[1]
Garfein E, Doscher M, Tepper O, Gill J, Gorlick R, Smith RV. Reconstruction of the pediatric midface following oncologic resection. Journal of reconstructive microsurgery. 2015 Jun:31(5):336-42. doi: 10.1055/s-0035-1544181. Epub 2015 Mar 24
[PubMed PMID: 25803408]
[2]
Li D, Xu F, Zhang R, Zhang Q, Xu Z, Li Y, Wang C, Li T. Surgical Reconstruction of Traumatic Partial Ear Defects Based on a Novel Classification of Defect Sizes and Surrounding Skin Conditions. Plastic and reconstructive surgery. 2016 Aug:138(2):307e-316e. doi: 10.1097/PRS.0000000000002408. Epub
[PubMed PMID: 27465192]
[3]
Marks MW, Friedman RJ, Thornton JW, Argenta LC. The temporal island scalp flap for management of facial burn scars. Plastic and reconstructive surgery. 1988 Aug:82(2):257-61
[PubMed PMID: 3399556]
[4]
Jose A, Nagori SA, Arya S, Roy ID. Chimeric temporopareital osteofascial and temporalis muscle flap; a novel method for the reconstruction of composite orbito-maxillary defects. Journal of stomatology, oral and maxillofacial surgery. 2019 Jun:120(3):250-254. doi: 10.1016/j.jormas.2019.02.002. Epub 2019 Feb 11
[PubMed PMID: 30763779]
[5]
Denadai R, Raposo-Amaral CE, Marques FF, Raposo-Amaral CA. Posttraumatic eyebrow reconstruction with hair-bearing temporoparietal fascia flap. Einstein (Sao Paulo, Brazil). 2015 Jan-Mar:13(1):106-9. doi: 10.1590/S1679-45082015RC2834. Epub 2015 Mar 3
[PubMed PMID: 25993077]
[6]
Schreiber M, Dragu A. Free temporal fascia flap to cover soft tissue defects of the foot: a case report. GMS Interdisciplinary plastic and reconstructive surgery DGPW. 2015:4():Doc01. doi: 10.3205/iprs000060. Epub 2015 Jan 13
[PubMed PMID: 26504730]
Level 3 (low-level) evidence
[7]
Olcott CM, Simon PE, Romo T 3rd, Louie W. Anatomy of the superficial temporal artery in patients with unilateral microtia. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2019 Jan:72(1):114-118. doi: 10.1016/j.bjps.2018.09.001. Epub 2018 Sep 28
[PubMed PMID: 30528867]
[8]
Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plastic and reconstructive surgery. 1976 Jul:58(1):80-8
[PubMed PMID: 935283]
[9]
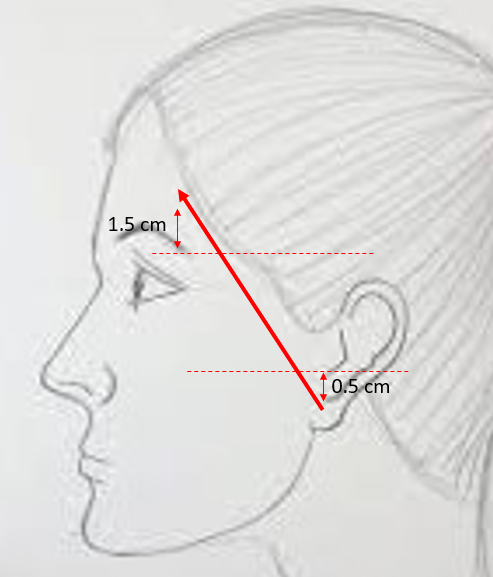
Pitanguy I, Ramos AS. The frontal branch of the facial nerve: the importance of its variations in face lifting. Plastic and reconstructive surgery. 1966 Oct:38(4):352-6
[PubMed PMID: 5926990]
[10]
Schmidt BL, Pogrel MA, Hakim-Faal Z. The course of the temporal branch of the facial nerve in the periorbital region. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2001 Feb:59(2):178-84
[PubMed PMID: 11213986]
[11]
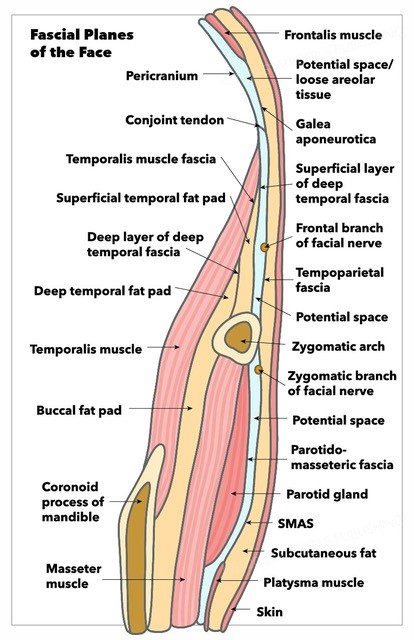
Trinei FA, Januszkiewicz J, Nahai F. The sentinel vein: an important reference point for surgery in the temporal region. Plastic and reconstructive surgery. 1998 Jan:101(1):27-32
[PubMed PMID: 9427913]
[12]
Safavi-Abbasi S, Komune N, Archer JB, Sun H, Theodore N, James J, Little AS, Nakaji P, Sughrue ME, Rhoton AL, Spetzler RF. Surgical anatomy and utility of pedicled vascularized tissue flaps for multilayered repair of skull base defects. Journal of neurosurgery. 2016 Aug:125(2):419-30. doi: 10.3171/2015.5.JNS15529. Epub 2015 Nov 27
[PubMed PMID: 26613175]
[13]
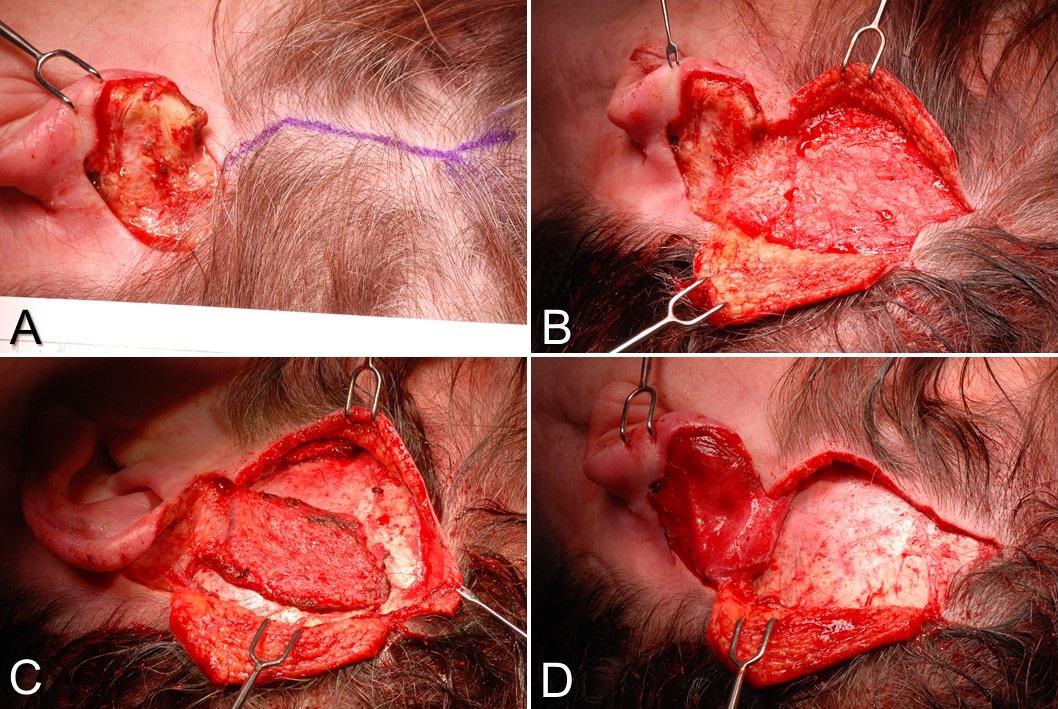
Mokal NJ, Ghalme AN, Kothari DS, Desai M. The use of the temporoparietal fascia flap in various clinical scenarios: A review of 71 cases. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India. 2013 Sep:46(3):493-501. doi: 10.4103/0970-0358.121988. Epub
[PubMed PMID: 24459337]
Level 3 (low-level) evidence
[14]
Jaquet Y, Higgins KM, Enepekides DJ. The temporoparietal fascia flap: a versatile tool in head and neck reconstruction. Current opinion in otolaryngology & head and neck surgery. 2011 Aug:19(4):235-41. doi: 10.1097/MOO.0b013e328347f87a. Epub
[PubMed PMID: 21593668]
Level 3 (low-level) evidence
[15]
Collar RM, Zopf D, Brown D, Fung K, Kim J. The versatility of the temporoparietal fascia flap in head and neck reconstruction. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2012 Feb:65(2):141-8. doi: 10.1016/j.bjps.2011.05.003. Epub 2011 Jun 22
[PubMed PMID: 21700520]
[18]
Rubinstein RY, Rosen A, Leeman D. Frey syndrome: treatment with temporoparietal fascia flap interposition. Archives of otolaryngology--head & neck surgery. 1999 Jul:125(7):808-11
[PubMed PMID: 10406323]
[19]
Movassaghi K, Lewis M, Shahzad F, May JW Jr. Optimizing the Aesthetic Result of Parotidectomy with a Facelift Incision and Temporoparietal Fascia Flap. Plastic and reconstructive surgery. Global open. 2019 Feb:7(2):e2067. doi: 10.1097/GOX.0000000000002067. Epub 2019 Feb 8
[PubMed PMID: 30881826]
[20]
Hing DN, Buncke HJ, Alpert BS. Use of the temporoparietal free fascial flap in the upper extremity. Plastic and reconstructive surgery. 1988 Apr:81(4):534-44
[PubMed PMID: 3347663]
[21]
Upton J, Rogers C, Durham-Smith G, Swartz WM. Clinical applications of free temporoparietal flaps in hand reconstruction. The Journal of hand surgery. 1986 Jul:11(4):475-83
[PubMed PMID: 3722753]
[22]
Mavropoulos JC, Bordeaux JS. The temporoparietal fascia flap: a versatile tool for the dermatologic surgeon. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2014 Sep:40 Suppl 9():S113-9. doi: 10.1097/dss.0000000000000114. Epub
[PubMed PMID: 25158871]
[23]
Yano H, Fukui M, Yamada K, Nishimura G. Endoscopic harvest of free temporoparietal fascial flap to improve donor-site morbidity. Plastic and reconstructive surgery. 2001 Apr 1:107(4):1003-9
[PubMed PMID: 11252096]