[1]
Sankri-Tarbichi AG. Obstructive sleep apnea-hypopnea syndrome: Etiology and diagnosis. Avicenna journal of medicine. 2012 Jan:2(1):3-8. doi: 10.4103/2231-0770.94803. Epub
[PubMed PMID: 23210013]
[2]
Arnold WC, Guilleminault C. Upper airway resistance syndrome 2018: non-hypoxic sleep-disordered breathing. Expert review of respiratory medicine. 2019 Apr:13(4):317-326. doi: 10.1080/17476348.2019.1575731. Epub 2019 Feb 6
[PubMed PMID: 30689957]
[3]
Chervin RD, Guilleminault C. Obstructive sleep apnea and related disorders. Neurologic clinics. 1996 Aug:14(3):583-609
[PubMed PMID: 8871978]
[4]
Ogna A, Tobback N, Andries D, Preisig M, Vollenweider P, Waeber G, Marques-Vidal P, Haba-Rubio J, Heinzer R. Prevalence and Clinical Significance of Respiratory Effort-Related Arousals in the General Population. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2018 Aug 15:14(8):1339-1345. doi: 10.5664/jcsm.7268. Epub 2018 Aug 15
[PubMed PMID: 30092888]
[5]
Vizcarra-Escobar D, Duque KR, Barbagelata-Agüero F, Vizcarra JA. Quality of life in upper airway resistance syndrome. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2022 May 1:18(5):1263-1270. doi: 10.5664/jcsm.9838. Epub
[PubMed PMID: 34931609]
Level 2 (mid-level) evidence
[6]
Tufik SB, Pires GN, Palombini L, Andersen ML, Tufik S. Prevalence of upper airway resistance syndrome in the São Paulo Epidemiologic Sleep Study. Sleep medicine. 2022 Mar:91():43-50. doi: 10.1016/j.sleep.2022.02.004. Epub 2022 Feb 14
[PubMed PMID: 35255282]
[7]
Trudo FJ, Gefter WB, Welch KC, Gupta KB, Maislin G, Schwab RJ. State-related changes in upper airway caliber and surrounding soft-tissue structures in normal subjects. American journal of respiratory and critical care medicine. 1998 Oct:158(4):1259-70
[PubMed PMID: 9769290]
[8]
Sankari A, Pranathiageswaran S, Maresh S, Hosni AM, Badr MS. Characteristics and Consequences of Non-apneic Respiratory Events During Sleep. Sleep. 2017 Jan 1:40(1):. doi: 10.1093/sleep/zsw024. Epub
[PubMed PMID: 28364453]
[9]
Berry RB, Brooks R, Gamaldo C, Harding SM, Lloyd RM, Quan SF, Troester MT, Vaughn BV. AASM Scoring Manual Updates for 2017 (Version 2.4). Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2017 May 15:13(5):665-666. doi: 10.5664/jcsm.6576. Epub 2017 May 15
[PubMed PMID: 28416048]
[10]
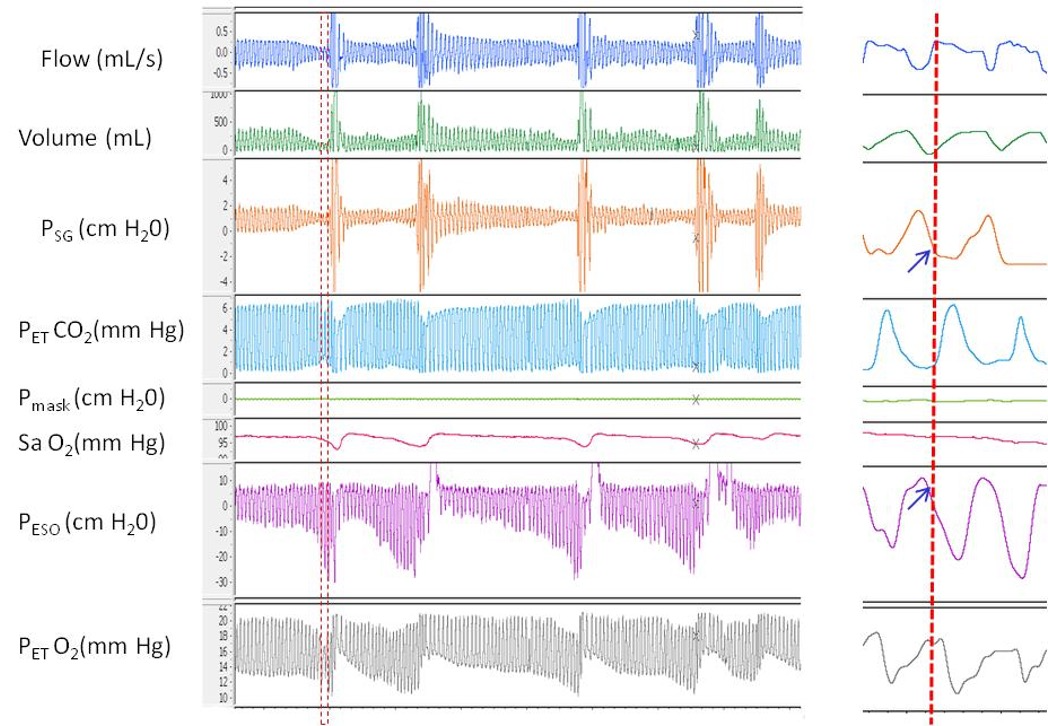
Rizwan A, Sankari A, Bascom AT, Vaughan S, Badr MS. Nocturnal swallowing and arousal threshold in individuals with chronic spinal cord injury. Journal of applied physiology (Bethesda, Md. : 1985). 2018 Aug 1:125(2):445-452. doi: 10.1152/japplphysiol.00641.2017. Epub 2018 Apr 19
[PubMed PMID: 29672224]
[11]
Alchakaki A, Riehani A, Shikh-Hamdon M, Mina N, Badr MS, Sankari A. Expiratory Snoring Predicts Obstructive Pulmonary Disease in Patients with Sleep-disordered Breathing. Annals of the American Thoracic Society. 2016 Jan:13(1):86-92. doi: 10.1513/AnnalsATS.201507-413OC. Epub
[PubMed PMID: 26630563]
[12]
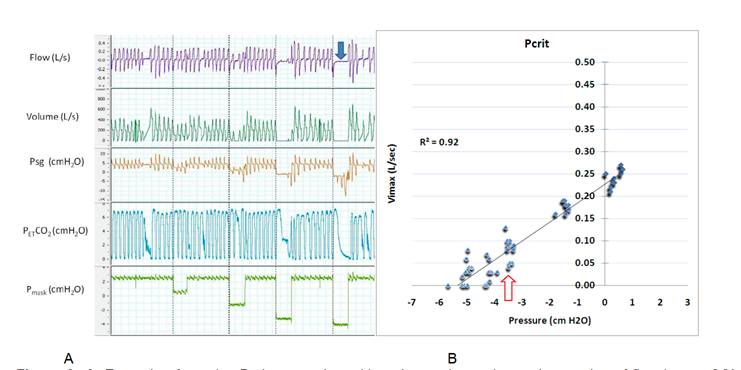
Patil SP, Schneider H, Marx JJ, Gladmon E, Schwartz AR, Smith PL. Neuromechanical control of upper airway patency during sleep. Journal of applied physiology (Bethesda, Md. : 1985). 2007 Feb:102(2):547-56
[PubMed PMID: 17008440]
[13]
Sankri-Tarbichi AG, Rowley JA, Badr MS. Expiratory pharyngeal narrowing during central hypocapnic hypopnea. American journal of respiratory and critical care medicine. 2009 Feb 15:179(4):313-9. doi: 10.1164/rccm.200805-741OC. Epub 2008 Nov 21
[PubMed PMID: 19201929]
[14]
Sankari A, Badr MS. Sleep-Disordered Breathing in Patients with Chronic Obstructive Pulmonary Disease. Annals of the American Thoracic Society. 2015 Sep:12(9):1419-20. doi: 10.1513/AnnalsATS.201506-313LE. Epub
[PubMed PMID: 26372809]
[15]
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. The New England journal of medicine. 1993 Apr 29:328(17):1230-5
[PubMed PMID: 8464434]
[16]
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE, Sinha S, Tufik S, Valentine K, Malhotra A. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. The Lancet. Respiratory medicine. 2019 Aug:7(8):687-698. doi: 10.1016/S2213-2600(19)30198-5. Epub 2019 Jul 9
[PubMed PMID: 31300334]
[17]
Cracowski C, Pépin JL, Wuyam B, Lévy P. Characterization of obstructive nonapneic respiratory events in moderate sleep apnea syndrome. American journal of respiratory and critical care medicine. 2001 Sep 15:164(6):944-8
[PubMed PMID: 11587975]
[18]
Stoohs R, Janicki J, Hohenhorst W. [Obstructive sleep apnea syndrome and upper airway resistance syndrome. Gender-related differences]. HNO. 2007 Oct:55(10):792-7
[PubMed PMID: 17287938]
[19]
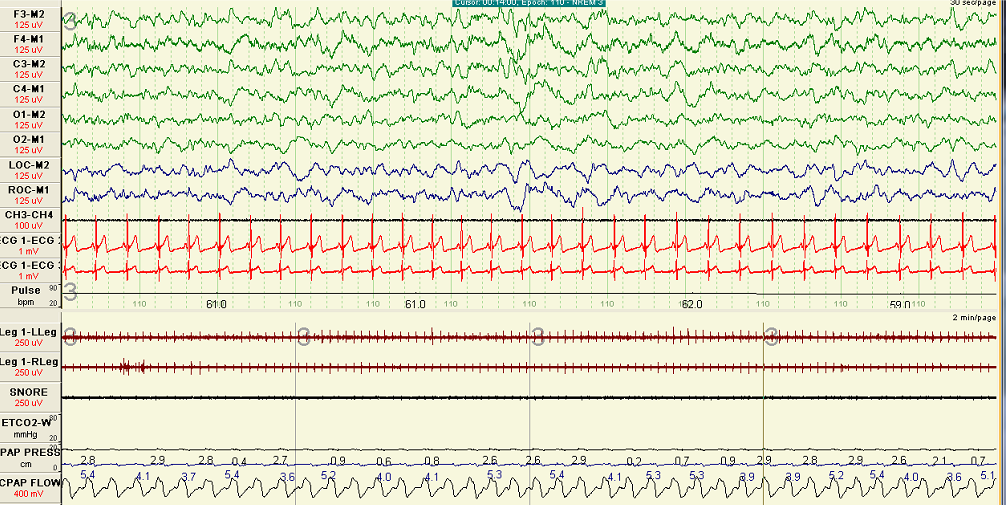
Anttalainen U, Tenhunen M, Rimpilä V, Polo O, Rauhala E, Himanen SL, Saaresranta T. Prolonged partial upper airway obstruction during sleep - an underdiagnosed phenotype of sleep-disordered breathing. European clinical respiratory journal. 2016:3():31806. doi: 10.3402/ecrj.v3.31806. Epub 2016 Sep 6
[PubMed PMID: 27608271]
[20]
Guilleminault C, Do Kim Y, Chowdhuri S, Horita M, Ohayon M, Kushida C. Sleep and daytime sleepiness in upper airway resistance syndrome compared to obstructive sleep apnoea syndrome. The European respiratory journal. 2001 May:17(5):838-47
[PubMed PMID: 11488314]
[21]
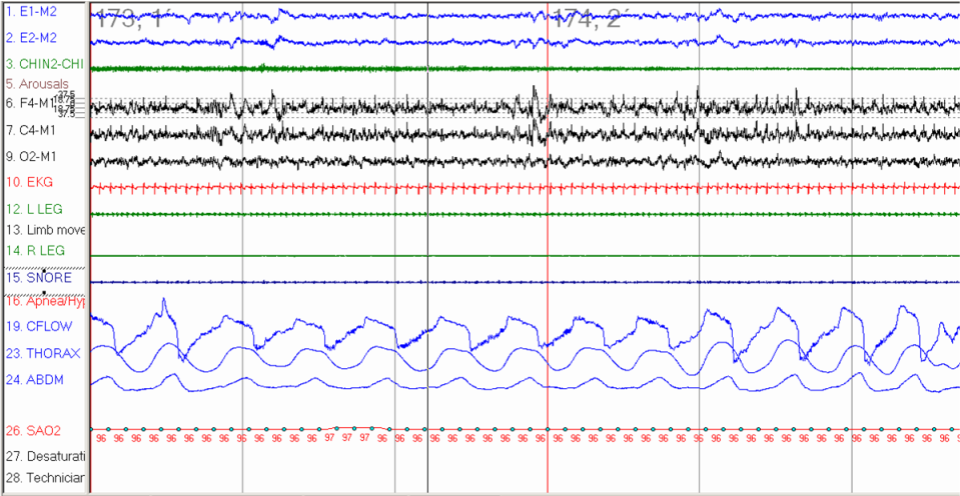
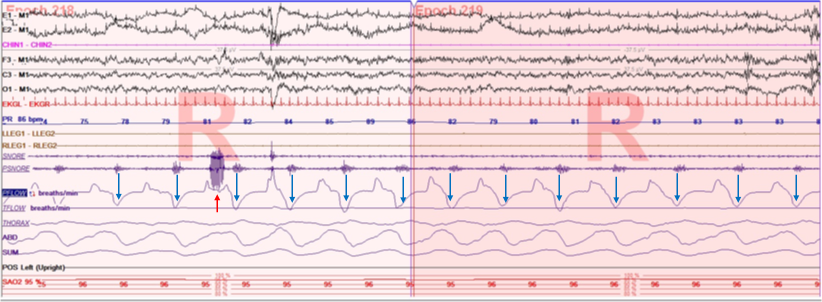
Badr MS, Zahn BR. Images in clinical medicine. Upper-airway resistance syndrome. The New England journal of medicine. 2000 May 11:342(19):1408
[PubMed PMID: 10805826]
[22]
Nerfeldt P, Friberg D. Effectiveness of Oral Appliances in Obstructive Sleep Apnea with Respiratory Arousals. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2016 Aug 15:12(8):1159-65. doi: 10.5664/jcsm.6058. Epub 2016 Aug 15
[PubMed PMID: 27397661]
[23]
de Godoy LBM, Sousa KMM, Palombini LO, Poyares D, Dal-Fabbro C, Guimarães TM, Tufik S, Togeiro SM. Long term oral appliance therapy decreases stress symptoms in patients with upper airway resistance syndrome. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2020 Nov 15:16(11):1857-1862. doi: 10.5664/jcsm.8698. Epub
[PubMed PMID: 32686643]
[24]
Newman JP, Clerk AA, Moore M, Utley DS, Terris DJ. Recognition and surgical management of the upper airway resistance syndrome. The Laryngoscope. 1996 Sep:106(9 Pt 1):1089-93
[PubMed PMID: 8822711]
[25]
Messineo L, Eckert DJ, Lim R, Chiang A, Azarbarzin A, Carter SG, Carberry JC. Zolpidem increases sleep efficiency and the respiratory arousal threshold without changing sleep apnoea severity and pharyngeal muscle activity. The Journal of physiology. 2020 Oct:598(20):4681-4692. doi: 10.1113/JP280173. Epub 2020 Aug 30
[PubMed PMID: 32864734]
[26]
Carberry JC, Grunstein RR, Eckert DJ. The effects of zolpidem in obstructive sleep apnea - An open-label pilot study. Journal of sleep research. 2019 Dec:28(6):e12853. doi: 10.1111/jsr.12853. Epub 2019 Apr 10
[PubMed PMID: 30968498]
Level 3 (low-level) evidence
[27]
Smith PR, Sheikh KL, Costan-Toth C, Forsthoefel D, Bridges E, Andrada TF, Holley AB. Eszopiclone and Zolpidem Do Not Affect the Prevalence of the Low Arousal Threshold Phenotype. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2017 Jan 15:13(1):115-119. doi: 10.5664/jcsm.6402. Epub 2017 Jan 15
[PubMed PMID: 27784413]
[28]
M'saad S, Yangui I, Feki W, Abid N, Bahloul N, Marouen F, Chakroun A, Kammoun S. [The syndrome of increased upper airways resistance: What are the clinical features and diagnostic procedures?]. Revue des maladies respiratoires. 2015 Dec:32(10):1002-15. doi: 10.1016/j.rmr.2015.08.001. Epub 2015 Oct 30
[PubMed PMID: 26525135]
[29]
Rimpilä V, Hosokawa K, Huhtala H, Saaresranta T, Salminen AV, Polo O. Transcutaneous carbon dioxide during sleep-disordered breathing. Respiratory physiology & neurobiology. 2015 Dec:219():95-102. doi: 10.1016/j.resp.2015.10.002. Epub 2015 Oct 22
[PubMed PMID: 26474829]
[30]
de Godoy LB, Palombini LO, Guilleminault C, Poyares D, Tufik S, Togeiro SM. Treatment of upper airway resistance syndrome in adults: Where do we stand? Sleep science (Sao Paulo, Brazil). 2015 Jan-Mar:8(1):42-8. doi: 10.1016/j.slsci.2015.03.001. Epub 2015 Mar 20
[PubMed PMID: 26483942]
[31]
Guilleminault C, Stoohs R, Shiomi T, Kushida C, Schnittger I. Upper airway resistance syndrome, nocturnal blood pressure monitoring, and borderline hypertension. Chest. 1996 Apr:109(4):901-8
[PubMed PMID: 8635368]
[32]
Guilleminault C, Los Reyes VD. Upper-airway resistance syndrome. Handbook of clinical neurology. 2011:98():401-9. doi: 10.1016/B978-0-444-52006-7.00026-5. Epub
[PubMed PMID: 21056201]