[2]
Bouccara D, Rubin F, Bonfils P, Lisan Q. [Management of vertigo and dizziness]. La Revue de medecine interne. 2018 Nov:39(11):869-874. doi: 10.1016/j.revmed.2018.02.004. Epub 2018 Feb 26
[PubMed PMID: 29496272]
[3]
Post RE, Dickerson LM. Dizziness: a diagnostic approach. American family physician. 2010 Aug 15:82(4):361-8, 369
[PubMed PMID: 20704166]
[4]
Paparella MM, Djalilian HR. Etiology, pathophysiology of symptoms, and pathogenesis of Meniere's disease. Otolaryngologic clinics of North America. 2002 Jun:35(3):529-45, vi
[PubMed PMID: 12486838]
[5]
Yokose M, Shimizu T. A Case of Ramsay Hunt Syndrome That Began with Vestibular Symptoms: A Great Mimicker. The American journal of medicine. 2021 Apr:134(4):e271-e272. doi: 10.1016/j.amjmed.2020.09.049. Epub 2020 Nov 2
[PubMed PMID: 33144130]
Level 3 (low-level) evidence
[6]
Semaan MT, Megerian CA. The pathophysiology of cholesteatoma. Otolaryngologic clinics of North America. 2006 Dec:39(6):1143-59
[PubMed PMID: 17097438]
[7]
Stankovic KM, McKenna MJ. Current research in otosclerosis. Current opinion in otolaryngology & head and neck surgery. 2006 Oct:14(5):347-51
[PubMed PMID: 16974150]
Level 3 (low-level) evidence
[8]
Schneider JI, Olshaker JS. Vertigo, vertebrobasilar disease, and posterior circulation ischemic stroke. Emergency medicine clinics of North America. 2012 Aug:30(3):681-93. doi: 10.1016/j.emc.2012.06.004. Epub
[PubMed PMID: 22974644]
[9]
Mukherjee A, Chatterjee SK, Chakravarty A. Vertigo and dizziness--a clinical approach. The Journal of the Association of Physicians of India. 2003 Nov:51():1095-101
[PubMed PMID: 15260396]
[10]
Pula JH, Newman-Toker DE, Kattah JC. Multiple sclerosis as a cause of the acute vestibular syndrome. Journal of neurology. 2013 Jun:260(6):1649-54. doi: 10.1007/s00415-013-6850-1. Epub 2013 Feb 8
[PubMed PMID: 23392781]
[11]
Neuhauser HK. The epidemiology of dizziness and vertigo. Handbook of clinical neurology. 2016:137():67-82. doi: 10.1016/B978-0-444-63437-5.00005-4. Epub
[PubMed PMID: 27638063]
[12]
Neuhauser HK. Epidemiology of vertigo. Current opinion in neurology. 2007 Feb:20(1):40-6
[PubMed PMID: 17215687]
Level 3 (low-level) evidence
[13]
Johkura K. [Vertigo and dizziness]. Rinsho shinkeigaku = Clinical neurology. 2021 May 19:61(5):279-287. doi: 10.5692/clinicalneurol.cn-001570. Epub 2021 Apr 17
[PubMed PMID: 33867417]
[14]
Taylor RL, Chen L, Lechner C, Aw ST, Welgampola MS. Vestibular schwannoma mimicking horizontal cupulolithiasis. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2013 Aug:20(8):1170-3. doi: 10.1016/j.jocn.2012.08.013. Epub 2013 May 9
[PubMed PMID: 23665081]
[15]
Ribeiro BNF, Correia RS, Antunes LO, Salata TM, Rosas HB, Marchiori E. The diagnostic challenge of dizziness: computed tomography and magnetic resonance imaging findings. Radiologia brasileira. 2017 Sep-Oct:50(5):328-334. doi: 10.1590/0100-3984.2016.0054. Epub
[PubMed PMID: 29085167]
[16]
Eggers SDZ, Kattah JC. Approaching Acute Vertigo With Diplopia: A Rare Skew Deviation in Vestibular Neuritis. Mayo Clinic proceedings. Innovations, quality & outcomes. 2020 Apr:4(2):216-222. doi: 10.1016/j.mayocpiqo.2019.12.003. Epub 2020 Mar 9
[PubMed PMID: 32280933]
Level 2 (mid-level) evidence
[17]
Havia M, Kentala E, Pyykkö I. Hearing loss and tinnitus in Meniere's disease. Auris, nasus, larynx. 2002 Apr:29(2):115-9
[PubMed PMID: 11893444]
[18]
MYERS EN, BERNSTEIN JM, FOSTIROPOLOUS G. SALICYLATE OTOTOXICITY: A CLINICAL STUDY. The New England journal of medicine. 1965 Sep 9:273():587-90
[PubMed PMID: 14329630]
[19]
Büttner U, Helmchen C, Brandt T. Diagnostic criteria for central versus peripheral positioning nystagmus and vertigo: a review. Acta oto-laryngologica. 1999 Jan:119(1):1-5
[PubMed PMID: 10219377]
[20]
Kattah JC. Use of HINTS in the acute vestibular syndrome. An Overview. Stroke and vascular neurology. 2018 Dec:3(4):190-196. doi: 10.1136/svn-2018-000160. Epub 2018 Jun 23
[PubMed PMID: 30637123]
Level 3 (low-level) evidence
[21]
Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009 Nov:40(11):3504-10. doi: 10.1161/STROKEAHA.109.551234. Epub 2009 Sep 17
[PubMed PMID: 19762709]
[22]
Halker RB, Barrs DM, Wellik KE, Wingerchuk DM, Demaerschalk BM. Establishing a diagnosis of benign paroxysmal positional vertigo through the dix-hallpike and side-lying maneuvers: a critically appraised topic. The neurologist. 2008 May:14(3):201-4. doi: 10.1097/NRL.0b013e31816f2820. Epub
[PubMed PMID: 18469678]
[23]
Ulytė A, Valančius D, Masiliūnas R, Paškonienė A, Lesinskas E, Kaski D, Jatužis D, Ryliškienė K. Diagnosis and treatment choices of suspected benign paroxysmal positional vertigo: current approach of general practitioners, neurologists, and ENT physicians. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2019 Apr:276(4):985-991. doi: 10.1007/s00405-019-05313-y. Epub 2019 Jan 29
[PubMed PMID: 30694376]
[24]
Bagai A, Thavendiranathan P, Detsky AS. Does this patient have hearing impairment? JAMA. 2006 Jan 25:295(4):416-28
[PubMed PMID: 16434632]
[25]
Dorresteijn PM, Ipenburg NA, Murphy KJ, Smit M, van Vulpen JK, Wegner I, Stegeman I, Grolman W. Rapid Systematic Review of Normal Audiometry Results as a Predictor for Benign Paroxysmal Positional Vertigo. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2014 Jun:150(6):919-24. doi: 10.1177/0194599814527233. Epub 2014 Mar 18
[PubMed PMID: 24642523]
Level 1 (high-level) evidence
[26]
Vanni S, Pecci R, Edlow JA, Nazerian P, Santimone R, Pepe G, Moretti M, Pavellini A, Caviglioli C, Casula C, Bigiarini S, Vannucchi P, Grifoni S. Differential Diagnosis of Vertigo in the Emergency Department: A Prospective Validation Study of the STANDING Algorithm. Frontiers in neurology. 2017:8():590. doi: 10.3389/fneur.2017.00590. Epub 2017 Nov 7
[PubMed PMID: 29163350]
Level 1 (high-level) evidence
[27]
Shih RD, Walsh B, Eskin B, Allegra J, Fiesseler FW, Salo D, Silverman M. Diazepam and Meclizine Are Equally Effective in the Treatment of Vertigo: An Emergency Department Randomized Double-Blind Placebo-Controlled Trial. The Journal of emergency medicine. 2017 Jan:52(1):23-27. doi: 10.1016/j.jemermed.2016.09.016. Epub 2016 Oct 24
[PubMed PMID: 27789115]
Level 1 (high-level) evidence
[28]
Venosa AR, Bittar RS. Vestibular rehabilitation exercises in acute vertigo. The Laryngoscope. 2007 Aug:117(8):1482-7
[PubMed PMID: 17592393]
[29]
Cohen HS, Kimball KT. Increased independence and decreased vertigo after vestibular rehabilitation. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2003 Jan:128(1):60-70
[PubMed PMID: 12574761]
[30]
Bittar RS, Pedalini ME, Lorenzi MC, Formigoni LG. Treating vertigo with vestibular rehabilitation: results in 155 patients. Revue de laryngologie - otologie - rhinologie. 2002:123(1):61-5
[PubMed PMID: 12201005]
[31]
Tsukamoto HF, Costa Vde S, Silva RA Junior, Pelosi GG, Marchiori LL, Vaz CR, Fernandes KB. Effectiveness of a Vestibular Rehabilitation Protocol to Improve the Health-Related Quality of Life and Postural Balance in Patients with Vertigo. International archives of otorhinolaryngology. 2015 Jul:19(3):238-47. doi: 10.1055/s-0035-1547523. Epub 2015 May 6
[PubMed PMID: 26157499]
Level 2 (mid-level) evidence
[32]
Gottshall KR, Topp SG, Hoffer ME. Early vestibular physical therapy rehabilitation for Meniere's disease. Otolaryngologic clinics of North America. 2010 Oct:43(5):1113-9. doi: 10.1016/j.otc.2010.05.006. Epub
[PubMed PMID: 20713248]
[33]
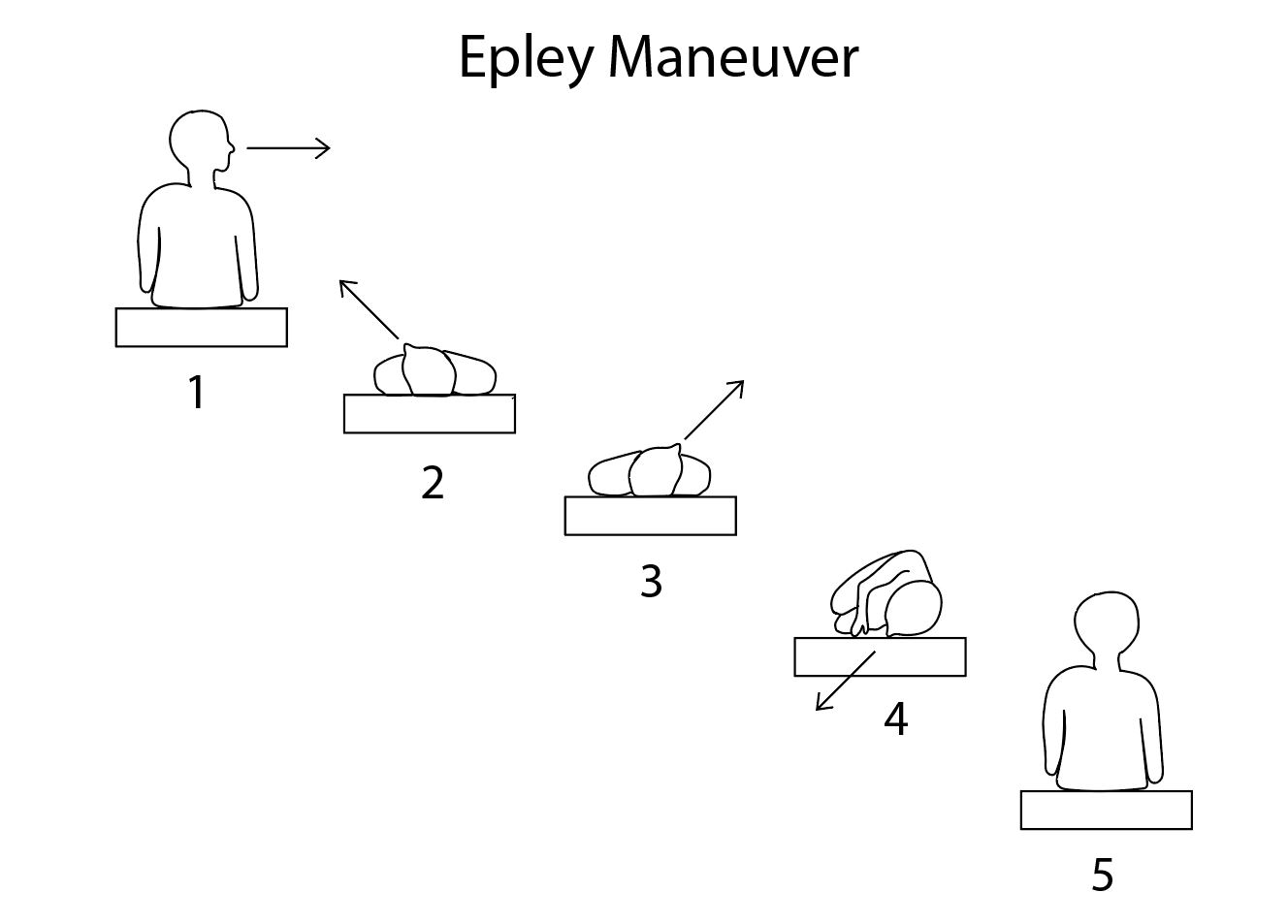
Cetin YS, Ozmen OA, Demir UL, Kasapoglu F, Basut O, Coskun H. Comparison of the effectiveness of Brandt-Daroff Vestibular training and Epley Canalith repositioning maneuver in benign Paroxysmal positional vertigo long term result: A randomized prospective clinical trial. Pakistan journal of medical sciences. 2018 May-Jun:34(3):558-563. doi: 10.12669/pjms.343.14786. Epub
[PubMed PMID: 30034415]
Level 1 (high-level) evidence
[34]
Berisavac II, Pavlović AM, Trajković JJ, Šternić NM, Bumbaširević LG. Drug treatment of vertigo in neurological disorders. Neurology India. 2015 Nov-Dec:63(6):933-9
[PubMed PMID: 26588629]
[35]
Zwergal A, Dieterich M. [Update on diagnosis and therapy in frequent vestibular and balance disorders]. Fortschritte der Neurologie-Psychiatrie. 2021 May:89(5):211-220. doi: 10.1055/a-1432-1849. Epub 2021 Apr 19
[PubMed PMID: 33873210]
[36]
Perez-Garrigues H, Lopez-Escamez JA, Perez P, Sanz R, Orts M, Marco J, Barona R, Tapia MC, Aran I, Cenjor C, Perez N, Morera C, Ramirez R. Time course of episodes of definitive vertigo in Meniere's disease. Archives of otolaryngology--head & neck surgery. 2008 Nov:134(11):1149-54. doi: 10.1001/archotol.134.11.1149. Epub
[PubMed PMID: 19015442]
[37]
Stahle J. Advanced Meniere's disease. A study of 356 severely disabled patients. Acta oto-laryngologica. 1976 Jan-Feb:81(1-2):113-9
[PubMed PMID: 1251702]
[38]
Rizvi I, Garg RK, Malhotra HS, Kumar N, Sharma E, Srivastava C, Uniyal R. Ventriculo-peritoneal shunt surgery for tuberculous meningitis: A systematic review. Journal of the neurological sciences. 2017 Apr 15:375():255-263. doi: 10.1016/j.jns.2017.02.008. Epub 2017 Feb 4
[PubMed PMID: 28320142]
Level 1 (high-level) evidence
[39]
Lee AT. Diagnosing the cause of vertigo: a practical approach. Hong Kong medical journal = Xianggang yi xue za zhi. 2012 Aug:18(4):327-32
[PubMed PMID: 22865178]
[40]
Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, Holmberg JM, Mahoney K, Hollingsworth DB, Roberts R, Seidman MD, Steiner RW, Do BT, Voelker CC, Waguespack RW, Corrigan MD. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update). Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2017 Mar:156(3_suppl):S1-S47. doi: 10.1177/0194599816689667. Epub
[PubMed PMID: 28248609]
Level 1 (high-level) evidence