-white deposits of varying size. They may be idiopathic and are generally a finding in elderly individuals or secondary to chronic conjunctival inflammation like in trachoma. They typically exist in the subepithelial space of palpebral conjunctiva or fornices. Concretions are usually asymptomatic when small but larger ones may cause symptoms.
Etiology
Concretions are mostly idiopathic and result from degenerative changes in the conjunctiva due to aging.
Secondary causes include:
- An allergic or chronic infective disorder affecting the conjunctival surface such as trachoma, allergic keratoconjunctivitis, atopic keratoconjunctivitis
- Dry eye disease associated with low-grade inflammation: chronic meibomitis or dry eye.[1]
- Recrystallization of certain drops: sulphadiazine.[2]
Epidemiology
Conjunctival concretions have no gender predilection. They are mostly a finding in elderly individuals, but it is not unusual to find them in younger people in the second or third decade of life, especially the ones that are secondary to chronic inflammation. In one study, researchers reported them in around 40 to 50% of the studied population. Research has found no predilection for the left or right eye, the upper or lower part of the palpebral conjunctiva.[3]
Pathophysiology
Subsequent to aging or inflammation, the degenerated epithelial cells with debris and inspissated proteinaceous secretions like keratin get organized and deposit in the subepithelial space or conjunctival recesses of Henle's glands. With time calcium may or may not deposit within the substance. However, there is no definitive pattern of calcium crystals on electron microscopy, and therefore the term "lithiasis" previously used is a misnomer.[4][5]
Histopathology
Microscopic examination reveals the degenerated epithelial cells along with mucinous secretions. Sometimes there can be an epithelial lined cyst on the top surface of the concretion. The concretions strongly stain for dyes to stain phospholipid and elastin, weakly for polysaccharides and lipids. They do not stain for amyloid, collagen, DNA, RNA, calcium, iron, and mucopolysaccharides.[6]
History and Physical
Usually, the patient is asymptomatic. Concretions are usually detected incidentally when the eye is examined for some other purpose.
When large, they may become symptomatic. The patient may present with complaints of:
- Irritation
- A foreign body sensation that can usually localize to a specific point
- Tearing
- Redness
- Photophobia (usually with large concretions on the upper tarsal conjunctiva that rub against the cornea
- Photophobia
- Blurry vision
Evaluation
A diagnosis is made upon clinical examination with eversion of the eyelids and examination under the biomicroscope. Concretions may be single or multiple. They present as yellowish-white structures located in the palpebral conjunctiva or fornices. They may become confluent, and these, as well as the larger ones, may erode through the conjunctiva and protrude to become symptomatic. The surrounding conjunctiva may show signs of allergy-like follicles and redness.
Treatment / Management
If the patient is asymptomatic and the finding of concretions is incidental, it is best not to perform any procedures. Most concretions remain asymptomatic and do not need a specific treatment.
If the patient is symptomatic, the specific concretions may be removed.
Method of removal: Proparacaine hydrochloride 0.5% drops are instilled, and the lid is everted to expose the palpebral conjunctival surface. Applying the anesthetic via a Q-tip soaked with the anesthetic on the concretion is useful in achieving better local anesthesia. The concretions may either be removed using a 26G or 30G needle with bevel away from tarsus and just nudging the concretion at one end and lifting it from the conjunctiva. Fine-tipped forceps may also be used. Mild oozing is common and is easily controllable with simple local pressure. A topical antibiotic drop or ointment is administered. If there has been a breakdown of the corneal surface, a few days of antibiotic drops or ointment are prescribed.
Differential Diagnosis
Three entities require differentiation from the conjunctival concretion:
- Conjunctival foreign body: if small and buried in the conjunctiva with a part protruding from the conjunctiva the foreign body may mimic a concretion
- Epidermal inclusion cyst: can be congenital or acquired. These are cystic lesions in the subepithelium space but have clear fluid, unlike concretions that are solid and filled with keratin.[7]
- Lymphoid follicle: these are also found in the subepithelial space but are usually diffuse and multiple. Histologically they have central immature lymphocytes and surrounding mature cells.[8]
- Rarely with ophthalmia nodosa: ophthalmia nodosa is a conjunctival or corneal inflammatory response to hair, caterpillar spines, and other foreign bodies. They may also cause multiple linear abrasions on the cornea. However, unlike with concretions, these eyes show more inflammation and a granulomatous reaction around the foreign body. [9] Pagenstecher, in 1883, described the first case of ophthalmia nodosa and termed the disease "caterpillar hair ophthalmia." Wagenmann reported a case in 1890, and mistakenly called it pseudotuberculosis. Saemisch, in 1904, gave the condition the correct name. In the early 20th Century, the condition was termed "nursemaid's disease" because of the frequency with which nursemaids who sat under the trees in Hyde Park as they watched children became afflicted by urticaria and conjunctivitis caused by hairs from the vapourer moth (Orgyn antiqua).
Prognosis
Conjunctival concretions are a benign condition. Treatment of symptomatic lesions offers a cure. If the concretions are associated with inflammation or allergy, appropriate treatment for these conditions is necessary to prevent a recurrence. It is wise not to remove asymptomatic concretions.
Complications
Conjunctival concretions are rarely associated with complications. Corneal abrasion caused by prominent concretions can cause irritation, pain, photophobia, redness, blurring of vision or corneal ulceration, and dry eye.[10]
Deterrence and Patient Education
A diagnosis of concretions is usually made incidentally during a routine eye examination under the biomicroscope. Once diagnosed, the clinician should reassure the patient that the condition is entirely benign. Asymptomatic patients can undergo observation. In the presence of a foreign body sensation, irritation, redness, or watering, these concretions can be necessary. Removal of concretions is performed with a topical anesthetic in an outpatient setting, usually in the clinic. Recovery is generally rapid, with little discomfort. Recurrence of concretions may occur, especially if there is associated inflammation.
Enhancing Healthcare Team Outcomes
Ophthalmologists or optometrists are the first to diagnose conjunctival concretions. The diagnosis requires confirmation with slit-lamp biomicroscopy. The benign nature of the condition should be stressed. The healthcare team consisting of ophthalmologists, optometrist, nurse, and pharmacist should all be aware of the condition, how to diagnose, and the treatment options available for the condition. However, treatment should only be by a trained ophthalmologist. Not all cases require treatment, just symptomatic cases. Histopathology is usually not necessary. The excellent prognosis should be discussed with the patient.