Definition/Introduction
Trendelenburg sign is a physical examination finding seen when assessing for any hip dysfunction. A positive Trendelenburg sign usually indicates weakness in the hip abductor muscles, which consists of the gluteus medius and gluteus minimus. A contralateral pelvic drop during a single-leg stance defines a positive sign. Named after a German surgeon, Friedrich Trendelenburg, the Trendelenburg sign was first described in 1897 to identify hip abductor weakness in individuals with congenital dislocation of the hip and progressive muscular atrophy.[1]
Anatomy/Physiology
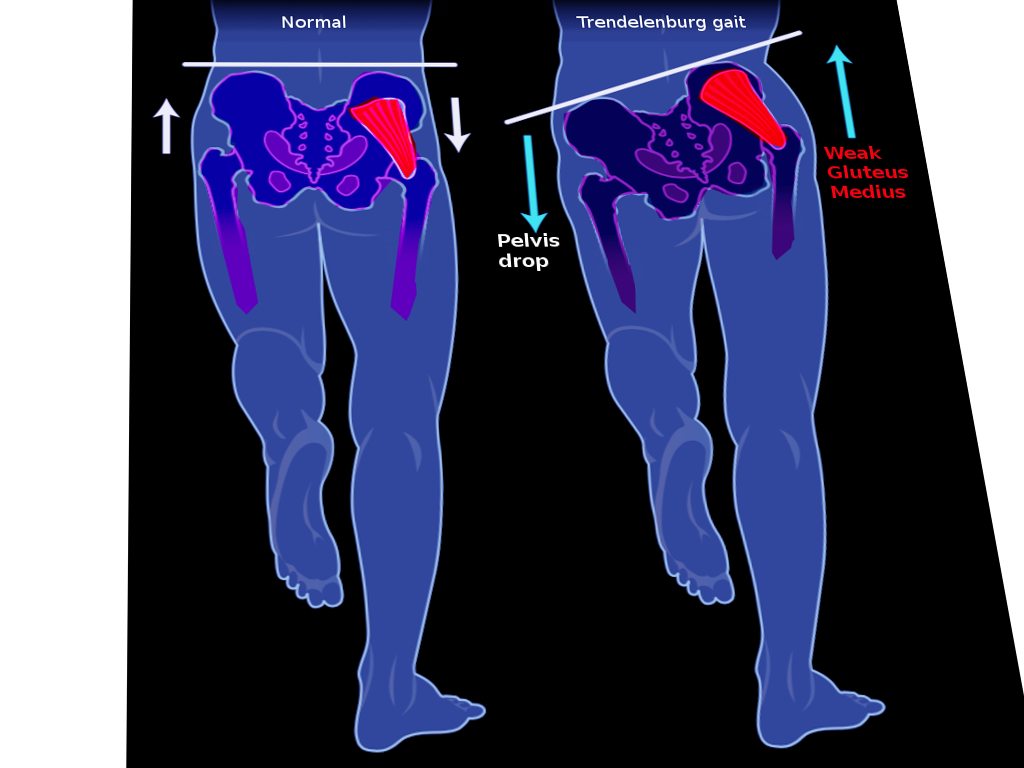
Gluteus medius and minimus muscles are the primary abductors of the hip. These muscles are essential in stabilizing the hip and pelvis to maintain a mid-line center of gravity. Both muscles receive innervation from the superior gluteal nerve from contributions from the L4-S1 nerve roots.[2] The muscle function can become compromised through several etiologies, some of which are listed below. A few etiologies include damage to the nerve resulting in hip dislocation, diseases such as poliomyelitis, avulsion of muscle ligaments from their distal attachment to the femur, fractures, etc.[3] The Trendelenburg sign is most apparent during the gait cycle (see Image. Trendelenburg Gait). The pelvis rises ipsilaterally when the leg supports the body's weight on the lesioned side. This presentation is more accurately dipping the pelvis towards the contralateral side. Because the lesioned abductors cannot maintain the pelvis in a level plane, the patient falls towards the good side and simultaneously leans the torso towards the lesioned side to maintain balance. This type of gait is known as the Trendelenburg gait.
Methods of Evaluation
Prerequisites of Testing
- The patient can stand on the affected side for more than 30 seconds
- The patient can understand commands
- The patient has intact coordination
- The patient has free abduction movement; no fixed adduction deformity
Standing Test
The patient stands on the affected leg in a single-leg stance for up to 30 seconds. The provider stands behind the patient at the hip level and places their hands on the iliac crests on either side of the pelvis, observing if it stays level during the single-leg stance. Repeat the test on the opposite side. A positive Trendelenburg sign is when the pelvis drops on the unaffected side.[4]
Gait Test
The examiner asks the patient to walk a short distance. In a normal gait, the body shifts the weight to the stance leg, allowing the center of gravity to shift, stabilizing the body. In a patient with a positive Trendelenburg sign constituting abductor weakness, when they lift the unaffected leg, the shift does not occur; therefore, the patient is unable to maintain balance, leading to instability.
Bottom Line
The Trendelenburg sign alone cannot diagnose hip conditions, but it is essentially a physical exam assessment used to aid in the diagnosis of various hip pathologies. A health care provider should still complete a full history and physical and order appropriate lab and imaging tests to assist in the final diagnosis, contributing to a positive Trendelenburg sign. Other diagnostic tests can include X-rays, ultrasonography, computed tomography scans, and magnetic resonance imaging to diagnose the primary condition.
Issues of Concern
The Trendelenburg sign is useful in assessing different hip dysfunctions, but the interpretation of the results remains controversial as there is no established standard for a positive test. According to Bailey et al, only 2 authors have objectively defined the point at which pelvic drop can be considered a positive Trendelenburg test result: Asayama et al established a positive Trendelenburg test result as a pelvic tilt angle of greater than 2 degrees, while Westhoff et al (2005) considered “positive” to be a pelvic drop in the non-stance limb during the single-stance phase of over 4 degrees or a maximum pelvic drop in the stance phase exceeding 8 degrees (Bailey et al, 2009).[1][5] In recent years, the Hardcastle modification of the Trendelengberg test (described above) has helped to eliminate false positives.
False positives can occur with:
- Obesity
- Fixed adduction deformity
- Medialization of lower limb axis, such as coxa vara, genu varum, and malunited supracondylar femur with varus deformity
- Non-intact quadratus lumborum (pulls the pelvis on the unaffected side up if it is not intact)
- Pain
- Poor balance
- Lack of cooperation or understanding
- Costo-pelvic impingement
- Scoliosis
- Pelvic drop can occur even in healthy individuals with normal abductor mechanisms when the abductor muscles are not working adequately.
False negatives can occur with:
- Use of supra-pelvic muscles
- Use of psoas and rectus femoris
- Wide lateral translocation of the trunk to allow balance over the hip as a fulcrum
- In patients with early stages of osteonecrosis, despite having an abductor mechanism defect, Trendelenburg sign and, therefore, gait remain masked.[6]
Clinical Significance
The Trendelenburg sign is useful in identifying weak hip abductors and assessing other mechanical, neurological, and spinal disorders. Especially in the postoperative setting, a positive Trendelenburg sign may identify the source of patient complications. Particularly in the posterior approach to the hip, the gluteus medius is likely to be detached from its attachment at the greater trochanter. Therefore, orthopedic surgeons must be careful in their surgical approach to avoid this complication.
A positive Trendelenburg test is a finding in the following [7]:
- Any condition that brings the origin and insertion of gluteus medius together:
- Subluxation or dislocation of the hip
- Coxa vara
- Greater trochanter fractures
- Slipped femoral capital epiphysis
- Legg-Calve-Perthes disease
- Abductor paralysis or weakness:
- Polio
- Root-lesion
- Post-operative nerve damage
- Muscle-wasting disease
- Hemiplegic cerebral palsy
- Muscular dystrophy
- Any painful hip disorder that results in gluteal inhibition
- Others
- Lower back pain
- Osteoarthritis of the hip
- Greater trochanter fractures
- Femoral neck fractures
- Short leg syndrome
- The initial time following total hip replacement
- Cleidocranial dysostosis
Nursing, Allied Health, and Interprofessional Team Interventions
A patient-centered approach to care is necessary to manage and treat a patient with a positive Trendelenburg sign. A team of health care workers, including the patient’s primary care physician, specialists like orthopedics and neurologists, nurses, physical therapists, or chiropractors, all working in an interdisciplinary manner with the patient, can help find the root cause and treat the patient. Often, patients must follow up with their physical therapists and other doctors to manage their condition long-term, as it takes time to recover fully, depending on the diagnosis.
Management
Medical management of a positive Trendelenburg sign depends on the underlying cause. If the positive Trendelenburg sign is the result of pain, providers might suggest pain control through the use of over-the-counter nonsteroidal anti-inflammatory drugs. In severe cases, doctors might prescribe steroids such as cortisone injections to help reduce pain. If the patient has short leg syndrome, patients might benefit from a shoe lift to minimize the waddling gait. Other times, the clinician might suggest a harness for developmental dysplasia of the hip or a cast for Legg Calve Perthes disease. Physical therapists often recommend various exercises to strengthen the hip abductors so that the patient can maintain a midline center of gravity, preventing side-to-side motion during their gait cycle. Osteopathic manipulative treatment could result in improved gait and range of motion for individuals with somatic dysfunctions, short-leg syndrome, and lower back pain, contributing to positive Trendelenburg sign.[8] Biofeedback, through electromyography, can help patients understand how their muscles respond to specific movements and adjust their gait accordingly. This allows patients to control their muscle movements and increase their range of motion.[9]