Introduction
The tensor fasciae latae (TFL) is a muscle of the proximal anterolateral thigh that lies between the superficial and deep fibers of the iliotibial (IT) band. There is high variability in muscle belly length, although, in most patients, the TFL muscle belly ends before the greater trochanter of the femur. The TFL works in conjunction with the gluteus maximus, gluteus medius, and gluteus minimus in various hip movements, including flexion, abduction, and internal rotation. This muscle acts via the iliotibial (IT) band's attachment to the tibia to assist with knee flexion and lateral rotation. The TFL is most important clinically for assisting pelvic stability while standing and walking.[1][2][3]
Structure and Function
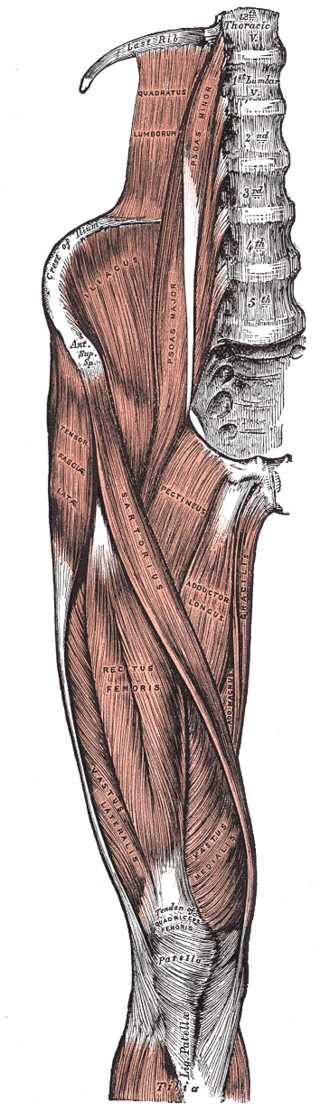
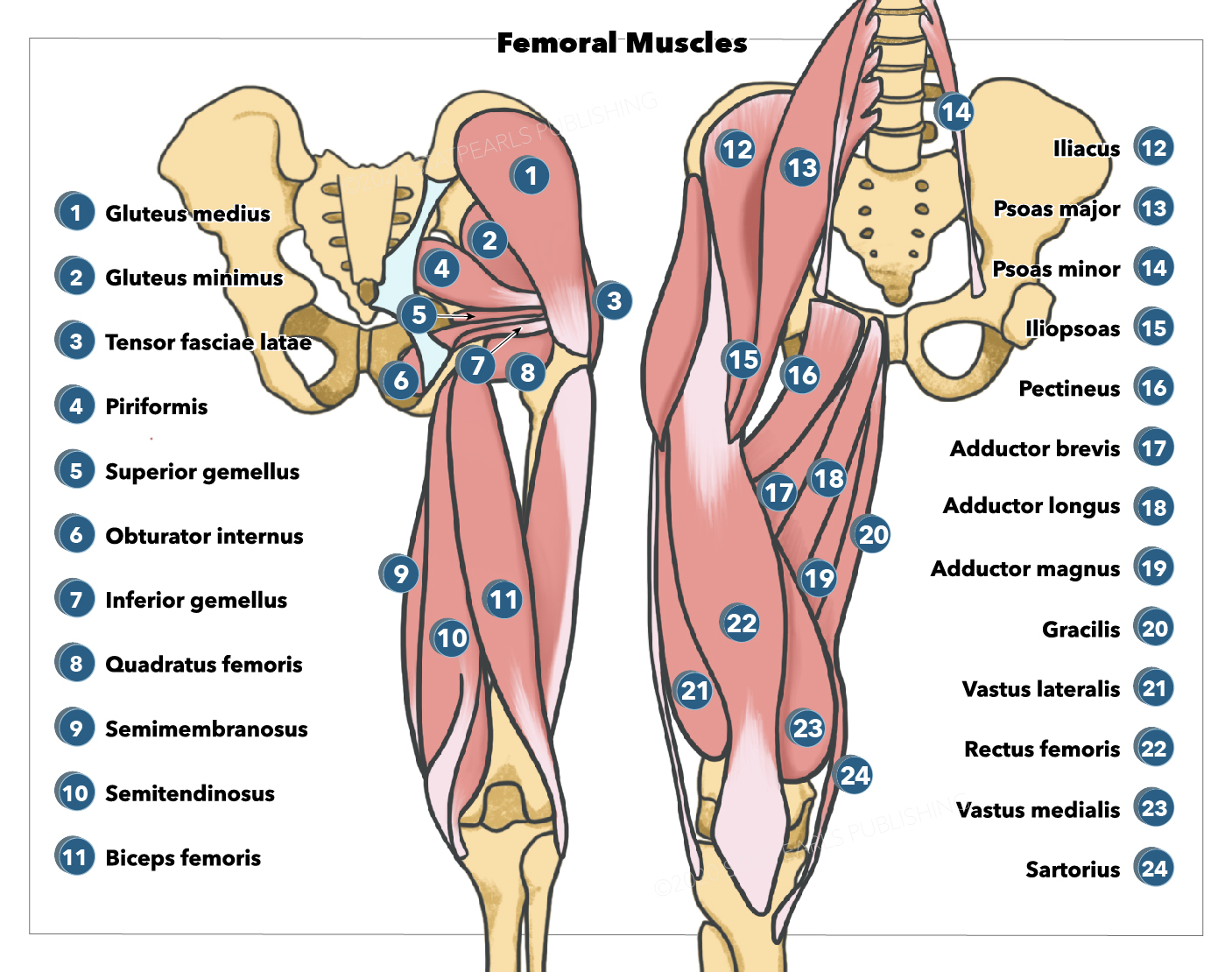
The TFL originates from the anterior superior iliac spine (ASIS) and the anterior aspect of the iliac crest and descends between and is attached to the deep fascia and the superficial fascia of the IT band. The TFL descends on the anterolateral aspect over the thigh, running superficially to the greater trochanter of the femur. The TFL inserts distally to the IT track/band, which is comprised of the fascial aponeurosis of the gluteus maximus and the tensor fascia latae. The IT band then runs along the lateral aspect of the thigh, where it attaches to the lateral condyle of the tibia, specifically the Gerdy tubercle.
Though small in size, the TFL works with several muscle groups to assist in the movement and stabilization of both the hip and the knee. This muscle works synergistically with the gluteus medius and gluteus minimus to internally rotate and abduct the hip and with the gluteus maximus via the IT band to abduct the hip. It assists the rectus femoris in the flexion of the hip.
The TFL acts on the tibia via the IT band's attachment to the Gerdy tubercle of the lateral tibia. The TFL is an accessory knee flexor, though its action is only seen once the knee is flexed beyond 30 degrees. Furthermore, the TFL works with the IT band to stabilize the knee in full extension. The TFL also acts via the IT band in the lateral rotation of the tibia. This lateral rotation may be performed while the hip is in the abduction and medial rotation, as is seen when kicking a soccer ball.
Clinically, the primary function of the TFL is to assist in walking. The TFL does this by pulling the ilium inferiorly on the weight-bearing side, causing the contralateral hip to rise. The rise in the non–weight-bearing hip allows the leg to swing through without hitting the ground during the swing phase of the gait.[4]
Embryology
The TFL is a skeletal muscle. The paraxial mesoderm, which creates somitomeres in the head and composes somites from the occipital to the sacral areas, leads to the formation of skeletal muscles.[5] During embryological differentiation, the myoblasts (precursor cells) fuse and compose long multinucleated muscle fibers. In the cytoplasm, myofibrils are present, and cross-striations appear by the endpoint of the third month. Tendon, which eventually will connect the TFL to the Gerdy tubercle of the tibia, is yielded from sclerotome cells lying adjacent to myotomes at borders of somites (both anterior and posterior).
SCLERAXIS, a type of transcription factor, regulates the development of tendons. Lateral plate mesodermal fibroblast growth factors and bone morphogenetic protein 4 (BMP4), working in coordination with WNT proteins from adjacent ectoderm, signal the dermomyotome VLL cells to express the muscle-specific gene MyoD. BMP4 induces the production of WNT proteins via the dorsal neural tube. Meanwhile, the low osmolarity of sonic hedgehog (SHH) proteins, secreted by the floor plate of the neural tube and the notochord, reach the dermomyotome DML cells. These expressions lead to the endocellular induction of MYF5 and MyoD. Both MyoD and MYF5 are in the family of myogenic regulatory factors (MRFs), which are transcription factors that activate TFL and other muscular development pathways.[6]
Blood Supply and Lymphatics
The deep branch of the superior gluteal artery supplies the TFL. The superior gluteal artery is the largest branch of the posterior division of the internal iliac artery; it runs posteriorly between the lumbosacral trunk and the first sacral nerve root. The superior gluteal artery exits the pelvis via the greater sciatic foramen, where it divides into superficial and deep branches. The deep branch travels between the gluteus minimus and gluteus medius to supply those muscles and the TFL.
Nerves
The TFL is innervated by the superior gluteal nerve, L4, L5, and S1. The superior gluteal nerve is formed from the anterior rami of L4-S1 and runs with the superior gluteal artery and vein, passing superior to the piriformis before exiting the pelvis through the greater sciatic foramen. This nerve runs anterior to the gluteus maximus muscle before ending at the gluteus minimus and TFL muscles.
Physiologic Variants
Though the TFL typically terminates before the greater trochanter, in approximately one-third of patients, the TFL can extend distally to the greater trochanter. This is clinically significant as the TFL fibers must be split when performing a lateral approach to the proximal femur in those patients.
Surgical Considerations
In orthopedics, there are 4 basic surgical approaches to the hip joint: the anterior, anterolateral, posterior, and medial. The TFL is used as a surgical landmark in anterior and anterolateral approaches. The anterior approach to the hip is performed using the internervous plane between the sartorius (femoral nerve) and the TFL (superior gluteal nerve). The anterolateral approach to the hip uses the intermuscular plane between the TFL and gluteus medius. Since the gluteus medius and TFL are both innervated by the superior gluteal nerve, this approach has no true internervous plane. However, the superior gluteal nerve enters the TFL very close to its origin at the iliac crest. Therefore, as long as the surgical plane is not extended proximally to the TFL insertion, the nerve will remain out of the surgical field and safe.[7][8][9]
In reconstructive surgery, the TFL can be used for soft tissue coverage. Case of the TFL being used for local flaps, regional flaps, and free flaps have been reported. Due to its small size, the TFL is not often the first choice for free flaps, but there are case reports of using TFL free flaps when latissimus dorsi and rectus abdominis flaps are unavailable. When a large area needs coverage, the TFL can be used in conjunction with an anterolateral thigh flap by using the lateral circumflex system of the femoral vessels.[10][11]
Clinical Significance
The TFL can become clinically significant in cases of tightening, friction between or over bony prominences, or through its attachment to the IT band. The TFL can become tight, especially in situations of prolonged shortening, such as in a seated position. A shortened TFL can lead to an anterior tilt of the pelvis and/or medial rotation of the femur.
External snapping hip syndrome is a condition where patients describe a palpable snap on the lateral aspect of their hip that occurs with various movements. Though this syndrome has multiple etiologies, the most common etiology is due to the IT band moving over the greater trochanter. This is thought to be due to a thickening of the posterior band of the IT fascia. Though patients will often not complain of pain from this syndrome, it can progress to become painful. Treatment is typically conservative with oral NSAIDs and physical therapy.
IT band syndrome is a common overuse injury observed in runners and cyclists. Patients describe lateral-sided knee pain. The etiology of IT band syndrome is controversial, although many authors agree the etiology can be divided into three main categories:
- IT band friction over the lateral femoral epicondyle
- Compression of the fat and connective tissue deep to the ITB
- Chronic inflammation of the IT band bursa
Treatment of IT band syndrome is conservative, starting with NSAIDs, physical therapy, and possibly a corticosteroid injection.[12]
Older patients often experience weakened TFL actions due to vitamin B12 deficiency.[13] Vitamin B12 deficiency typically leads to nerve demyelination within the CNS and the PNS. Demyelination eventually leads to large fiber (type A) peripheral neuropathy and causes weakness in the lower extremities. As type A fibers work with sensory and motor nerve function, TFL-based hip flexion is compromised.