Etiology
Tachycardia can have physiological or pathological causes. Physiologically it is commonly associated with catecholaminergic triggers, including exercise, stress, pain, and anxiety.[2] Pathologically, there are cardiac and non-cardiac etiologies as summarized below:
Cardiac etiologies:
*Supraventricular tachycardia is an arrhythmia originating above the ventricles as demonstrated by a narrow QRS complex on an electrocardiogram. If the rhythm is regular, atrial flutter, atrioventricular reentrant tachycardia (AVRT), atrioventricular nodal reentrant tachycardia (AVNRT), atrial tachycardia, or sinus tachycardia are the common etiologies. If the rhythm is irregular atrial fibrillation, atrial tachycardia with variable block, atrial flutter with variable block, multifocal atrial tachycardia, or frequent premature atrial contractions should merit consideration.[5]
*Ventricular tachycardia is is an arrhythmia that originates in the ventricles as demonstrated by a wide QRS on an electrocardiogram. It can be nonsustained (lasting less than 30 seconds or sustained (lasting greater than 30 seconds or with associated hemodynamic instability). Additionally, if the QRS morphology is stable, it is classified as monomorphic, and if the PRS morphology is variable, it classifies as polymorphic.[6]
*Torsades de pointes is a characteristic form of polymorphic ventricular tachycardia that results from either a congenital or acquired prolonged QT interval. Risk factors for torsades de pointes include medications that prolong the QT interval, female gender, hypokalemia, hypocalcemia, hypomagnesemia, ischemia, and structural heart disease.[7][8]
*Myocarditis is an inflammatory process involving cardiac myocytes that is generally secondary to a viral infection. Other sources of myocarditis include bacterial and parasitic infection, ingestion of medication or recreational substance, hypersensitivity reactions to medications or venoms, autoimmune disease, sarcoidosis, hypothermia, ischemia, radiation, and rejection of a transplanted heart.[9]
*Cardiac tamponade is a collection of symptoms (traditionally hypotension, jugular venous distention, muffled heart sounds, pulses paradoxus, and interventricular septum bowing during inspiration) secondary to increased pressure in the pericardial space. This pressure increase results from a transudative, exudative, or sanguineous pericardial effusion. The effusion can be secondary to acute trauma, aortic dissection, intrathoracic neoplasm, recent procedures or instrumentation of the thorax, radiation therapy, autoimmune disease, myocardial infarction, medication, uremia, or infection.[10]
*Acute coronary syndrome is a collection of symptoms secondary to ischemic heart disease. It can present as unstable angina, non-ST segment elevation myocardial infarction (NSTEMI), and ST-segment myocardial infarction (STEMI). Patients at elevated risk for acute coronary syndrome are patients with obesity, hypercholesterolemia, hypertension, diabetes mellitus, age greater than 50 years, male gender, tobacco use, and a family history of heart disease.[11]
Non-cardiac pathologic etiologies:
Respiratory:
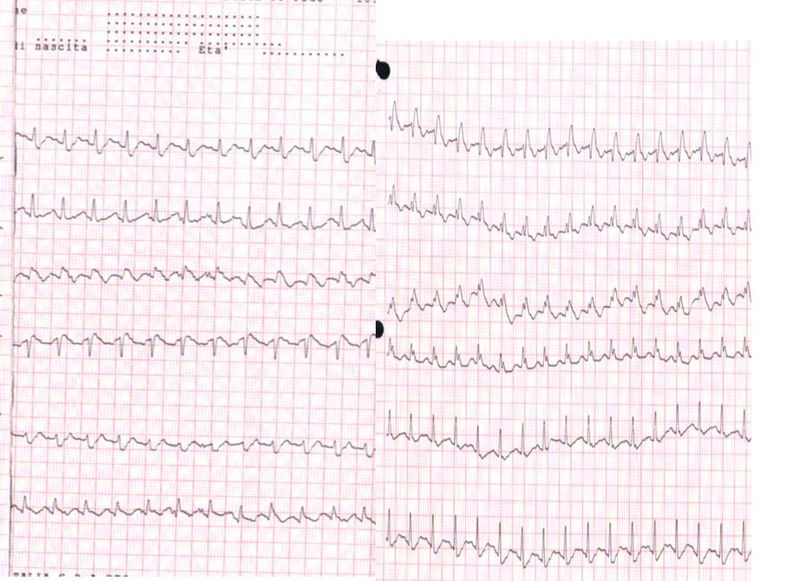
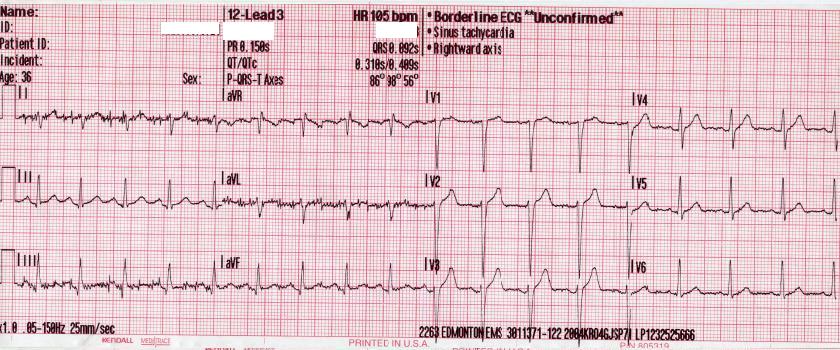
*Pulmonary Emboli are disorders of the pulmonary vasculature. They can be acute, chronic, or both.[12][13] Acute pulmonary emboli are generally more clinically significant and have higher rates of morbidity and mortality. Acute pulmonary emboli most often are a piece of a deep vein thrombus that has traveled through the circulation to the pulmonary vasculature, but fat emboli from an orthopedic injury, amniotic fluid emboli during pregnancy, and air emboli from instrumentation of central vasculature are all potential etiologies.[14][15][16][15][14] See Image. Electrocardiogram, Pulmonary Embolism.
*Hypoxia is a clinical state where tissues do not receive the necessary amount of oxygen to support their metabolic demand. Hypoxia can result from the inability to take in oxygen, transport the oxygen, or perform oxygen gas exchange.[17]
Gastrointestinal/Renal/Electrolyte:
*Hypoglycemia is the state when plasma glucose concentration falls below 70 mg/dL. It most commonly presents as a side effect of the medical therapies, i.e., drug-induced. It can also result from critical illness, alcohol consumption, hormonal imbalance, bariatric surgery, inborn errors of metabolism, insulinomas, and some pituitary and adrenal adenomas.[18]
*Dehydration results from an imbalance of the total body fluid intake and output. To maintain cardiac output in the setting of intravascular depletion, heart rate will increase.[19]
*Hyperkalemia is a potassium serum level greater than the standard accepted upper limit of normal (generally 5.0 to 5.5 mEq/L). Falsely elevated potassium levels, from sample hemolysis, is the most common cause of hyperkalemia. Additional etiologies include renal failure, rhabdomyolysis, excessive exercise, metabolic acidosis, insulin deficiency, tumor lysis syndrome, medication-induced, and increased intake of potassium.[20]
Hypomagnesemia is a serum magnesium level below 1.6 mg/dL. Hypomagnesemia can result from the low intake or poor absorption of magnesium, and increased filtration or excretion of magnesium. These can all be either congenital or acquired conditions. Acquired conditions that impact magnesium level include prolonged nasogastric suction, malabsorption, acute pancreatitis, refeeding syndrome, late-term pregnancy, lactation, uncontrolled diabetes mellitus with glucosuria or diabetes mellitus complicated by diabetic nephropathy, post-kidney injury diuresis, proximal tubule injury or medications that act on the proximal tubule, thick ascending loop of Henle, or descending loop of Henle.[21]
Hypocalcemia is a serum calcium level below 8.5 mg/dL. It can result from lack of sunlight exposure, nutritional deficiency, malabsorption, post-gastric bypass surgery, end-stage liver disease, chronic kidney disease, vitamin-D dependent rickets, hypomagnesemia, hyperphosphatemia, medications, rapid transfusion of large volumes of citrate-containing blood, acute critical illness, osteoblastic metastases, acute pancreatitis, rhabdomyolysis, and mitochondrial gene defects.[22]
Infectious Disease:
*Sepsis is a systemic inflammatory illness secondary to an infection that causes organ dysfunction and is a leading cause of mortality in the United States. It is a spectrum of illness and can present as mild, fulminant, or intermediate disease. In the early stages of sepsis, the large inflammatory burden will decrease systemic vascular resistance. The body compensates for decreased systemic vascular resistance by increasing heart rate, and patients (particularly pediatric patients) can be normotensive to hypertensive through this compensatory period.[23]
Vascular:
*Shock is an acute circulatory failure that provides insufficient tissue perfusion and hypoxia. There are four major types of shock- distributive, hypovolemic, cardiogenic, and obstructive. Distributive shock is characterized by decreased systemic vascular resistance and is secondary to sepsis, systemic inflammatory response syndrome, anaphylaxis, neurologic trauma, or endocrinologic pathology. Hypovolemic shock characteristically demonstrates intravascular volume depletion. It can be secondary to hemorrhage or dehydration. Cardiogenic shock is characterized by decreased cardiac output. Cardiogenic shock can be secondary to infarction-causing either large areas of ischemia in the ventricles, papillary muscle rupture, or ventricular septal rupture; infection of the myocardium; pericardial effusion, aortic dissection, acute arrhythmias; and cardiotoxic medications-particularly in an overdose. Obstructive shock is characterized by inappropriate cardiac output despite normovolemia and cardiac function. Common causes include tension pneumothorax, cardiac tamponade, restrictive cardiomyopathy, constrictive pericarditis, hemodynamically significant pulmonary emboli, coarctation of the aorta, or other cardiac outflow obstruction, restrictive cardiomyopathy, and severe pulmonary hypertension.[24]
Hematologic
*Hemorrhage is the disease process where a clinically significant amount of blood is lost after a blood vessel is damaged. There are four classes of hemorrhage. Class I is less than 15% of total blood volume. In general, there is no change to hemodynamics, and urine output is maintained. Class II is between 15 to 30% of total blood volume loss, and mild tachycardia (10 to 20% increase in baseline rate), hypotension, tachypnea, and decreased urine output are notable. Class III is 30 to 40% of total blood volume loss with associated tachycardia (20 to 40% increase), hypotension, tachypnea, and oliguria. Class IV is greater than 40% blood loss with significant tachycardia (40% pulse increase), hypotension, tachypnea, anuria, and lethargy.[25][26]
Anemia is a disease where the body does not have the appropriate amount of hemoglobin or red blood cells. Anemia can be acute or chronic and can divide into microcytic, normocytic, and macrocytic. Microcytic anemia can be secondary to iron deficiency, lead poisoning, or thalassemia. Normocytic anemia can be secondary to malignant processes, hemorrhage, hemolysis, chronic disease, aplastic anemia, or other bone marrow failure syndromes. Macrocytic anemia can be secondary to vitamin B12 or folate deficiency, hypothyroidism, medications, alcoholism, liver disease, or myelodysplastic syndromes.[25]
Toxicology:
*Ingestion of medications can cause tachycardia. The following are is a list of common medications that will result in tachycardia:
- Albuterol
- Amphetamines
- Anticholinergics
- Antihistamine
- Atropine
- Caffeine
- Carbon monoxide
- Cellular asphyxiants
- Chloral hydrate
- Clozapine
- Cocaine
- Dobutamine
- Dopamine
- Ephedrine
- Epinephrine
- Fluoride
- Levothyroxine
- Methylphenidate
- Phenothiazines
- Potassium
- Pseudoephedrine
- Scopolamine
- Theophylline
- Tricyclic antidepressants
*Withdrawal from substances or medications is an additional source of tachycardia. The following is a list of common medications that will result in tachycardia when discontinued:
- Alcohol
- Benzodiazepines
- Beta-blockers
- Calcium channel blockers
- Carbamates
- Clonidine
- Digitalis lanata
- Digitalis pupurea
- Digitoxin
- Digoxin
- Imidazoline
- Magnesium
- Oleander
- Opioids
- Organophosphates
- Phenylpropanolamine
- Red Squill
- Sedative-hypnotics
Endocrinologic:
Pregnancy results in many physiologic changes, including increased heart rate, cardiac output, and vascular volume.[27]
Hyperthyroidism is a condition secondary to excess thyroid hormone. It commonly presents with multisystem pathology, including palpitations, tachycardia, anxiety, tremor, diaphoresis, edema, hyperreflexia, weight loss, and changes to the skin and nails. Hyperthyroidism can also result in cardiac arrhythmias such as atrial fibrillation.[28]
Pheochromocytomas and paragangliomas are neuroendocrine tumors of the adrenal gland and extra-adrenal autonomic tissue, respectively. They present with tachycardia, diaphoresis, diarrhea, hypertension, weight loss, and anxiety.[29]
*denotes a life-threatening etiology