Continuing Education Activity
Dental caries is a common chronic infectious resulting from tooth-adherent cariogenic bacteria, primarily Streptococcus mutans, which metabolize sugars to produce acid, demineralizing the tooth structure over time. This activity describes the evaluation and management of dental caries and highlights the role of the interprofessional team in evaluating and treating patients with dental caries.
Objectives:
Describe the etiology of dental caries.
Summarize the pathophysiology of dental caries, highlighting the currently accepted theory.
Describe dental caries' clinical findings.
Explain the treatment considerations for patients with dental caries.
Introduction
Dentistry dates back to 5000 B.C. when the thinking was that the cause of dental caries was a “tooth worm.” The term “dental caries” was first reported in the literature around 1634, and it originates from the Latin word “caries,” which stands for decay. The term was initially used to describe holes in the teeth. Dental caries is reported to be one of the oldest and most common diseases found in humans. Dental caries is a prevalent chronic infectious disease resulting from tooth-adherent cariogenic bacteria that metabolize sugars to produce acid, which, over time, demineralizes tooth structure.
Etiology
Dental caries is a term that refers to both the disease and the resulting lesion. The caries process occurs in the biofilm, which is permanently active with every pH fluctuation [1], and the lesion manifests in the dental hard tissues.
Dental caries occurs when the biofilm microbiota that normally resides in the oral cavity in homeostasis change to an acidogenic, aciduric, and cariogenic population due to the frequent consumption of sugars.[2] The result of this shift can be clinically invisible or lead to a net mineral loss within the tooth's hard structures, resulting in a visible carious lesion.[1] - caries, the process, can exist without caries, the visible lesion.
Therefore, dental caries is considered a dietary-microbial disease [3] that requires a cariogenic biofilm and regular exposure to fermentable carbohydrates (glucose, fructose, maltose, and sucrose) from the diet.
Behavioral, psychological, and social factors also play a significant role in the disease process.[4] Fluoride's capacity to prevent caries is a well-known fact, and insufficient fluoride exposure should also be considered a contributing factor in the disease process.[5]
Epidemiology
Dental caries is a major healthcare problem as it is the most prevalent disease worldwide.[6] Almost 100% of adults are affected by dental caries.[7] The disease concentrates in groups with low socioeconomic status,[6] and despite being easily preventable, its prevalence did not significantly decrease over the last thirty years.[8]
Pathophysiology
Microbial Role
Carious lesions have a higher percentage and incidence of certain bacterial species: Streptococcus mutans, Streptococcus sobrinus, and Lactobacilli, isolated from advanced caries.[9] The specific plaque hypothesis was based on this finding, believing only specific bacteria caused the disease.[10] Indeed, Streptococcus mutans, in particular, are strongly linked to caries, but caries can develop in sites where Streptococcus mutans are absent.[3] This observation gave rise to the nonspecific plaque hypothesis, where caries is believed to result from the net metabolic activity of the microbiota of the biofilm. Although the etiology of dental caries is not completely specific, we cannot ignore that a limited type of bacteria is consistently found in higher numbers from the affected areas.[11] The currently accepted concept is the ecological plaque hypothesis.
The ecological plaque hypothesis believes that dental caries is not caused by a specific type of microorganism acting alone but is the result of a shift in the microbiota of the dental biofilm towards more cariogenic species.[3] Oral acidic conditions from regular sugar consumption select the bacteria that empathize more with this environment and eliminate the benign species that do not tolerate such conditions.[3]
Demineralization and remineralization
Fermentable carbohydrates are metabolized by the biofilm bacteria that produce organic acids, primarily lactic acid. These end products of bacterial metabolism accumulate in the fluid phase of the biofilm, causing a pH drop and demineralization of the surface layer of the tooth.[12]
The enamel porosity increases, the spaces between the crystals widen, and the surface softens, which provides an opportunity for the acids to get deeper into the tooth structure and demineralize the subsurface.[3]
At this point, the reaction products of the demineralization - calcium and phosphate - accumulate in the enamel surface and can protect it from further mineral loss.[3] Also, available fluoride can help to protect from surface demineralization.[13]
Sugars are swallowed and cleared by saliva that can return the biofilm pH to neutrality thanks to its buffer capacity; calcium, phosphate, and fluoride now remineralize the tooth's surface.[3]
If the acidic conditions perpetuate, the pH drops will continue, reaching a point when the rate of mineral loss in the subsurface is higher than the surface, resulting in a subsurface lesion. When there is sufficient mineral loss, a white spot becomes clinically visible.
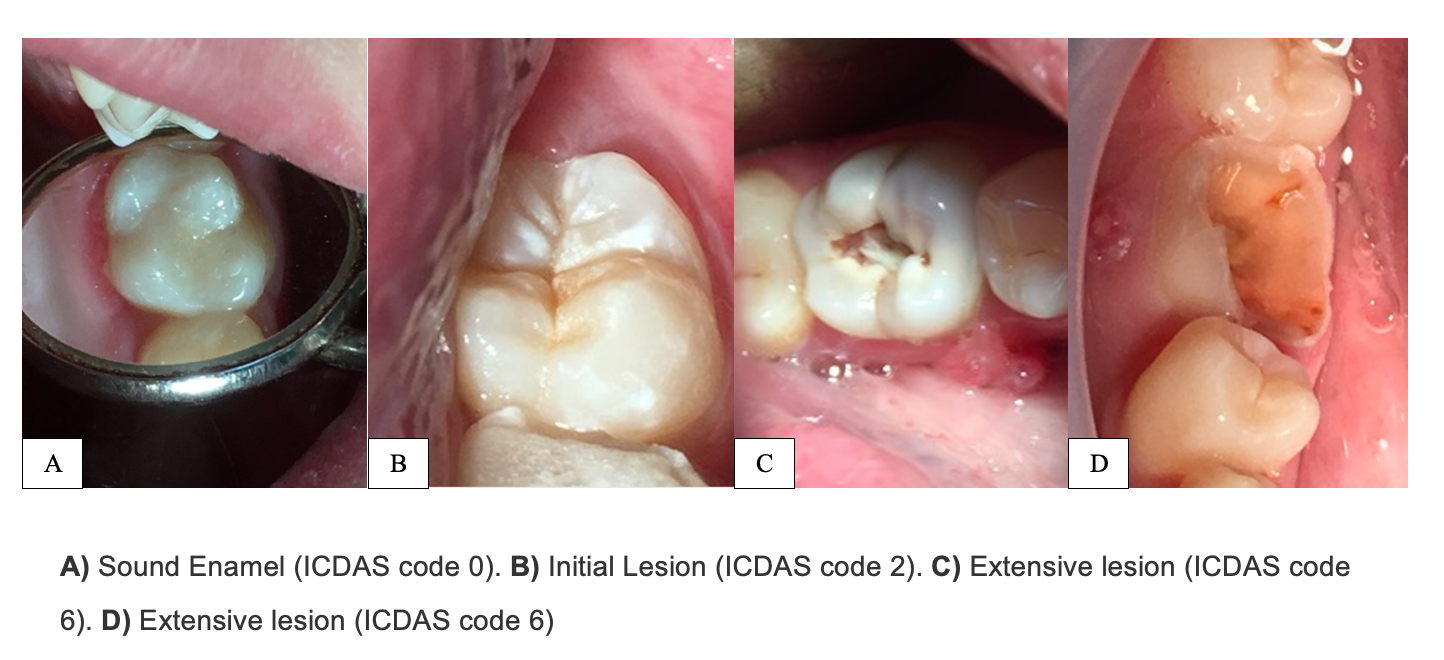
A white spot can be arrested or reversed if behavioral changes and preventive measures are implemented (ICDAS 1 and 2).[3] If caries progresses further, microcavities are formed in the enamel due to the increased surface porosity, clinically corresponding to an ICDAS code 3.[3] The surface lesion will collapse with time, leaving a macroscopic hole (ICDAS 5 or 6).[3] Despite the severity of the lesion at this point, it can still be arrested, but the cavity will remain.[3]
Histopathology
A carious tissue consists of four different zones histologically, among which three zones are visible clinically. The outer layer consists of the necrotic zone and contaminated zone containing microbial biofilm, which can be appreciated clinically as soft mineralized tissue of the tooth. This necrotic zone has a very high microbial load. The next zone is the zone of demineralization, characterized by very few microorganisms, minimal nutrients, and an anaerobic atmosphere. This zone can be correlated clinically as leathery dentine. Finally, the innermost zone near the pulp is the translucent zone of a firm, softer dentine. Demineralization and the absence of microorganisms characterize this zone because microbial flora cannot penetrate to this depth.
History and Physical
The first clinical sign of the disease is a white spot, which is the expression of the enamel subsurface demineralization - the surface enamel is more mineralized. If the acid challenge continues, the previously smooth enamel surface becomes rough. Eventually, enamel microcavitations and cavitations may occur - the average time that the carious lesions remain radiographically in the enamel was suggested to be three to four years [14], but lesions are highly variable, and they have the potential to regress.
As the caries process progresses, the dentin also experiences mineral loss and bacterial invasion, producing tertiary dentin to protect the pulp.
Active or Inactive?
We can determine if a carious lesion is active or inactive according to several factors:[3]
- Location: is the lesion in a plaque stagnation area? Is it located along the gingival margin?
- Aspect: is it white or brown? Is it matte or shiny?
- Texture: is it rough or smooth?
- Integrity: is it cavitated or non-cavitated?
- Gingival bleeding on probing: is the gingiva bleeding on probing?
A carious lesion is considered active when it shows more of these characteristics: it is whitish, matte, has a rough texture (when carefully touched with the tip of a blunt probe), has plaque stagnation, is cavitated, and if there is gingival bleeding.[15]
By contrast, a carious lesion is presumed inactive if it has the opposite characteristics: brownish, shiny, smooth, non-cavitated, it is not associated with plaque and away from the gingival margin, and there is no gingival bleeding on probing.
Root Caries
Root caries also start as subsurface demineralization, like enamel caries; however, root caries become softer at an earlier stage.[16] These lesions tend to look extensive, but they rarely exceed 0.5 to 1 mm deep. Root caries provide time to implement plaque control measurements to arrest them, thanks to the slow rate of microbial penetration and tissue degradation they experience.[16]
Recurrent Caries
A recurrent or secondary caries is a new caries that form at the restoration’s margin.[17] A microleakage of the restoration causes it; however, this leakage does not result in an active demineralization under the filling.[16]
Evaluation
Evaluation of dental caries involves using various techniques, such as the visual-tactile method, radiographs, fiberoptic illumination (FOTI), and digital fiberoptic illumination (DIFOTI). The most common and easiest method is the conventional visual-tactile method. Several radiographic techniques are effective for detecting caries radiographically, such as intraoral periapical radiographs and bitewing radiographs for occlusion-proximal caries.
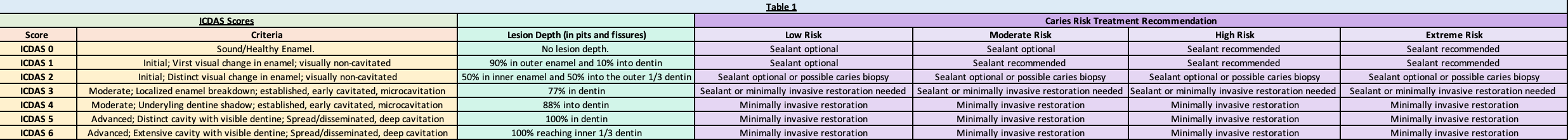
The International Caries Detection and Assessment System (ICDAS) is a useful tool for detecting and recording caries. This system classifies carious lesions into six categories, where a higher score correlates with a more advanced lesion. The ICDAS tracks the progression of carious lesions and is an accurate and reproducible caries classification system.[18] (Table 1).
Newer diagnostic devices, including laser fluorescence detection and light-induced fluorescence, provide extra information on the carious lesion. Light-induced fluorescence can show the lesion’s extension, specific location, and bacterial activity [18]; laser fluorescence detection devices detect demineralization and remineralization cycles.
Treatment / Management
The management of dental caries should be aimed at 1) detecting initial lesions, 2) determining caries activity, 3) performing a caries risk assessment, 4) preventing new carious lesions, 5) preserving dental tissue, and 6) maintaining teeth for as long as possible.
Existing caries should be initially managed by non-invasive procedures (e.g., remineralization, biofilm removal, sealing) instead of removing dental tissue. Cavitated lesions should be arrested or controlled following a minimally invasive approach, e.g., repairing a defective restoration instead of replacing it.[2]
Non-invasive Procedures
We do not need to place a filling in a lesion that can be accessed by easy cleaning measures that will disturb the biofilm, such as fluoride-containing toothpaste.[1]
The following lesions can be managed conservatively without the need for a filling:
- White spot lesions, including initial occlusal lesions.[1][19]
- When on a bitewing x-ray, approximal lesions are limited to the enamel or are just into dentin. (It is improbable that these lesions are cavitated in modern populations).[1]
- Cavitated and non-cavitated root surface lesions can be reached by cleaning implements.[20][1]
- If a recurrent lesion adjacent to a restoration is cleansable, it does not require restoration.[1]
When do we restore?
In 2016, The International Caries Consensus Collaboration [2] presented recommendations for carious tissue removal and cavitated lesions management. They based the decision-making process on whether the lesion can be reached by cleaning implements - cleansable lesion - or not - non-cleansable lesion; if surface cavitation is present, the lesion should be considered non-cleansable and active.[2]
The resulting consensus was as follows:
- “Noncleansable cavitated dentine caries cannot be managed by biofilm removal, remineralization, or sealing alone. However, in the primary dentition, these lesions might be transformable into cleansable lesions and managed via nonrestorative cavity control.”[2]
- “Certain occlusal lesions might appear clinically non-cavitated but radiographically extend significantly into dentine. If such lesions cannot be arrested through biofilm control alone, fissure sealing can be carried out; however, the integrity of the sealant needs to be monitored, and there is a possibility, until more evidence has emerged, that a “trampoline” effect may lead to failure of the sealant and restoration will be required.”[2]
Furthermore, Kidd et al.[1] recommend performing invasive treatments in cavitated occlusal lesions (ICDAS codes 3 or higher) visible in dentin on a bitewing x-ray and cavitated approximal lesions that are clearly in dentin on a bitewing x-ray.
Differential Diagnosis
Dental caries should be differentiated from developmental lesions (hypoplasia, hypomineralization, dental fluorosis, amelogenesis, and dentinogenesis imperfecta) and mechanical and chemical trauma (tooth wear).
Prognosis
Dental caries prognosis depends on the patient's health, maintenance of oral hygiene, and the extent and severity of dental caries. If the individual reports early signs of dental caries, a lesion may be reversed with a preventive method and minor dental intervention like remineralization of the initial lesion. If dental caries progresses to the moderate stage with loss of specific tooth structure, the tooth must be filled and rebuilt.
Complications
- Apical periodontitis
- Periapical abscess
- Periapical granuloma
- Periapical cyst
- Cellulitis
- Abscess
- Periostitis
- Osteomyelitis
Dental caries are not life-threatening, but if the infection spreads through facial planes, patients are at increased risk of sepsis, airway compromise (Ludwig angina), and odontogenic infections, which accounted for 49.1% of cases in a study of deep neck abscesses.[21]
Deterrence and Patient Education
Prevention Strategies
Meticulous Maintenance of Oral Hygiene:
As dental caries cannot progress without the presence of microorganisms present in dental plaque, daily removal of dental plaque with tooth brushing and flossing is considered to be the best preventive method.
Topical Fluoride Application
Fluoride inhibits dental caries by inhibiting demineralization and enhancing remineralization of tooth structure by the formation of acid-resistant fluorapatite crystals. Various methods that incorporate fluoride in daily life include fluoridated water supply, use of fluoridated toothpaste, use of fluoridated mouth rinse, and application of different professional fluoride gels and varnishes.
Application of Pit and Fissure Sealants: Pits and fissures pose a non-cleansable morphology and are, hence, the most susceptible site for the initial development of caries. Pit and fissure sealants provide a mechanical barrier that deprives the microbes of sugars and hence halts the progression of dental caries.
Xylitol: The main dietary culprit in the formation of dental caries is sucrose. Nowadays, sucrose is being replaced by xylitol, an artificial sweetener that is not only non-cariogenic but also anti-cariogenic.
Enhancing Healthcare Team Outcomes
The early stages of dental caries and their management frequently pose a dilemma. Dental caries occurs when the biofilm microbiota that normally resides in the oral cavity in homeostasis changes to an acidogenic, aciduric, and cariogenic population due to the frequent consumption of sugars.[2] The result of this shift can be clinically invisible or lead to a net mineral loss within the tooth's hard structures, resulting in a visible carious lesion - a white spot.[1] If plaque control measures are performed, the lesion can regress without the need for invasive intervention. Existing caries should be initially managed by non-invasive procedures (eg, remineralization, biofilm removal, sealing) instead of removing dental tissue. Cavitated lesions should be arrested or controlled following a minimally invasive approach, e.g., repairing a defective restoration instead of replacing it.[2] Dentists should undertake a conservative approach when treating dental caries, and professionals from other dental specialties should detect early carious lesions and make appropriate referrals promptly to improve patients' outcomes.