Continuing Education Activity
Erythema annulare centrifugum is an annular, erythematous lesion that appears as urticaria-like papules, enlarges centrifugally, and clears centrally. A fine scale, called a trailing scale, is sometimes inside the advancing edge. The lesion is classified as a reactive erythema and has been associated with many different conditions. The cause of erythema annulare centrifugum is frequently unknown. Often, the eruption of erythema annulare centrifugum diminishes with therapy for the underlying disease. When the condition occurs as part of a paraneoplastic phenomenon, this is called paraneoplastic erythema annulare centrifugum eruption.
This activity describes the pathophysiology, evaluation, and management of erythema annulare centrifugum and highlights the role of the interprofessional team in diagnosing and managing patients with this condition. Women are more likely to experience paraneoplastic erythema annulare centrifugum eruption, which typically precedes the clinical diagnosis of malignancy and may recur with subsequent relapses. Numerous conditions must be considered in the differential diagnosis to ensure optimal patient outcomes within an interprofessional team.
Objectives:
Identify the etiology of erythema annulare centrifugum based on patient history and physical examination.
Interpret the presentation of a patient with erythema annulare centrifugum.
Assess the management options available for erythema annulare centrifugum.
Implement care coordination to advance the evaluation and management of erythema annulare centrifugum and improve outcomes.
Introduction
Erythema annulare centrifugum is an annular, erythematous lesion that appears as urticarial-like papules, enlarges centrifugally, and clears centrally. A fine scale, called a trailing scale, is sometimes inside the advancing edge. Erythema annulare centrifugum is classified as a reactive erythema and has been associated with various underlying conditions, including malignancies. When erythema annulare centrifugum occurs as a paraneoplastic phenomenon, the lesion has been designated paraneoplastic erythema annulare centrifugum eruption. Women are more likely to experience paraneoplastic erythema annulare centrifugum eruption, which typically precedes the clinical diagnosis of malignancy and may recur with subsequent relapses.[1][2][3]
In 1881, Colcott-Fox described erythema gyratum perstans as persistent, ring-shaped lesions with pruritus. The term erythema annulare centrifugum was introduced by Darier in 1916, whereas the name erythema perstans is still used by some authors to describe similar annular erythemas. All of these previous terms refer to clinical or pathologic variants of the entity now referred to as erythema annulare centrifugum. Some dermatologists preferred distinguishing the 2 histologically different forms (superficial and deep) as superficial and deep gyrate erythema. In contrast, others believed that the superficial and deep forms were unrelated and should not be referred to by the same name.[4][5][6] Erythema annulare centrifugum is one of the three major figurative erythemas. These dermatoses exhibit advancing erythematous, annular lesions as a common presentation. However, each type possesses unique clinical and histopathological characteristics. When the other major figurate erythemas, such as erythema marginatum, erythema migrans, and erythema gyratum repens, are excluded, this is a diagnosis of exclusion.[7][8]
Etiology
Erythema annulare centrifugum is often idiopathic in origin. Nevertheless, the literature has multiple case reports that establish a link with other disorders. Eruptions frequently subside after treating the underlying condition.
Infections
Bacteria: Erythema annulare centrifugum has been associated with Escherichia coli. For example, one case involved erythema annulare centrifugum and a urinary tract infection, which resolved 3 weeks after treatment. Streptococcal infections are also linked to erythema annulare centrifugum. In addition, Mycobacterium tuberculosis is associated with erythema annulare centrifugum. The use of isoniazid, rifampin, and streptomycin successfully resolved the outbreak of erythema annulare centrifugum within 20 days of initiating tuberculosis treatment in the case of a patient.
Parasites: Ascaris lumbricoides is one of the parasites associated with erythema annulare centrifugum, and piperazine and thiabendazole treatments cleared the infection. Reports also link erythema annulare centrifugum to the Phthirus pubis infestation.
Fungi: Fungal infections associated with erythema annulare centrifugum include Candida albicans, blue cheese Penicillium, and dermatophytes, such as Trichophyton, tinea pedis, Pityrosporum orbiculare, and Malassezia furfur.
Viruses: Researchers have linked erythema annulare centrifugum to the Epstein-Barr virus in an infant and to Molluscum contagiosum in an 8-year-old child. Two cases were reported in a specific pattern that matched the distribution of recent preceding herpes zoster infections. These cases were referenced as instances of Wolf's isotopic response. An HIV-positive patient reported erythema annulare centrifugum in 2006. A case associated with SARS-CoV-2 infection in a pediatric patient has been reported. In addition, reports indicate that the SARS-CoV-2 vaccination is the secondary cause. A 42-year-old woman with a dark complexion experienced recurrent erythema annular centrifugum, which appeared to be a secondary complication of influenza type A (H1N1).[9][10][11][12][13]
Drugs
The administration of certain medications can trigger the occurrence of erythema annular centrifugum, which often resolves upon discontinuation of the drug. Drugs linked to erythema annular centrifugum include amitriptyline, azacitidine, chloroquine, hydroxychloroquine, cimetidine, estrogen, etizolam, finasteride, hydrochlorothiazide, gold sodium thiomalate, pegylated interferon alfa-2a plus ribavirin combination therapy, piroxicam, salicylates, rituximab, ustekinumab, and tocilizumab. Eruptions have also been reported with nivolumab.[14][15][16][17][18][19][20][21]
Neoplasms
Detecting unnoticed paraneoplastic erythema annulare centrifugum is crucial as it can lead to the discovery of undiagnosed cancers. In a review by Chodkiewicz et al, a total of 40 patients with malignancies associated with erythema annulare centrifugum were identified. Of the associated malignancies, 37.5% were solid tumors, and 62.5% were lymphoproliferative disorders. Eleven individuals each had leukemia and lymphoma, forming the largest association between any malignancy and erythema annulare centrifugum. Erythema annulare centrifugum resolved with successful treatment of the malignancy but relapsed with tumor recurrence in cases of Hodgkin disease, acute myelogenous leukemia, and squamous cell carcinoma in a sebaceous cyst. However, in the latter case, erythema annulare centrifugum was cleared at the terminal stage of the disease. Other reported cases include primary bronchial carcinoid, Hodgkin lymphoma, and breast cancer. The associations with paraneoplastic erythema annulare centrifugum expand to include cutaneous T-cell lymphoma. The distinction between cutaneous T-cell lymphoma–associated paraneoplastic erythema annulare centrifugum eruption and mycosis fungoides with erythema annulare centrifugum–like morphology is challenging due to the convergent clinical presentations and the nuanced histopathological characteristics of early mycosis fungoides.[22][23][24][25][26]
Additional Causes
Other causes of erythema annulare centrifugum include the following:
- Recurrent acute appendicitis
- Cholestatic liver disease
- Thyroid diseases: The eruption resolved 2 weeks after undergoing thyroid ablation with iodine-131 for Graves disease. An infrequently reported association occurs between erythema annulare centrifugum and Hashimoto thyroiditis.
- Menstruation: An instance of a woman diagnosed with erythema annulare centrifugum has been documented in which the lesions ceased to progress before menstruation but enlarged once menstruation began. Another patient experienced premenstrual exacerbations, which manifested as an autoimmune form of progesterone dermatitis.
- Hypereosinophilic syndrome: A patient presented with hypereosinophilic syndrome, characterized by a 31% increase in eosinophils, pruritus, and erythema annulare centrifugum. The treatment involved the administration of ketoconazole, dapsone, and trimethoprim-sulfamethoxazole, which resulted in the eruption's remission within 2 weeks.
- Osteoarthritis: Intra-articular hyaluronic acid injections helped eliminate left knee osteoarthritis and erythema annulare centrifugum in a patient who had reported symptoms for 11 weeks before the onset of knee osteoarthritis.
- Stress: According to a case report, stress was the triggering factor for erythema annulare centrifugum. When the patient's stress began, the lesions were exacerbated, but after those periods ended, the symptoms resolved.
- Pregnancy: A single case report details the occurrence of erythema annulare centrifugum during pregnancy, with the condition resolving shortly before childbirth. Instances where other cases improved or resolved during pregnancy are being examined.[27][28][29][30][31][32][33][34][35]
Epidemiology
The literature primarily consists of case reports and brief reviews that challenge the definition of the incidence and prevalence of erythema annulare centrifugum. Although this condition can manifest in any age group, it typically peaks in mid-adulthood, with reports of neonatal onset. No gender difference is known, and whether any ethnic predilection exists is unknown. Patients from infancy to the ninth decade of life have documented erythema annulare centrifugum. The average onset age is 40. A rare autosomal dominantly inherited form of erythema annulare centrifugum, referred to as familial annular erythema, has been described.[36]
Pathophysiology
The pathogenesis of erythema annulare centrifugum is unknown. Most cases of idiopathic erythema annulare centrifugum lack a detectable causative agent. Researchers have suggested that erythema annulare centrifugum, particularly the superficial form, may result from a hypersensitivity reaction to external or internal stimuli. Erythema annulare centrifugum has been associated with many infectious entities, particularly dermatophytes and other fungal elements, but also with viruses, parasites, and bacteria. Some foods and drugs have been implicated as additional causative factors. The literature has reported on some less common entities, including Crohn disease, pregnancy, autoimmune endocrinopathies, and hypereosinophilic syndrome.
Chodkiewicz et al proposed that the underlying malignancy must directly or indirectly elicit cytokines or antigens to stimulate the development of the dermatoses observed in cutaneous paraneoplastic syndromes. Another proposed mechanism for developing erythema annulare centrifugum involves a Th1-mediated response characterized by increased tumor necrosis factor-α and proinflammatory cytokines. This theory is supported by a case reported by Minni and Sarro, where a 57-year-old white man responded to and relapsed after discontinuation of etanercept. Hypotheses concerning the mechanism center on the interaction between inflammatory mediators and the ground substance during the transdermal diffusion of foreign antigens.[22][37]
Histopathology
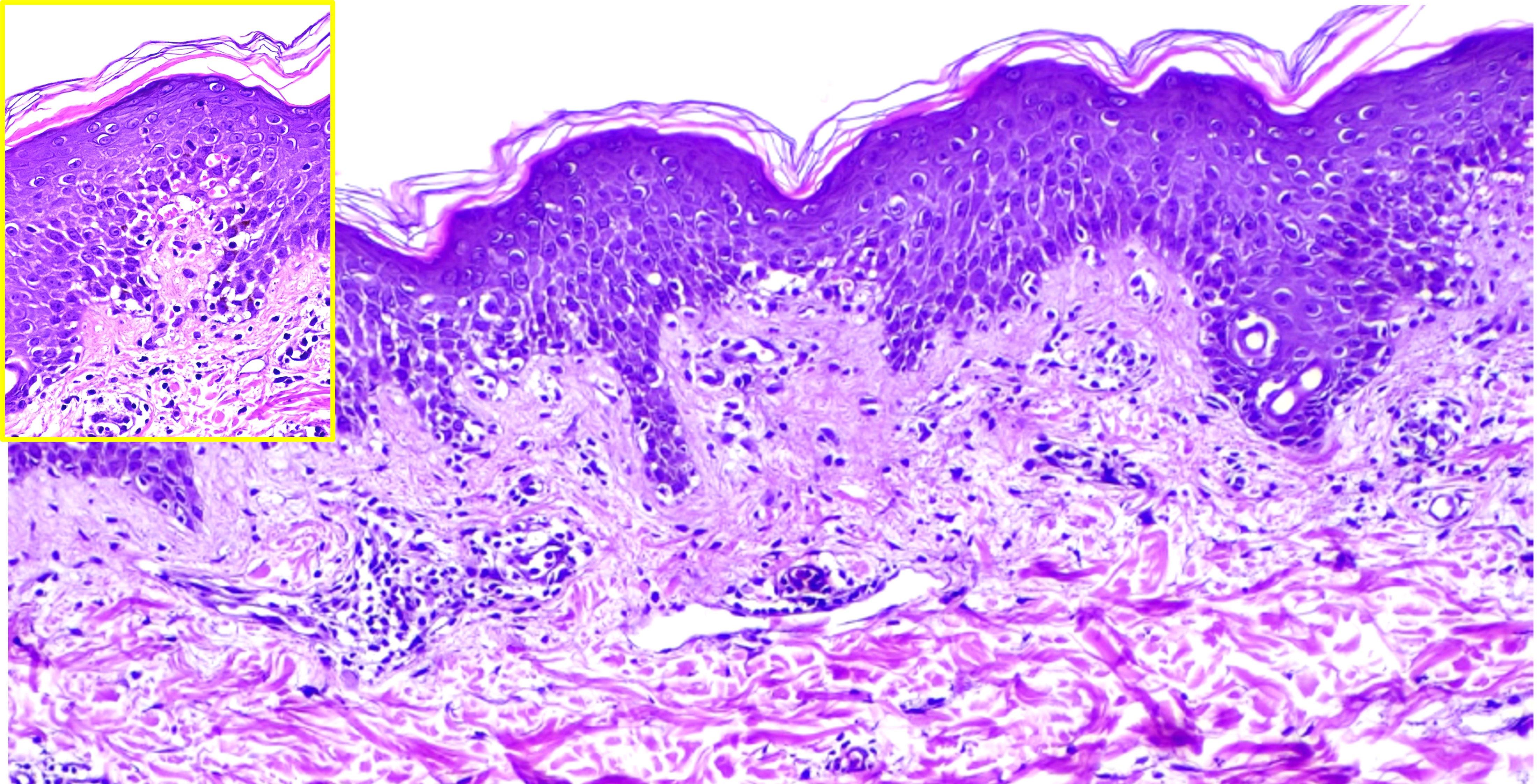
In the superficial variant of erythema annular centrifugum, an infiltrate of histiocytes, lymphocytes, and, rarely, eosinophils is present around the superficial vascular plexus vessels. The infiltrate is well-demarcated, with fairly tight aggregate around vessels, otherwise known as coat-sleeve distribution. Cells may reach into the walls of the small vessels. Erythema annulare centrifugum is considered a pseudo vasculitis rather than a vasculitis due to a lack of fibrin extravasation. The advancing edge, which is slightly raised, may also show edema in the papillary dermis. The central clearing area may contain dermal melanophages (see Image. Histopathology of Erythema Annulare Centrifugum).
In the deep variant of erythema annular centrifugum, the epidermis is typically unremarkable, and mononuclear cell infiltrates with a sharply demarcated perivascular arrangement are present primarily in the mid and lower dermis. Compared to the superficial form of erythema annulare centrifugum, the deeper dermal involvement leads to elevated and more indurated lesions lacking a trailing scale. Some dermatopathologists believe that the deep form may be a manifestation of tumid lupus. Performing a periodic acid-Schiff special stain on all biopsies is necessary to rule out dermatophytosis by identifying hyphae.
History and Physical
Typically, patients with erythema annulare centrifugum manifest with a variable-duration asymptomatic or pruritic eruption. Underlying diseases, such as tuberculosis or Hodgkin lymphoma, may cause the eruption and symptoms such as night sweats, fever, and shivers. These diseases include infection, malignancy, sarcoidosis, and other systemic illnesses. If other underlying diseases are responsible, the temporal relationship is also variable. Obtain a history of any antecedent infections. Obtain a history of the recent initiation of a new drug due to numerous reports of medication-associated erythema annulare centrifugum.
The initial lesions begin as asymptomatic, annular, or polycyclic lesions that grow slowly (2 to 3 mm per day), rarely reaching more than 10 cm in diameter, and then develop central clearing. Individual lesions can enlarge to greater than 6 cm in diameter over 1 to 2 weeks. Characteristically, a trailing scale at the inner border of the annular erythema is visualized. If the expansion of the annular plaque is not uniform, incomplete arcs appear, as do polycyclic lesions or festooned bands. Lesions are typical on the thighs and legs but may also manifest on the face, trunk, or upper extremities. The soles and palms remain unaffected. Although a localized palmar erythema annulare centrifugum has been reported, the lesions are minimally elevated in the superficial form, and desquamation occurs at the inner margin, known as the trailing scale.
The scale may not be present in all the lesions. Typically, lesions lack crusts or vesicles on their surface, but reports of atypical cases exist with telangiectasia and purpura. Occasionally, vesicles develop within the peripheral margin with associated pruritus. Lymphadenopathy may be present in cases associated with Hodgkin or non-Hodgkin lymphoma, tuberculosis, or autoimmune processes. Given the association of erythema annulare centrifugum with tuberculosis, lymphoma, sarcoidosis, and malignant bronchial carcinoid, examining the lungs is important. Erythema annulare centrifugum has been linked to appendicitis; lymphoma, with splenomegaly; liver disease, such as cholelithiasis and hepatitis; and pregnancy. Assessing the abdomen for hepatosplenomegaly, masses, or tenderness is crucial.[38]
The advancing edges are elevated in deep gyrate erythema; no associated scale or pruritus is typically apparent. No residual scarring occurs in resolving lesions, but postinflammatory hyperpigmentation is visible. Individual lesions can persist for weeks to months but without associated systemic manifestations. Researchers have described an unusual form of erythema annulare centrifugum that recurs annually, and the total duration ranges from days to decades.[39]
Evaluation
In addition to obtaining a detailed history and performing a thorough physical examination, the evaluation of the erythema annulare centrifugum includes the following steps:
- Excluding any underlying disorder that could contribute to the cutaneous manifestations. If the dermatologist suspects malignancy, an age-appropriate screening is appropriate to rule out cancer. Unfortunately, the majority of cases are idiopathic.
- If clinical suspicion of onychomycosis, tinea pedis, or tinea corporis is apparent, sending toenail clippings and skin scrapings for mycology analysis is advisable. Analyzing skin scrapings from lesional sites of erythema annulare centrifugum after potassium hydroxide (KOH) preparation can determine the presence or absence of hyphae suggestive of tinea or candidiasis.
- The Lyme antibody titer excludes erythema migrans, and serological investigations can exclude syphilis.
- An anti-nuclear antibody test should be recommended. Reports have linked Sjögren syndrome to erythema annulare centrifugum, and the differential diagnosis includes systemic lupus erythematosus.
- An anergy panel and a purified protein derivative test can be used to determine the presence of an underlying tuberculosis infection.
- A complete blood count with differential analysis can help determine whether an underlying infection is the cause.
- A stool examination may be beneficial to detect ova and parasites in the presence of an appropriate history of gastrointestinal complaints. Ascariasis has been reported in conjunction with erythema annulare centrifugum.
- Beta-human chorionic gonadotropin testing may be recommended for women.
- Chest radiography can exclude erythema annulare centrifugum if pulmonary nodules or hilar adenopathy suggest tuberculosis, malignancy (primary or metastatic), sarcoidosis, or lymphoma.
Treatment / Management
The treatment of erythema annulare centrifugum is focused on relieving any associated symptoms and resolving the clinical lesions when no underlying disorder can be identified. If the condition is associated with an underlying disorder, the cutaneous manifestations typically resolve when the underlying process has been successfully treated.
Local Therapy
Topical agents are employed to alleviate symptoms such as pruritus and to treat inflammatory lesions. Topical corticosteroids can be applied to the advancing border of the lesions. Topical antipruritics can be prescribed if associated pruritus is apparent. Two medications commonly used to treat this condition are topical corticosteroids and topical calcineurin inhibitors, specifically tacrolimus and pimecrolimus.
Systemic Therapy
For extremely symptomatic cases of erythema annulare centrifugum, such as severe pruritus, a brief course of systemic steroid therapy and sedating antihistamines may be considered. Although systemic corticosteroids can induce clinical remission, recurrences are common when the medication is discontinued. Some authors have advocated the empiric use of antibiotics or antifungals in the absence of an identifiable cause due to their association with many infectious diseases. Fluconazole, azithromycin, erythromycin, and metronidazole are some systemic drugs used to treat erythema annulare centrifugum. Etanercept has been documented to cause remission in a case of extensive erythema annulare centrifugum. Another case was cleared with upadacitinib. Idiopathic erythema annulare centrifugum has been successfully treated with doxycycline. Apremilast may represent a novel therapy for refractory erythema annular centrifugum, given the ability to upregulate interleukin 10, an anti-inflammatory cytokine that inhibits the synthesis of Th1 and Th17 cytokines. Roflumilast, a topical phosphodiesterase-4 inhibitor, successfully treated a case of erythema annulare centrifugum resistant to conventional treatments.[37][40][41][42][43][44]
Differential Diagnosis
Numerous conditions must be considered in the differential diagnosis of erythema annulare centrifugum. Patients with autoimmune diseases, including Sjögren syndrome, linear immunoglobulin A bullous dermatosis, and lupus erythematosus, specifically subacute cutaneous lupus erythematosus and tumid lupus erythematosus, can also have erythematous arciform, annular, and polycyclic lesions. Discoid eczema, chronic plaque psoriasis, seborrheic dermatitis, pityriasis rosea, porokeratosis, and sarcoidosis frequently exhibit annular scaly plaques. Less commonly, cutaneous metastases from visceral malignancies, such as stomach (inflammatory signet ring or adenocarcinoma), ovary, primary breast tumors, or malignancy of unknown primary, can mimic erythema annulare centrifugum.
Other types of annular erythema include the following:
- Erythema gyratum repens: A paraneoplastic rash presenting a characteristic wood-grain look from fast-spreading erythematous lines in a circular pattern. The difference between erythema annulare centrifugum and this condition is the delayed rate of spread (weeks as opposed to days) and the less peculiar configuration. In addition, this condition is almost always linked to an underlying malignancy.
- Necrolytic migratory erythema: Ring-shaped, red lesions that gradually blister, erode, and crust; this is typically the result of a glucagonoma.
- Erythema marginatum: A rash that manifests in acute rheumatic fever, typically circular, sharply bordered macules or pink or red papules. This nonscaling gyrate erythema is, by definition, associated with rheumatic fever in 10% to 18% of patients. The skin infiltration is neutrophilic rather than lymphohistiocytic, and the dissemination rate is quantifiable in hours.
- Erythema migrans: A growing red patch of skin that originates from a tick bite and gradually expands to cover a significant area. These lesions are frequently associated with a tick bite history (Ixodes scapularis), are fewer in number, and are less circinate in configuration.
- Erythema multiforme: Lesions appear on the backs of hands and tops of feet, but they can also occur elsewhere. These lesions consist of distinct reddish-pink macules that gradually grow into plaques. The central part of the lesions may change color or become clear, forming rings.
- Tinea (dermatophyte infection): Gradually expanding, itchy, and scaly annular lesions with central clearing.
- Granuloma annulare: A circular rash with a raised, smooth erythematous edge and a clear center.
- Secondary syphilis: This may manifest as non-itchy, scaly, annular, and polycyclic plaques. In an immunocompromised patient, Cotterman et al describe a case of syphilis that mimicked erythema annulare centrifugum and tinea imbricata.
- Subacute cutaneous lupus erythematosus: Central hypopigmentation and telangiectasias may accompany these lesions, which have a propensity to coalesce.
- Erythema papulatum centrifugum: A dermatological condition characterized by red, itchy papules that grow into circular and arc-shaped formations on the trunk and limbs. This condition is associated with sweating.[45][46]
Prognosis
The prognosis for erythema annulare centrifugum is good except for cases with underlying malignancy and other systemic diseases. The average duration of the condition is 11 months. Nevertheless, the course duration has varied from 4 to 6 weeks to 34 years in recurrent cases. Most cases resolve spontaneously without the need for treatment. When erythema annulare centrifugum is linked to an underlying neoplasm, the eruptions typically respond to the treatment of the malignancy, and the underlying condition then influences the prognosis.[39][47]
Complications
Complications are rare unless erythema annulare centrifugum is associated with an underlying condition.
Deterrence and Patient Education
Identifying and treating the root cause of erythema annulare centrifugum is critical, as is addressing a fungal infection on the skin. If associated with pregnancy, the condition typically resolves after delivery. If the dermatology consultation considers malignancy, an age-appropriate screening should rule out cancer. Unfortunately, the majority of cases are idiopathic. Case reports have reported the following benefits—topical calcipotriene, topical tacrolimus, narrowband ultraviolet B, subcutaneous etanercept, oral metronidazole, and subcutaneous interferon-alpha.[48]
Pearls and Other Issues
Erythema annulare centrifugum must be differentiated from other annular erythematous lesions, particularly annular psoriasis, and tinea corporis, when an associated scale is visualized. Additional entities include annular urticaria, annular sarcoidosis, allergic urticarial eruption, cutaneous lymphoid hyperplasia (pseudolymphoma), and mycosis fungoides. Differentiating erythema annulare centrifugum from other annular erythemas, such as erythema gyratum repens, erythema chronicum migrans, erythema marginatum, and erythema multiforme, is crucial. Erythema annulare centrifugum tends to reoccur over several months or years, although resolution can occur without treatment.
Enhancing Healthcare Team Outcomes
Several benign causes of erythema annulare centrifugum are recognized, and clinicians need to be aware that this particular skin rash is part of a paraneoplastic process. The detection of unsuspected paraneoplastic erythema annulare centrifugum is particularly crucial and may lead to the discovery of a previously undiagnosed underlying cancer. Conditions such as infections, autoimmune diseases, and drug reactions can all trigger erythema annulare centrifugum, but in some cases, it is a cutaneous marker of internal malignancies, especially lymphomas and other cancers.
Given the potentially serious implications, if there is any uncertainty about the nature of a skin eruption, a dermatology consult should be sought to ensure accurate diagnosis and management. Dermatologists can provide a more nuanced evaluation and may recommend additional diagnostic tests to rule out or confirm an underlying malignancy.
In cases where no cause is identified, treating clinicians can focus on symptom management. Topical steroids are commonly used to reduce inflammation and alleviate itching, while antihistamines can help control pruritus. These treatments can improve the patient's quality of life while further investigations are conducted to identify underlying conditions.