Introduction
The sciatic nerve is the largest nerve in humans, originating in the lower back and traveling posteriorly through the lower limb as far down as the heel of the foot. The sciatic nerve innervates a significant portion of the skin and muscles of the thigh, leg, and foot.[1][2]
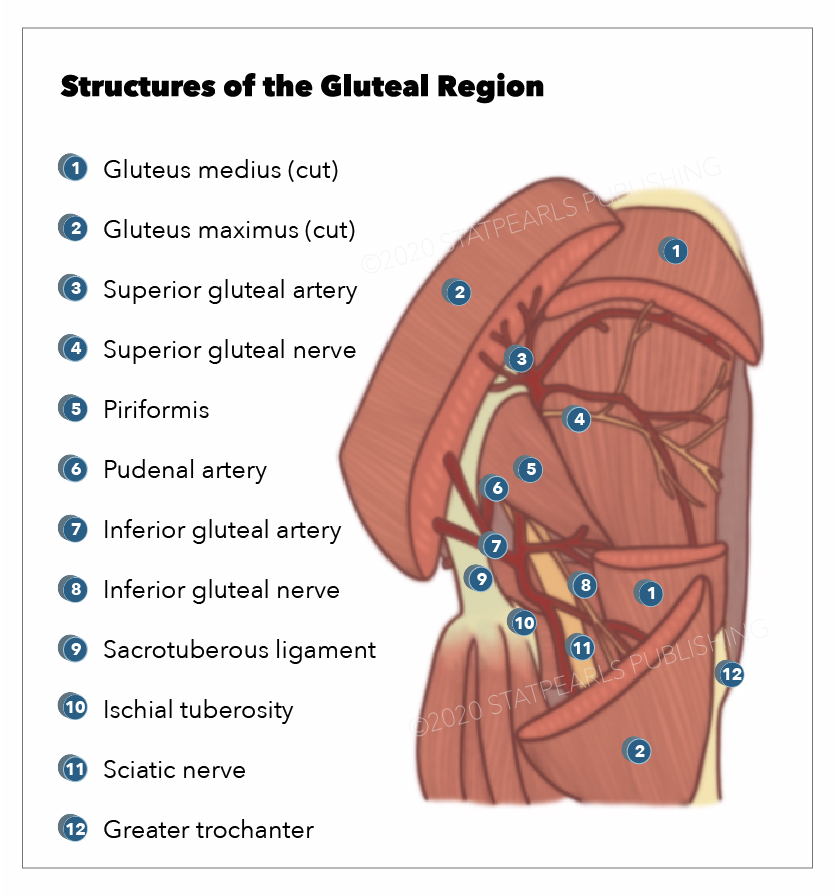
The nerve originates from the ventral rami of spinal nerves L4 through S3 and contains fibers from both the posterior and anterior divisions of the lumbosacral plexus. After leaving the lower vertebrae, the nerve fibers converge to form a single nerve. It exits the pelvis through the greater sciatic foramen inferior to the piriformis muscle along with the pudendal nerve and vessels, inferior gluteal nerve and vessels, nerve to obturator internus, and posterior femoral cutaneous nerve. The sciatic nerve then progresses down the posterior compartment of the thigh deep to the long head of the biceps femoris muscle, superficial to adductor magnus and short head of the biceps femoris muscle, and laterally to semitendinosus and semimembranosus muscles.
Just before reaching the popliteal fossa, it divides into two important branches. One branch is the tibial nerve, which continues to descend in the posterior compartment of the leg and foot. The other branch is the common peroneal nerve, which travels down the lateral and anterior compartments of the leg and foot. Until this division occurs, the medial component is referred to as the tibial division or the common fibular (peroneal) division of the sciatic nerve.
Structure and Function
The sciatic nerve provides motor innervation to the posterior compartment of the thigh. This includes the biceps femoris, semimembranosus, semitendinosus, and the ischial portion of the adductor magnus, providing knee flexion and hip adduction.
The tibial nerve innervates the posterior compartment of the leg and foot, which includes the gastrocnemius, soleus, plantaris, popliteus, flexor hallucis longus, flexor digitorum longus, and tibialis posterior. These muscles are primarily responsible for plantar flexion and flexion of the toes.
The common fibular (peroneal) nerve innervates the anterior and lateral compartments of the leg and foot. The anterior compartment includes tibialis anterior, extensor hallucis longus, extensor digitorum longus, and fibularis tertius. These muscles are primarily responsible for dorsiflexion of the foot and extension of the toes. The lateral compartment includes the peroneus longus and brevis, which are responsible for foot eversion.[3]
The sciatic nerve also provides sensory innervation to the skin of the foot and the lower leg (except for the medial leg, which is innervated by the saphenous nerve). The tibial nerve further divides into the medial and lateral plantar nerves, which are responsible for the sensation of the sole. The common fibular (peroneal) nerve further divides into the superficial fibular (peroneal) nerve and deep fibular (peroneal) nerve. The superficial fibular nerve provides sensory innervation to the lateral leg and dorsum of the foot. The deep fibular nerve is responsible for sensation between the first and second toes. The medial and lateral sural nerves are made up of collateral branches from both the tibial and common fibular nerves and provide sensation to the calf and a small lateral portion of the foot.
Embryology
A process called neurulation begins at the beginning of the third week after fertilization. It starts when a region of cells overlying the ectoderm thickens and forms the neural plate. The neural plate leads to the neural tube and neural crest cells. The neural crest cells will lead to the neurons in the peripheral nervous system, including the sciatic nerve. Additionally, Schwann cells, responsible for myelination of the peripheral nervous system, are also derived from neural crest cells.
Blood Supply and Lymphatics
Peripheral nerves, including the sciatic nerve and its divisions, receive their blood supply from 2 sources, the extrinsic and intrinsic systems. The extrinsic system consists of contributions from nearby arteries and veins that comprise the vasa nervorum.
The intrinsic vasculature of the sciatic nerve includes arteries and veins that run longitudinally just deep to the epineurium. This vasculature connects with extrinsic vasculature at various junction points. The flow within the nerve's vasculature is highly variable and consists of many collateral networks. When comparing the branches of the sciatic nerve, the tibial portion of the sciatic nerve has a richer blood supply than the fibular branches.
Muscles
The sciatic nerve emerges from the greater sciatic foramen below the piriformis. It divides into the (medial) tibial and (lateral) common fibular divisions. The septum of Compton-Cruveilhier separates the two divisions. The tibial division innervates the posterior half of the adductor magnus, the semitendinosus, the semimembranosus, and the long head of the biceps femoris. These hamstring muscles arise from the ischial tuberosity. They are long, stringy muscles arising from the ham (buttock).
In the thigh, the short head of the biceps femoris is supplied by the common fibular nerve.
The tibial nerve then passes into the leg, innervating the superficial posterior compartment and the deep posterior compartment. The superficial posterior compartment consists of the triceps surae (medial and lateral heads of the gastrocnemius and the soleus) and the plantaris and popliteus. The plantaris is innervated by the tibial nerve, as is the popliteus. The deep posterior compartment consists of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus. Passing behind the medial malleolus, the tibial nerve forms the medial plantar nerve, which innervates the flexor hallucis brevis and abductor hallucis, the first lumbrical, and the fibularis tertius.
The common fibular nerve divides into the superficial fibular nerve that innervates the fibularis longus and the fibularis brevis in the lateral compartment of the leg and the deep fibular nerve, which innervates the tibialis anterior, the extensor digitorum longus, the extensor hallucis longus, extensor hallucis brevis, extensor digitorum brevis, and the first lumbrical. An important clinical point is that the deep fibular nerve innervates the space between the big and second toe. This is the only part of the foot with sensory innervation from the deep fibular nerve.
The lateral plantar nerve is the homolog of the ulnar nerve in the hand. It innervates the adductor hallucis, flexor digiti minimi brevis, lumbricals 2 through 4, four dorsal interossei, and three palmar interossei.
Physiologic Variants
Most often, the undivided sciatic nerve exits the greater sciatic foramen inferior to the piriformis, but this is not always the case.[4] In the most common anatomic variant, the sciatic nerve splits above the piriformis, and one division exits through the piriformis while the other exits below. There are six anatomic variants described in the current literature.[5][6][7][8]
- Type I: sciatic nerve exits inferior to piriformis, undivided. This is the most common form.[9][10]
- Type II: sciatic nerve divides above piriformis; one portion exits through the piriformis, the other inferior to it. The common fibular (peroneal) division passes through the piriformis. This is especially problematic when the common fibular nerve passes between the two tendons of the piriformis.[11] In 10%, the sciatic nerve passed through or above the piriformis.[9]
- Type III: sciatic nerve divides above piriformis; one portion courses anterior to piriformis, the other posterior to it
- Type IV: sciatic nerve exits through the piriformis, undivided
- Type V: sciatic nerve divides above piriformis; one portion exits through the piriformis, the other superior to it
- Type VI: sciatic nerve divides exist from the superior aspect of the piriformis posteriorly, undivided
Surgical Considerations
Sciatica is defined as irritation or compression of the sciatic nerve that causes pain in the buttock area with radiation to the lower leg. The vast majority of cases have a spinal cause, such as disc herniation or rupture causing L5 or S1 nerve root impingement. Other common causes include spinal stenosis, degenerative disc disease, and spondylolisthesis. There are also many non-spinal causes of sciatica, which are less common. These include piriformis syndrome, trauma, postoperative complications, gynecologic conditions, and herpes zoster.[12][13][14]
Symptoms include mid-buttock pain that radiates down the leg, most often unilaterally. Depending on where the sciatic nerve is irritated, the patient will often experience paresthesias in a dermatomal distribution, either L5 or S1. Weakness and changes in reflexes are less commonly seen. L5 has no reflex. S1 is the ankle jerk reflex.
One test that should always be done in patients with low back pain is the Lasegue straight leg raising with the patient supine. The test is positive if there is ipsilateral pain between 10 to 60 degrees. This test is quite sensitive (90%) but not specific. If this test elicits pain in the contralateral leg, one should suspect disc herniation and order an imaging test. MRI is very useful when the exact level of compression in the spine is unclear.
MRI can also assess the soft tissues (including discopathy), the presence of an infection, or a neoplastic cause. If there is urine retention or dysesthesia around the anus in a patient with sciatica, one should suspect cauda equina syndrome. Prompt surgical decompression is indicated for this disorder.
The majority of cases of sciatica are treated conservatively with rest for a few days, pain medication, and some physical therapy. Surgery may be required in cases where there is significant stenosis or there is evidence of irritation of the nerve.[15]
Clinical Significance
Piriformis Syndrome
Piriformis syndrome is caused by a swollen piriformis that compresses the sciatic nerve or its divisions - the tibial division and/or the common fibular division. In Beatty and Anson type and Robinson type C or III, the common fibular division passes above the piriformis muscle.[5] This has been confirmed surgically and using an intraoperative EMG study in which stimulation of the sciatic nerve caused dorsiflexion of the foot. Division of the piriformis muscle by a transgluteal surgical approach produced a cure.[5]
The piriformis syndrome produces hip pain that radiates down into the lower limb. The pain is made much worse when driving and sitting. Unlike a herniated disc, piriformis syndrome does not produce paralumbar muscle spasms. The presence of piriformis syndrome has been estimated to be about 16%.[16] It has been postulated that piriformis syndrome is the most common form of extraspinal sciatica.[17]
Guiding the lidocaine injection with ultrasound can be used in an emergency department setting to treat piriformis syndrome.[18]
In an MRI study of 254 sciatic nerves in 127 patients, the sciatic nerve and piriformis muscle in patients with piriformis syndrome demonstrated increased T2 signal intensity. Splitting of the sciatic nerve was seen in 56/64 compared to 20/190 control cases (P<0.0001). The symptomatic side demonstrated the increased size of the sciatic nerve, increased piriformis size, and increased T2 signal intensity.[6]
The posterior aspect of the piriformis syndrome is especially important when performing an arthroplasty of the hip, blockade of the sciatic nerve, or image-guided injection of the piriformis syndrome.[9]
One concept is that trauma of the piriformis causes the release of inflammatory mediators that cause swelling of the piriformis, compressing the divisions of the sciatic nerve.
Other Issues
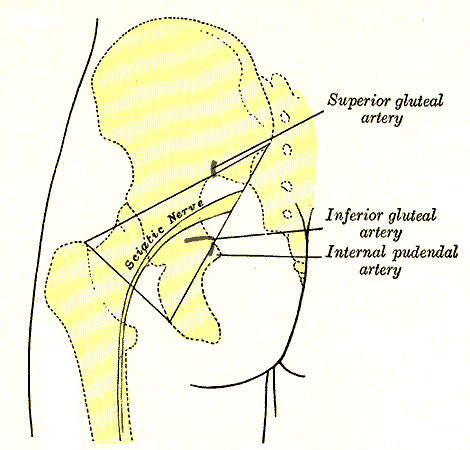
The buttock is often used for intramuscular injections. The usual concept is that the superolateral portion of the buttock is the safe side, whereas injection of the inferomedial portion of the buttock places the sciatic nerve at risk. A complication of this concept is many people have a fatty elevation on the inferomedial buttock. Using the “upper and outer” quadrant as a guide with this misconception places the sciatic risk in danger. Injection of the sciatic nerve can cause sciatic neuropathy. MRI of the sciatic nerve has been described in pediatric patients.[19] It is routinely used in adults.
Experiments in rats have shown that lesions of the L4 and L5 segments that form the sciatic nerve produce inflammatory reactions in the alpha-motor neurons in the ventral horns. The NLRP3 inflammasome is greatly upregulated in the motor neurons during the first three days after injury. This inflammatory reaction greatly inhibits the regeneration of the sciatic nerve. Extracellular ATP is an important modulator in the pro-inflammatory process that increases microgliosis, inhibiting the regeneration of these motor neurons.[20]