[1]
Lehmann P, Schwarz T. Photodermatoses: diagnosis and treatment. Deutsches Arzteblatt international. 2011 Mar:108(9):135-41. doi: 10.3238/arztebl.2011.0135. Epub 2011 Mar 4
[PubMed PMID: 21442060]
[2]
Lembo S, Raimondo A. Polymorphic Light Eruption: What's New in Pathogenesis and Management. Frontiers in medicine. 2018:5():252. doi: 10.3389/fmed.2018.00252. Epub 2018 Sep 10
[PubMed PMID: 30250845]
[4]
Photiou L,Foley P,Ross G, Solar urticaria - An Australian case series of 83 patients. The Australasian journal of dermatology. 2018 Dec 25;
[PubMed PMID: 30585308]
Level 2 (mid-level) evidence
[5]
Paek SY, Lim HW. Chronic actinic dermatitis. Dermatologic clinics. 2014 Jul:32(3):355-61, viii-ix. doi: 10.1016/j.det.2014.03.007. Epub
[PubMed PMID: 24891057]
[6]
Ahad T, Rhodes LE. Images in paediatrics: Haemorrhagic vesicles and varioliform scarring: consider photosensitivity. Archives of disease in childhood. 2020 Mar:105(3):302-303. doi: 10.1136/archdischild-2018-316272. Epub 2018 Nov 13
[PubMed PMID: 30425076]
[7]
Blakely KM, Drucker AM, Rosen CF. Drug-Induced Photosensitivity-An Update: Culprit Drugs, Prevention and Management. Drug safety. 2019 Jul:42(7):827-847. doi: 10.1007/s40264-019-00806-5. Epub
[PubMed PMID: 30888626]
[8]
Ibbotson S . Drug and chemical induced photosensitivity from a clinical perspective. Photochemical & photobiological sciences : Official journal of the European Photochemistry Association and the European Society for Photobiology. 2018 Dec 5:17(12):1885-1903. doi: 10.1039/c8pp00011e. Epub
[PubMed PMID: 30283959]
Level 3 (low-level) evidence
[9]
Snyder M, Turrentine JE, Cruz PD Jr. Photocontact Dermatitis and Its Clinical Mimics: an Overview for the Allergist. Clinical reviews in allergy & immunology. 2019 Feb:56(1):32-40. doi: 10.1007/s12016-018-8696-x. Epub
[PubMed PMID: 29951786]
Level 3 (low-level) evidence
[10]
Velander MJ, Þorsteinsdóttir S, Bygum A. [Clinical review of pseudoporphyria]. Ugeskrift for laeger. 2015 Feb 2:177(6):. pii: V11140599. Epub
[PubMed PMID: 25650579]
[11]
Foering K, Chang AY, Piette EW, Cucchiara A, Okawa J, Werth VP. Characterization of clinical photosensitivity in cutaneous lupus erythematosus. Journal of the American Academy of Dermatology. 2013 Aug:69(2):205-13. doi: 10.1016/j.jaad.2013.03.015. Epub 2013 May 3
[PubMed PMID: 23648190]
[12]
Auriemma M, Capo A, Meogrossi G, Amerio P. Cutaneous signs of classical dermatomyositis. Giornale italiano di dermatologia e venereologia : organo ufficiale, Societa italiana di dermatologia e sifilografia. 2014 Oct:149(5):505-17
[PubMed PMID: 25014587]
[13]
Baba T, Yaoita H. UV radiation and keratosis follicularis. Archives of dermatology. 1984 Nov:120(11):1484-7
[PubMed PMID: 6497416]
[15]
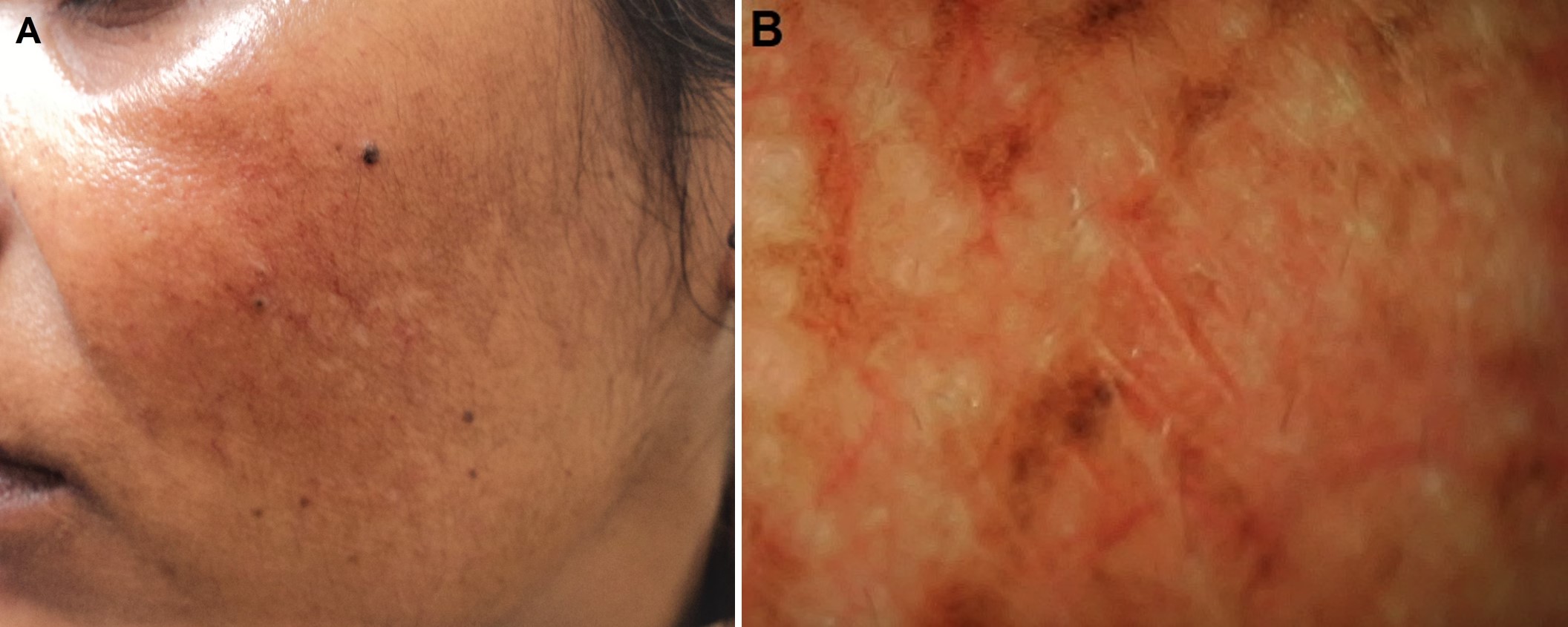
Suggs AK,Hamill SS,Friedman PM, Melasma: update on management. Seminars in cutaneous medicine and surgery. 2018 Dec;
[PubMed PMID: 30475935]
[16]
Igawa K, Matsunaga T, Nishioka K. Involvement of UV-irradiation in pemphigus foliaceus. Journal of the European Academy of Dermatology and Venereology : JEADV. 2004 Mar:18(2):216-7
[PubMed PMID: 15009310]
[17]
Ellenbogen E, Wesselmann U, Hofmann SC, Lehmann P. Photosensitive atopic dermatitis--a neglected subset: Clinical, laboratory, histological and photobiological workup. Journal of the European Academy of Dermatology and Venereology : JEADV. 2016 Feb:30(2):270-5. doi: 10.1111/jdv.13451. Epub 2015 Nov 2
[PubMed PMID: 26523351]
[18]
Palmer RA, Hawk JL. Light-induced seborrhoeic eczema: severe photoprovocation from subclinical disease. Photodermatology, photoimmunology & photomedicine. 2004 Feb:20(1):62-3
[PubMed PMID: 14738536]
[19]
Wolf P,Weger W,Patra V,Gruber-Wackernagel A,Byrne SN, Desired response to phototherapy vs photoaggravation in psoriasis: what makes the difference? Experimental dermatology. 2016 Dec;
[PubMed PMID: 27376966]
[21]
Rodríguez-Pazos L, Gómez-Bernal S, Rodríguez-Granados MT, Toribio J. Photodistributed erythema multiforme. Actas dermo-sifiliograficas. 2013 Oct:104(8):645-53. doi: 10.1016/j.adengl.2012.01.024. Epub 2013 Aug 17
[PubMed PMID: 23962583]
[22]
Haber R, Ram-Wolff C, Laly P, Bouaziz JD, Jachiet M, Rivet J, Bagot M. Photo-sensitive mycosis fungoides: a new variant? European journal of dermatology : EJD. 2017 Apr 1:27(2):181-182. doi: 10.1684/ejd.2016.2924. Epub
[PubMed PMID: 27869099]
[24]
Wang B, Rudnick S, Cengia B, Bonkovsky HL. Acute Hepatic Porphyrias: Review and Recent Progress. Hepatology communications. 2019 Feb:3(2):193-206. doi: 10.1002/hep4.1297. Epub 2018 Dec 20
[PubMed PMID: 30766957]
[25]
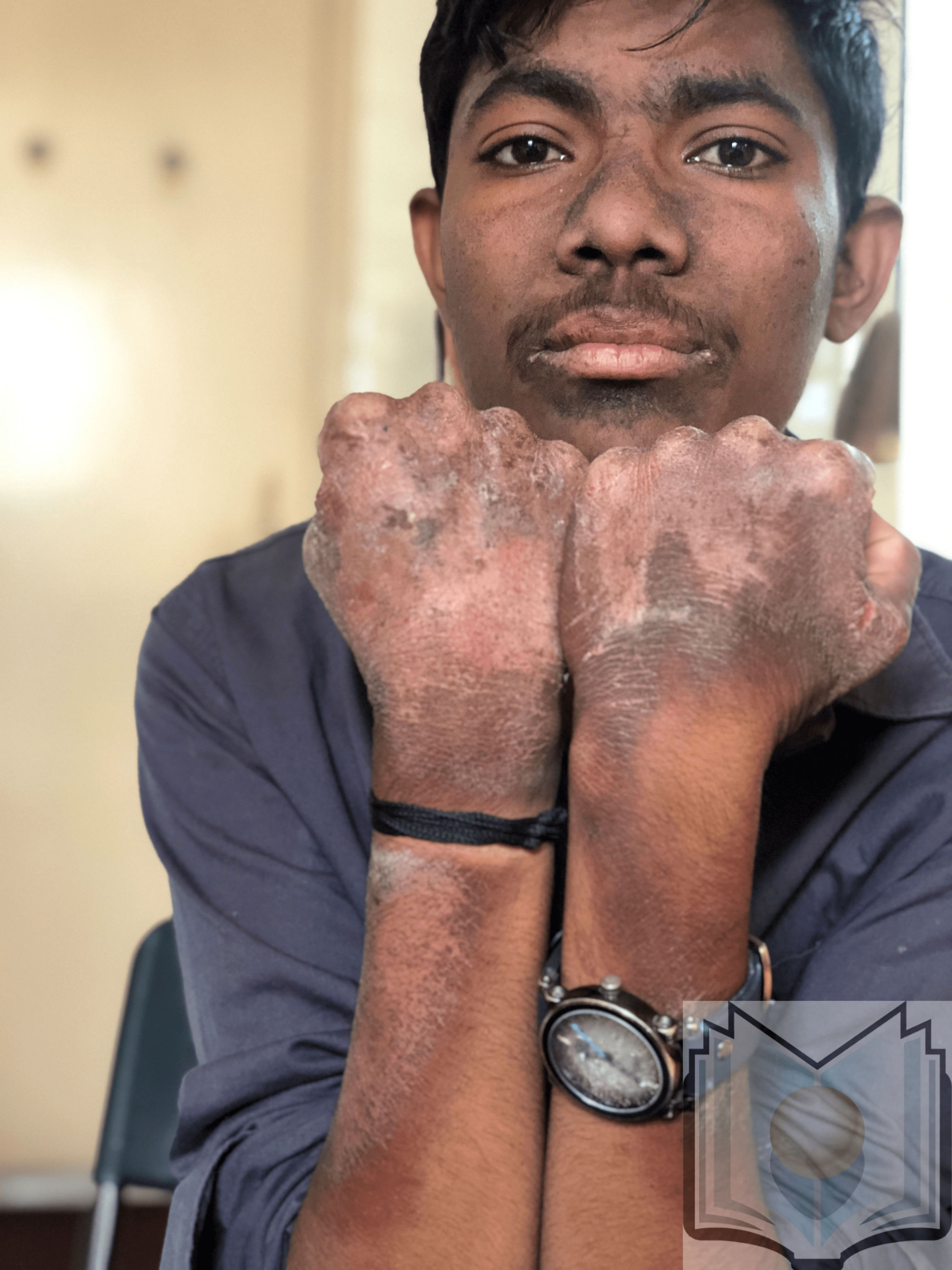
Erwin AL, Desnick RJ. Congenital erythropoietic porphyria: Recent advances. Molecular genetics and metabolism. 2019 Nov:128(3):288-297. doi: 10.1016/j.ymgme.2018.12.008. Epub 2018 Dec 27
[PubMed PMID: 30685241]
Level 3 (low-level) evidence
[26]
Lehmann J, Seebode C, Martens MC, Emmert S. Xeroderma Pigmentosum - Facts and Perspectives. Anticancer research. 2018 Feb:38(2):1159-1164
[PubMed PMID: 29374753]
Level 3 (low-level) evidence
[28]
Yew YW, Giordano CN, Spivak G, Lim HW. Understanding photodermatoses associated with defective DNA repair: Photosensitive syndromes without associated cancer predisposition. Journal of the American Academy of Dermatology. 2016 Nov:75(5):873-882. doi: 10.1016/j.jaad.2016.03.044. Epub
[PubMed PMID: 27745642]
Level 3 (low-level) evidence
[30]
Giordano CN,Yew YW,Spivak G,Lim HW, Understanding photodermatoses associated with defective DNA repair: Syndromes with cancer predisposition. Journal of the American Academy of Dermatology. 2016 Nov
[PubMed PMID: 27745641]
Level 3 (low-level) evidence
[31]
Gozali MV, Zhou BR, Luo D. Update on treatment of photodermatosis. Dermatology online journal. 2016 Feb 17:22(2):. pii: 13030/qt1rx7d228. Epub 2016 Feb 17
[PubMed PMID: 27267185]
[32]
Guarrera M. Polymorphous Light Eruption. Advances in experimental medicine and biology. 2017:996():61-70. doi: 10.1007/978-3-319-56017-5_6. Epub
[PubMed PMID: 29124691]
Level 3 (low-level) evidence