Introduction
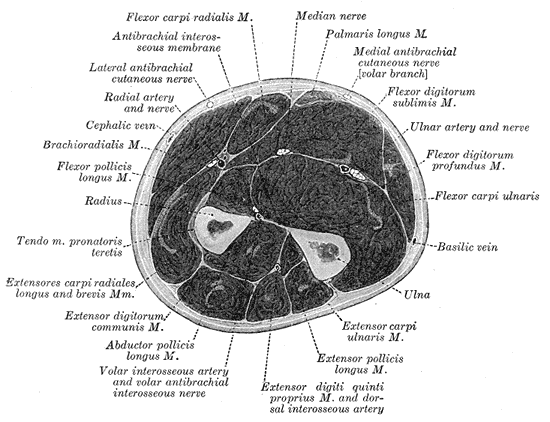
The forearm is the region of the body spanning from the elbow to the wrist. It consists of several muscles and an extensive neurovascular network encased in three compartments. These include the anterior compartment, posterior compartment, and the mobile wad. The compartments of the forearm are separated by an interosseous membrane found between the radius and ulna in addition to a lateral intermuscular septum.
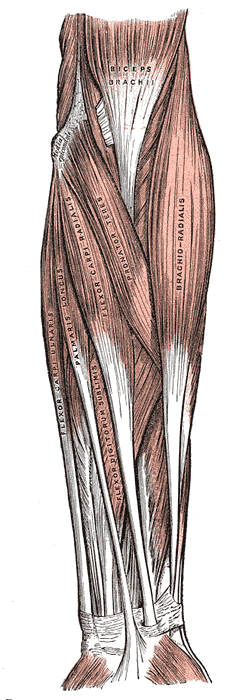
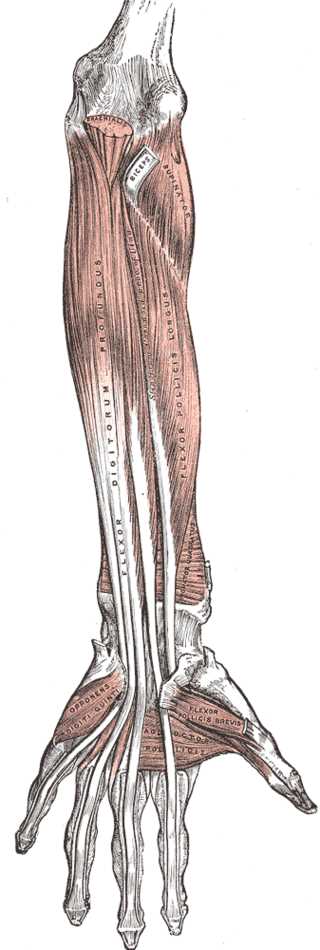
The muscles found in the posterior compartment primarily function to extend the wrists and digits. The muscles are further broken down into deep and superficial groups. The superficial group includes the extensor digitorum communis, extensor digiti minimi, extensor carpi ulnaris, and anconeus. The deep group includes the supinator, abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and extensor indicia. The mobile wad consists of three muscles: the brachioradialis, extensor carpi radialis longus, and extensor carpi radialis brevis. The anterior compartment contains muscles that act to flex the wrist and digits. The muscles are separated into deep, intermediate, and superficial groups. The superficial compartment contains the pronator teres, the flexor carpi radialis, and the flexor carpi ulnaris. The intermediate compartment contains the flexor digitorum superficially. The deep compartment of the contains the flexor digitorum profundus, flexor pollicis longus, and pronator quadratus. [1]
Structure and Function
The posterior compartment of the forearm is also known as the extensor compartment since the muscles primarily function to extend the wrist and digits of the hand. The posterior compartment of the forearm contains a superficial and deep muscle group. The superficial group includes the extensor digitorum communis, extensor digiti minimi, extensor carpi ulnaris, and anconeus. These muscles are relatively subcutaneous as there is usually not much subcutaneous fat on the dorsal aspect of the forearm. The primary function of these muscles is digit and wrist extension, with the extensor carpi ulnaris assisting in ulnar deviation of the wrist during wrist extension. The deep group contains the supinator, abductor pollicis longus, extensor pollicis brevis, and the extensor pollicis longus. The supinator functions to supinates the forearm. Supination is defined as the radius rotating laterally around its longitudinal axis over the ulna, causing the palm to face anteriorly. The remaining deep muscles function to extend and abduct the thumb.[2] The deep compartment also contains the extensor indices whose tendon lays radial to the extensor digitorium tendon to the index finger, and it assists in index finger extension. Similarly, the tendon of the extensor digiti minimi of the superficial posterior compartment travels ulnar to the extensor digitorium tendon the small finger, and assists in small finger extension.
The mobile wad contains three muscles. The brachioradialis originates over the proximal two-thirds of the lateral supracondylar ridge of the humerus, while both extensor carpi radialis longus and extensor carpi radialis brevis originate over the distal lateral supracondylar ridge. The brachioradialis inserts just proximal the radial styloid. The brachioradialis which is the strongest flexor of the forearm.[3] The extensor carpi radialis longus and extensor carpi radialis brevis insert on the second and third metacarpal base respectively. Of note, the mobile wad is occasionally included as part of the posterior compartment.
The anterior compartment is known as the flexor compartment since the muscles primarily function to flex the wrist and digits. The anterior compartment consists of a deep and superficial layer. The superficial compartment contains the pronator teres, the flexor carpi radialis, and the flexor carpi ulnaris. The palmaris longus is also present in the superficial compartment but is often absent in many people. All these muscles originate as part of the common flexor origin at the medial epicondyle. The intermediate compartment contains the flexor digitorum superficialis. The deep compartment of the contains the flexor digitorum profundus, flexor pollicis longus, and pronator quadratus. The pronator trees and pronator quadratus assist in pronation of the forearm. Pronation is defined as the radius pulling medially along its longitudinal axis over the ulna, causing the palm to face posteriorly. The carpal tunnel consists of nine tendons and the median nerve. It includes four tendons of the flexor digitorum profundus, four tendons of the flexor digitorum superficialis, and one tendon from flexor pollicis longus.
The interosseous membrane of the forearm is a Z shaped fibrous sheet that connects the radius and ulna forming a syndesmosis. The membrane divides the forearm into the anterior and posterior compartments and is the site of attachment for many muscles. Its main function is to transfer forces from the radius, ulna, and humerus. The lateral intermusclar septum is an additional structure that helps delineate the compartments of the forearm.
Embryology
The dorsolateral somite cells migrate to the upper limb around the fourth week to form the muscles of the upper limb. Many transcription factors are activated at various stages, allowing the limb buds to develop. Connective tissue derived from the lateral plate of the mesoderm divides the forearm into extensor (dorsal) and flexor (volar) compartments.
Blood Supply and Lymphatics
The forearm has a vast vascular network. The brachial artery divides at the elbow giving rise to the ulnar and radial arteries which are located along the ulnar and radial aspects of the anterior forearm compartment. The radial artery supplies the posterolateral forearm and courses lateral to the flexor carpi radialis. The ulnar artery supplies the anteromedial aspect of the forearm and gives rise to the anterior and posterior interosseous arteries which course in the deep anterior and posterior compartments respectively bringing supply to deeper structures of the forearm.
The venous drainage of the arm consists of 3 superficial veins. The dense vascular network found in the forearms drains towards these 3 main veins. The cephalic vein is found on the lateral aspect of the arm. The basilic vein is located on the medial aspect of the arm. The median cubital vein connects the two structures and is commonly found in the antecubital fossa.
The lymphatic drainage of the forearm uses a lymphatic plexus which originates on the distal extremity that flows proximally to superficial lymphatic vessels towards the axillary lymph nodes.
Nerves
Three primary nerves supply the majority of muscles in the forearm. The radial nerve and its branches supply the mobile wad of Henry and the dorsal compartment. The ulnar nerve and median nerve, and their respective branches supply the volar compartment. The radial nerve provides innervation to the anconeus, brachioradialis, and extensor carpi radialis longus.[4] The posterior interosseous nerve, a branch of the radial nerve provides innervation to the rest of the muscles in the dorsal compartment of the forearm. The ulnar nerve provides innervation to the flexor carpi ulnaris and ulnar half of the flexor digitorum profundus. The median nerve provides innervation to the palmaris longus, flexor carpi radialis, pronator teres, and flexor digitorum superficialis.[5] The anterior interosseous nerve, a branch of the median nerves supplies flexor pollicis longus, radial half of the flexor digitorum profundus, and pronator quadratus.[4]
The cutaneous nerves provide the dermatome pattern of the forearm. The lateral aspect is covered by the C5 and C6 nerve roots while the medial side is covered by the C8 and T1 nerve roots. Cutaneous nerves of the forearm include the posterior cutaneous nerve of the arm, lateral cutaneous nerve of the forearm, and medial cutaneous nerve of the forearm.
Muscles
Posterior Compartment
Superficial Muscles
Extensor digitorum communis
- Origin: lateral epicondyle of humerus
- Insertion: extensor hood of digits
- Action: extension of the wrist and extension of the MCP and IP joints of the digits
- Innervation: posterior interosseous nerve
Extensor digiti minimi
- Origin: lateral epicondyle of humerus
- Insertion: extensor hood of 5th digit
- Action: extension of the wrist and extension of MCP and IP of the 5th digit
- Innervation: posterior interosseous
Extensor carpi ulnaris
- Origin: lateral epicondyle of humerus and ulna
- Insertion: base of 5th metacarpal
- Action: extension and adduction of the wrist
- Innervation: posterior interosseous nerve
Anconeus
- Origin: lateral epicondyle of the humerus
- Insertion: lateral surface of the olecranon
- Action: extension of the forearm and stabilization of the elbow joint
- Innervation: radial nerve
Deep Muscles
Supinator
- Origin: lateral epicondyle of humerus
- Insertion: proximal radius
- Action: supination of the forearm
- Innervation: posterior interosseous nerve
Abductor pollicis longus
- Origin: ulna, radius, interosseous membrane
- Insertion: 1st metacarpal
- Action: extension of the wrist, abduction of the thumb, and extension of the CMC joint
- Innervation: posterior interosseous nerve
Extensor pollicis brevis
- Origin: radius and interosseous membrane
- Insertion: phalanx of 1st digit
- Action: extension of the wrist, extension of the thumb and the CMC joint
- Innervation: posterior interosseous nerve
Extensor pollicis longus
- Origin: ulna and interosseous membrane
- Insertion: phalanx of first digit
- Action: extension of the wrist and extension thumb at IP, MCP, and CMC joints
- Innervation: posterior interosseous nerve
Extensor indicis
- Origin: ulna and interosseous membrane
- Insertion: phalanx of first digit
- Action: extension of the wrist and extension thumb at IP, MCP, and CMC joints
- Innervation: posterior interosseous nerve
Anterior Compartment
Superficial Muscles
Pronator teres
- Origin: 2 heads; medial epicondyle via common flexor tendon and coronoid process
- Insertion: lateral radius
- Action: pronation and flexion of forearm
- Innervation: median nerve
Flexor carpi radialis
- Origin: medial epicondyle of humerus via common flexor tendon
- Insertion: base of 2nd metacarpal
- Action: flexion and abduction of the hand
- Innervation: median nerve
Flexor carpi ulnaris
- Origin: medial epicondyle of humerus via common flexor tendon and olecranon
- Insertion: isoform, hook of hamate, 5th metacarpal
- Action: flexion and adduction of the wrist
- Innervation: ulnar nerve
Palmaris longus
- Origin: medial epicondyle of humerus via common flexor tendon
- Insertion: palmar aponeurosis and flexor retinaculum
- Action: flexion of the hand
- Innervation: median nerve
Intermediate Muscles
Flexor digitorum superficialis
- Origin: two heads; medial condyle of the humerus and radius
- Insertion: middle phalanges of digits 2-5
- Action: flexion of the metacarpophalangeal and proximal interphalangeal joints of digits 2-5
- Innervation: median nerve
Deep Muscles
Flexor digitorum profundus
- Origin: ulna and interosseous membrane
- Insertion: base of phalanges
- Action: flexion DIP joints of digits
- Innervation: digits 2-3: median nerve; digits 4-5: ulnar nerve
Flexor pollicis longus
- Origin: radius and interosseous membrane
- Insertion: distal phalanx of thumb
- Action: flexion of the wrist and flexion of the MCP and IP joints of the digits
- Innervation: median nerve
Pronator quadratus
- Origin: distal ulna
- Insertion: distal radius
- Action: pronation of the forearm
- Innervation: median nerve
Mobile Wad Muscles
Brachioradialis
- Origin: lateral supracondylar ridge of humerus and lateral intermuscular septum
- Insertion: styloid process of the radius
- Action: flexion of the forearm
- Innervation: radial nerve
Extensor carpi radialis longus
- Origin: lateral supracondylar ridge of humerus
- Insertion: base of 2nd metacarpal
- Action: extension and abduction of the wrist
- Innervation: radial nerve
Extensor carpi radialis brevis
- Origin: lateral epicondyle of humerus
- Insertion: base of 3rd metacarpal
- Action: extension and abduction of the wrist
- Innervation: radial nerve
Physiologic Variants
One of the most common variations in forearm anatomy is the presence of the palmaris longus. It is present in most people but can be absent in up to 26% of individuals.[5] Additionally, when present, the palmaris longus itself can have many variations. It usually has a tendinous proximal and long tendinous distal end, and a spindle-shaped muscle belly. Cadaveric studies have shown several variations such as a reversed palmaris longus coexisting with an additional abductor digiti minimi muscle, digastric palmaris longus with intermediate muscle belly and duplication.
Martin-Gruber connection, which occurs in approximately 15 to 18% of people is just one example of the many neurovascular variations in the forearm. It involves the median nerve connecting to the ulnar nerve during its course under the flexor digitorum superficialis.[6] This cross-connection allows for median nerve innervation to some intrinsic muscles of the hand that are usually supplied by the ulnar nerve.
Surgical Considerations
Compartment syndrome of the forearm is a relatively common clinical problem, and prompt surgical intervention can be limb saving. Orthopedic, vascular and general surgeons should be familiar with surgical decompression of the forearm.
Forearm Fasciotomy A standard OR table with a hand table is preferred. Starting on the anterior forearm, an incision should begin just proximal to the wrist crease and extend proximally to the distal ulnar aspect of the elbow flexion crease. Proceed through the subcutaneous tissue and the fascia into the anterior compartment. A small nick is made in the fascia, and Mayo scissors are slid down the length of the forearm compartment releasing the compartment. Assess the deep and superficial muscles. Now mark the second radial sided anterior incision. This incision is a middorsal straight-line incision that begins 3 cm proximal to the wrist crease and extends down to the radial aspect of the elbow flexion crease. After going through the subcutaneous tissue and fascia along the entire length of the radial sided incision, finger dissect and release the posterior compartment and mobile wad. Examine all the muscles in both compartments. All nonviable necrotic tissue in any fasciotomy should be debrided. However, after the fascial releases, muscles will bulge out and even some slightly devitalized appearing muscle may recover over time. After adequate release on all three compartments has been achieved many dressing options can be explored. There are reports of good outcomes with negative pressure wound therapy, tissue expanders, wet to dry dressings.[2] The patient should be monitored and a repeat surgical irrigation and debridement in 1 to 3 days may be required prior to definitive closure.
Clinical Significance
Compartment Syndrome
Compartment syndrome is primarily a clinical diagnosis. Stryker monitoring can is an option when the clinical exam is unequivocal, or the patient is intubated and sedated. A delta pressure of less than 30 is more specific to compartment syndrome than an absolute compartment pressure of greater than 30. Delta pressure is the difference between diastolic blood pressure and compartment pressures measured by the stryker monitor. The history usually includes a swollen forearm following some form of trauma or a vascular insult. Multiple bone fractures, especially when on the ipsilateral extremity has a strong association with compartment syndrome. However, isolated fractures such as both-bone forearm fractures in adults and supracondylar humerus fractures, especially those with associated vascular injuries, in kids are frequent causes of compartment syndrome.[7] The flexor digitorum profundus and flexor pollicis longus are often injured most severely secondary to their deep location. Tense and non-compressible compartments are more specific to compartment syndrome than a softly swollen forearm. During the physical exam, it is vital to assess all three compartments, as the pathology can be limited to just one compartment. The most sensitive exam finding is a pain with passive stretch or extension of the fingers or wrist.[8] Pulselessness, paresthesias, and loss of motor function are late findings, at which point ischemic insults have already taken place.
Pronator Syndrome
The median nerve travels between the two heads of the pronator teres muscles. Based on the restrictive anatomy, the median nerve has the potential to be compressed between the two muscle heads. This commonly presents with motor weakness of the muscles innervated by the median nerve. The anterior interosseous nerve (AIN) branches off the median nerve in the forearm once the median nerve has travelled through the pronator teres. The AIN continues in the forearm to innervate muscles but lacks a sensory component. Compression of the median nerve versus the AIN can be differentiated as the median nerve contains a sensory component and therefore the patient will complain of sensory deficits. [9]
Medial Epicondylitis
Many of the muscles in the anterior compartment attach to the medial epicondyle via a common flexor tendon. Medial epicondylitis, commonly referred to as Golfer's Elbow is an overuse syndrome of the flexor mass. The condition occurs in athletes whose sports require repetitive wrist flexion and pronation. These sports include golf, baseball, and racquet sports. The inflammation can progress and cause an ulnar neuropathy. Management is typically nonoperative involving rest, ice, and pain control. [10]