Continuing Education Activity
Pneumocephalus, also known as pneumatocele or intracranial aerocele, is the presence of air in the intracranial space. Pneumocephalus can occur following trauma, cranial surgeries, or spontaneously. The condition can be classified into simple and tension types based on severity and progression. In terms of onset, a pneumocephalus that started less than 72 hours before presentation is acute, while a delayed pneumocephalus is one that began more than 72 hours before presentation.
Symptoms of pneumocephalus can vary based on the amount of air present and its location within the cranial cavity. Mild cases may not present with significant symptoms, while larger intracranial air accumulations can cause headaches, dizziness, nausea, and neurological deficits. The condition is a medical emergency, although management can be challenging as pneumocephalus can resemble other neurologic conditions.
This activity is designed to enhance learners' proficiency in evaluating and managing pneumocephalus. Valuable skills will be gained that will equip learners to collaborate seamlessly with an interprofessional team caring for patients with this condition.
Objectives:
Identify the signs and symptoms of pneumocephalus.
Determine the diagnostic studies appropriate for evaluating patients with pneumocephalus and identify the imaging features indicative of this condition.
Identify the treatment options for pneumocephalus and formulate a personalized management plan for a patient with this condition.
Collaborate effectively with an interprofessional team to manage patients with pneumocephalus, specifically in formulating short- and long-term interventional strategies to improve outcomes.
Introduction
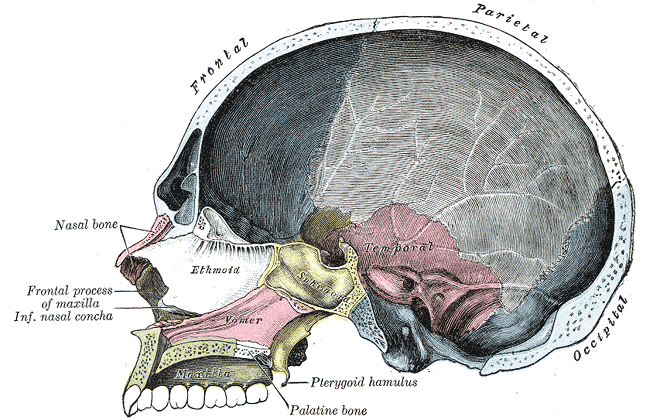
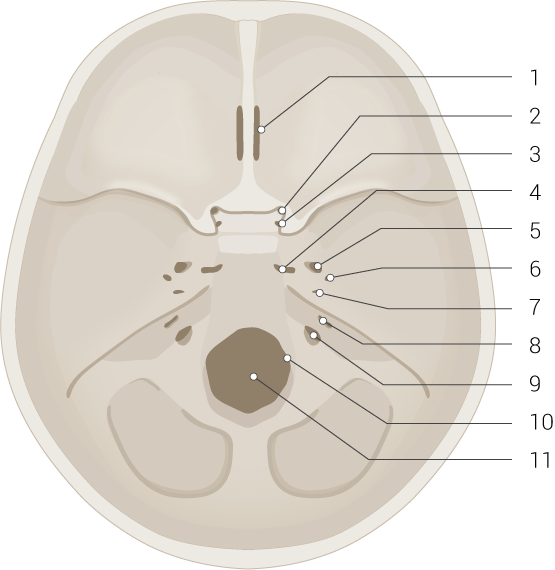
The skull or cranium is the skeleton of the head, consisting of 2 parts: the neurocranium and the facial skeleton (see Image. Skull Interior). The neurocranium or cranial vault protects the meninges and brain. The calvaria or skullcap serves as the brain's roof, while the cranial base acts as the floor. The cranial base is divided into the anterior, middle, and posterior cranial fossae (see Image. Skull Base and Foramina).
The neurocranial bones include the following:
- Frontal bone
- Paired parietal bones
- Paired temporal bones
- Occipital bone
- Sphenoid bone
- Ethmoid bone
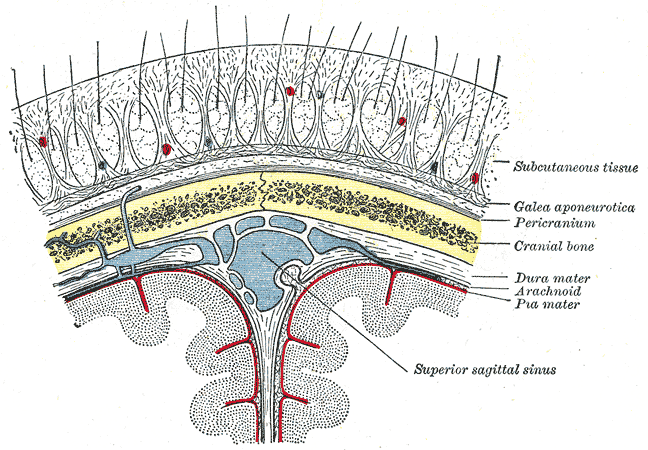
The scalp overlies the calvaria from the occipital bone's superior nuchal lines to the frontal bone's supraorbital margins anteriorly and the zygomatic arches' temporal fascia laterally (see Image. Relationship of the Meniges to the Skull and Brain). The 5 layers of the scalp are best remembered by the acronym "SCALP": skin, connective tissue (dense), aponeurosis, loose connective tissue, and pericranium.
The meninges lie deep to the skull's endosteal layer. The 3 meningeal layers, from superficial to deep, are the dura (dura mater), arachnoid (arachnoid mater), and pia (pia mater). The meningeal spaces from superficial to deep are the following:
- Epidural: a potential space that can form in the skull-dura interface; also known as the extradural space
- Subdural: a potential space that can develop between the dura and subarachnoid
- Subarachnoid: an actual space between the arachnoid and pia that contains blood vessels, cerebrospinal fluid (CSF), and trabecular cells
The facial skeleton, also known as splanchnocranium or viscerocranium, comprises the skull's anterior segment. The bones of the facial skeleton are the following:
- Paired lacrimal bones
- Paired nasal bones
- Paired maxillae
- Paired zygomatic bones
- Paired palatine bones
- Paired inferior nasal conchae
- Mandible
- Vomer
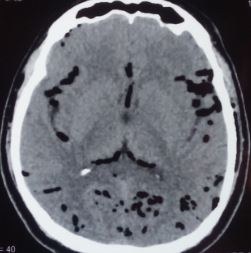
Pneumocephalus, also known as pneumatocele or intracranial aerocele, is the presence of air in the epidural, subdural, or subarachnoid space or within the brain parenchyma or ventricular cavities.[1] Lecat first described this condition in 1741 but Luckett coined the term "pneumocephalus" independently in 1913. Wolff used the same term to describe the condition in 1914.[2][3][4] The term "tension pneumocephalus" was proposed in 1962 by Ectors, Kessler, and Stern (see Image. Tension Pneumocephalus).[5]
Pneumocephalus can occur spontaneously or as a complication of trauma and cranial surgery. This condition is classified as simple or tension pneumocephalus, depending on severity and progression. Pneumocephalus can also be acute or delayed based on the onset. Acute pneumocephalus develops less than 72 hours before presentation, while the delayed type develops more than 72 hours after presentation.[6]
Pneumocephalus has to be differentiated from the following terms:
- Pneumorrhachis, which denotes intraspinal air
- Pneumocele, which is a focal or diffuse paranasal sinus (usually frontal) enlargement with bone thinning and hyperpneumatization
- Pneumosinus dilatans, which is the same as a pneumocele but has the sinus walls intact and normal
- Pneumoventricle, which is the presence of intraventricular air
The term "tension pneumoventricle" is used when air accumulates in the ventricles, increasing the intracranial pressure (ICP) and potentially compressing the brain's vital centers (see Image. Pneumocephalus and Pneumoventriculi).[7]
Etiology
Pneumocephalus can arise from various causes, summarized below. The most common cause of this condition is head or facial trauma. Air can enter the cranial cavity through skull fractures.
Table. Possible Causes of Pneumocephalus
|
Traumatic
- Fractures involving the skull base with breach of the dura
- Fractures of air sinuses
- Penetrating head injuries with a dural laceration
- High-pressure trauma to the conjunctiva
- Subarachnoid-pleural fistula [8]
|
|
Infectious
- Meningitis or ventriculitis that is produced by gas-forming organisms
- Chronic otitis media and sinusitis
|
|
Neoplastic
- Dermoid cyst rupture
- Tumors that erode the skull or skull base, like osteoma, epidermoid, or pituitary adenoma
|
|
Iatrogenic
- Transcranial surgeries, especially posterior fossa surgeries in a prone position and following chronic subdural hematoma evacuation in a supine position
- Transsphenoidal surgeries
- Following lumbar puncture or spine surgeries
- Ventriculostomies
- Epidural or subarachnoid blocks
- Endoscopic dacryocystorhinostomy or septoplasty
- Secondary to CSF leakage from the surgical site
- Positive pressure ventilation
- Spreading of subcutaneous emphysema through the ventriculoperitoneal shunt track into the brain [9][10][11]
|
|
Spontaneous
- Following the development of spontaneous cerebrospinal fluid rhinorrhea
- Secondary to CSF leakage from myelomeningocele
- Spontaneous otogenic pneumocephalus occurs when there is an anomalous communication between the intracranial space and a hyperpneumatized temporal bone
|
|
Congenital
- Skull base defects
- Tegmen tympani defect
|
|
Miscellaneous
|
Pneumocephalus can vary in severity, and the symptoms can range from mild headaches to more severe neurological deficits. Treatment depends on the underlying cause and the patient's clinical condition.
Epidemiology
The incidence of pneumocephalus depends on the etiology. The condition is seen in almost all postcraniotomy cases. The incidence of pneumocephalus following head injury varies depending on the study, from 1% to as high as 82%. About 74% of pneumocephalus cases are due to head trauma.[13][14][36]
Pathophysiology
Several theories regarding the etiology of pneumocephalus exist. These theories include the following:
- Air moves unidirectionally from the outside environment into the cranial cavity. This mechanism is responsible for pneumocephalus following positive pressure ventilation. This theory is called the "ball-valve theory of Dandy."
- ICP decreases due to excessive CSF loss, which may occur artificially via lumbar drainage or physiologically during Valsalva maneuvers. A vacuum is created, trapping air inside the cranium. This theory is called the "inverted-soda-bottle effect of Horowitz and Lunsford."
- Blowing the nose, coughing, or sneezing causes a sudden pressure increase in the air sinuses. Air is then drawn into the brain through defects in the skull base.
- The loss-of-resistance technique, used to identify the epidural space, is thought to be responsible for the development of pneumocephalus after epidural injections.
- Air entry through the meninges can be due to accidental injection, inadvertent dural puncture, or pressure gradients between the cranial cavity and atmosphere.
- Nitrous oxide may cause pneumocephalus during anesthetic procedures. The blood–gas partition coefficient of nitrous oxide is 34 times greater than that of nitrogen. Therefore, nitrous oxide can diffuse into the cranial cavity faster than nitrogen or air.
- Boyle's law states that pressure and volume are inversely proportional at constant temperature. Pneumocephalus expands during flights because air volume increases when pressure decreases inside the cranial cavity.[15][16]
Cranial breaks leave the cranial cavity vulnerable to air entry. Large air pockets can compress intracranial structures and increase the ICP, manifesting as focal neurological deficits. Air is also a potential intracranial infection source. Air entering the meninges can likewise irritate the cerebral cortex and produce seizures.
History and Physical
Pneumocephalus is a medical emergency, though it presents variably. A quick primary survey—assessing the airway, breathing circulation, disability, and exposure (ABCDE)—must be performed immediately upon receiving the patient. Unconscious individuals without respirations and pulses must be administered resuscitative measures promptly, regardless of cause. Once the patient's emergent needs are addressed, the secondary survey and diagnostic workup may be initiated.
The patient's history is likely to reveal a recent traumatic incident leading to a skull fracture. Symptoms depend on the pneumocephalus volume and intracranial area affected. Most patients are asymptomatic. However, symptomatic conscious patients may have nausea, vomiting, memory loss, speech and sensory changes, rhinorrhea or otorrhea, seizures, headaches, and motor weakness.
Though rare, patients may describe a splashing sound on head movement, known as "bruit hydroaerique," which is pathognomonic of pneumocephalus. This sign may be confirmed by cranial auscultation.
In severe cases, patients may present with altered sensorium, abnormal breathing patterns, or cardiorespiratory arrest. In individuals without a history of trauma, a recent neurosurgical or spinal procedure, infection symptoms, signs of intracranial mass effects, or a history of ventilator use or congenital anomalies may be elicited.
The head-and-neck examination may reveal scalp or skin lacerations, evidence of a skull fracture, blood and fluid in the nose or external auditory meatus, and tympanic membrane perforation. Evidence of multiple traumatic injuries includes respiratory distress signs, hypotension, tachycardia, abdominal rigidity, blood in the genitalia, bloody urine, and axioappendicular fractures. In patients with barotrauma, unilaterally decreased breath sounds (pneumothorax) or a positive Hamman sign (pneumomediastinum) may be noted on auscultation. Neurologic and musculoskeletal findings vary depending on the site affected.
The following features of the patient's history or examination should make clinicians suspicious that the patient may have pneumocephalus:
- CSF leak from the nose, ear, or surgical site
- Persistent headache after cranial or spinal surgery
- Seizures following surgery
- Postoperative meningitis
- Frontal lobe syndrome
- Flapping scalp sign
- Oculomotor nerve palsy
- Papilledema
- Tinnitus [17]
Posterior fossa involvement may occur in tension pneumocephalus, causing brainstem signs, respiratory irregularities, and cardiac arrest. Even paraplegia and hemiplegia have been reported following tension pneumocephalus.
Evaluation
Monitoring and Laboratory Testing
Individuals who appear unstable require continuous vital signs and cardiac monitoring. A fingerstick glucose test must be performed for all unconscious patients to rule out or address hypoglycemia. Individuals requiring oxygen supplementation must be monitored by pulse oximetry.
Laboratory testing must be performed immediately for trauma patients, especially if emergency surgery is considered. The initial tests may include a complete blood count, coagulation profile, blood typing, complete metabolic panel, and urinalysis. Arterial blood gases and electrocardiography may be considered if the patient exhibits cardiorespiratory distress. Imaging studies must be immediately scheduled.
Plain Films
Skull x-rays have been used in the past to identify pneumocephalus, but plain films usually miss small quantities of air. Still, x-rays are useful in evaluating patients with multiple injuries.
Head Computed Tomography Scan Without Contrast
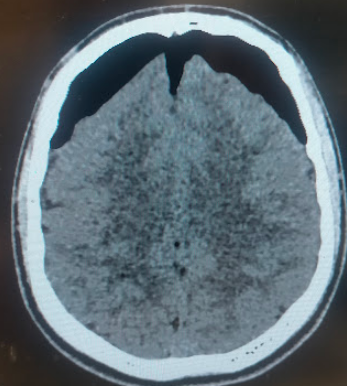
Head computed tomography (CT) scanning without contrast is the gold standard imaging modality in diagnosing pneumocephalus. This study can detect even 0.55 ml of intracranial air, while a skull radiograph requires at least 2 ml to be appreciable.[18] Air has a Hounsfield coefficient of -1000.
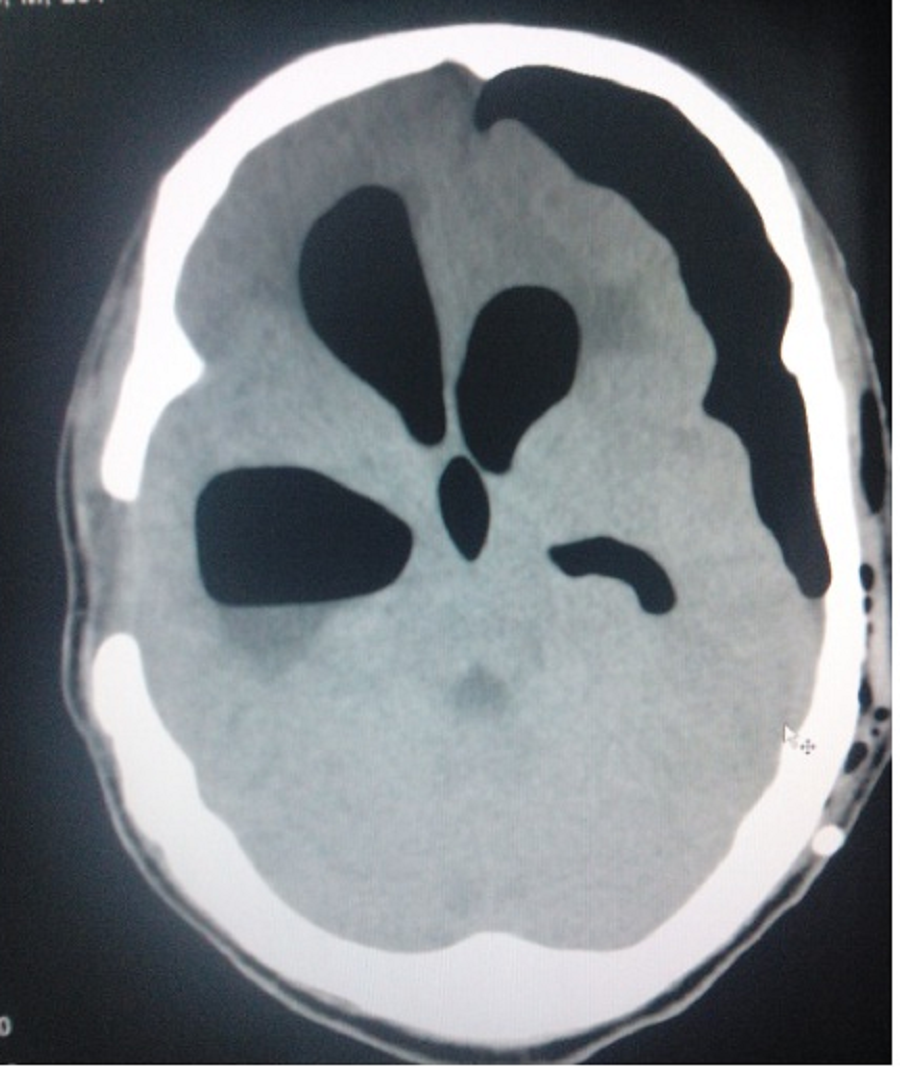
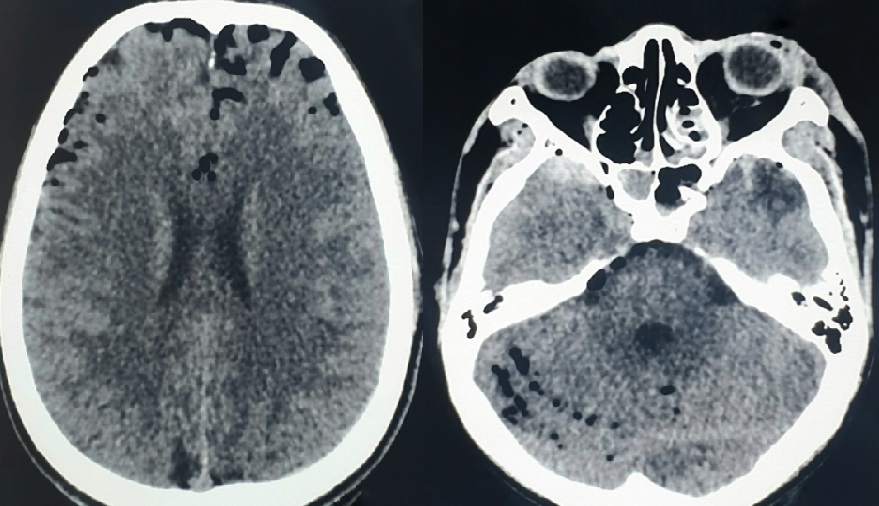
Ishiwata et al identified 2 signs as characteristic of tension pneumocephalus. The first is the Mount Fuji sign, named after Mount Fuji, the highest volcano in Japan. This sign is diagnostic of tension pneumocephalus and is formed by the accumulation of air in the frontal region, separating the frontal lobes' tips in a patient in the supine position (see Image. Mount Fuji Sign in Tension Pneumocephalus). The second is the "air bubble sign," denoting the presence of multiple air bubbles scattered in several cisterns (see Image. Air Bubble Sign in Tension Pneumocephalus).[19]
On the other hand, the "peaking sign" denotes bilateral compression of frontal lobes without separation of the tips. This sign indicates a less severe condition compared to the Mount Fuji sign.
Calculation of the Volume of Postoperative Pneumocephalus
The volume of intracranial air may be determined in 2 ways. The first is by computer-assisted volumetric measurement, which requires special software. The second is by using the ABC/2 formula at the bedside, which has the following steps:
- Select a representative slide near the center of the pneumocephalus.
- Measure "A" or the longest longitudinal length of the pneumocephalus in millimeters in the axial plane.
- Measure "B" or the maximum width in millimeters of the pneumocephalus from the skull's inner table perpendicular to "A" on the same slice.
- Measure "C" or the height of the air in the coronal plane, which is the same as the number of CT scan axial slides showing the pneumocephalus multiplied by the slice thickness.
- Calculate the estimated volume in milliliters using the formula = A x B x C / 2.[20]
The ABC/2 formula correlates well with computer-derived values.[37]
Brain Magnetic Resonance Imaging
Brain magnetic resonance imaging (MRI) may also be useful but is less sensitive than CT in diagnosing pneumocephalus. Air may be mistaken for flow voids or blood products on MRI, appearing dark in almost all sequences.
Treatment / Management
The Advanced Trauma Life Support (ATLS) protocol is a widely recognized, systematic approach to the care of trauma patients that focuses on critical interventions during initial patient assessment and resuscitation. The initial management of any head injury should follow this protocol. Once stabilized and diagnostics have been obtained, the pneumocephalus must be classified to determine the appropriate treatment plan.
Most patients will present with simple pneumocephalus, lacking signs of increased ICP and are asymptomatic. The head CT scan will show intracranial air without tension pneumocephalus indicators like the Mount Fuji sign. Intracranial air disappears over time due to absorption in the tissues. Management is conservative and involves the following measures:
- Bed rest
- Placing the patient in a 30° Fowler position
- Avoiding Valsalva maneuvers like nose-blowing, coughing, and sneezing
- Analgesics and antipyretics
- Osmotic diuretics, if indicated
- High-flow oxygen therapy given at 5 liters per minute for at least 5 days via a face tent or 100% nonrebreather mask with absolute avoidance of positive pressure
- Hyperbaric oxygen therapy.[21]
Atmospheric air is composed of 78% nitrogen and 21% oxygen. The rate of nitrogen absorption from intracranial air depends on nitrogen's partial pressure in the blood, which is inversely proportional to the fraction of inspired oxygen.
Oxygen supplementation reduces blood and brain nitrogen concentration, increasing the nitrogen gradient between the pneumocephalus air collection and surrounding brain tissue. Over time, oxygen replaces intracranial nitrogen—which is well-absorbed in brain tissue and blood—and facilitates nitrogen absorption and eventual pneumocephalus resolution.[22] Serial CT scans may be obtained to monitor the condition.
Although pneumocephalus poses an increased intracranial infection risk, prophylactic antibiotics have not been proven to have a protective advantage in patients with traumatic pneumocephalus.[38]
Surgery is indicated in the following conditions:
- Symptomatic pneumocephalus
- Tension pneumocephalus
- Recurrent pneumocephalus
- Persistent traumatic pneumocephalus lasting more than 1 week
- Tension pneumoventricle
Tension pneumocephalus following cranial surgery can be treated by introducing a needle through the burr hole of the previous craniotomy and aspirating the air with a syringe.
Surgical decompression options include the following:
- Needle aspiration, either blind or under radiological guidance through an existing burr hole or craniotomy [23]
- Controlled decompression via a subdural drain connected to an underwater seal followed by dural defect closure [24]
- Ventriculostomy for pneumoventricle
- Emergency decompression by the creation of fresh cranial burr holes
- Decompressive craniectomy [25]
- Saline-primed Camino bolt insertion
- Subdural evacuating port system (SEPS)™ insertion [26]
Endoscopic endonasal eustachian tube obliteration has also been tried successfully as a treatment for tension pneumocephalus following lateral skull base surgery.[27]
Differential Diagnosis
The differential diagnosis of pneumocephalus is broad but includes mostly neurologic conditions such as the following:
- Brain concussion
- Primary headache syndromes
- Stroke
- Metabolic encephalopathy
- Intracranial hematoma
- Diffuse axonal injury
- Arteriovenous malformations
- Intracranial neoplasm
- Intracranial infection
On imaging, pneumocephalus may be mistaken for other conditions. For example, intracranial fat can appear hypodense on CT scans and be mistaken for pneumocephalus, though it has a much higher density (-90 HU) than air (-1000 HU). On MRI, pneumocephalus may be mistaken for blood products or flow voids.
Prognosis
Simple pneumocephalus usually resolves spontaneously with conservative therapy. However, it can occasionally produce seizures and meningitis. Prognosis is generally good even with tension pneumocephalus, provided timely treatment is given.
The presence of pneumocephalus might act as a predictor of chemical meningitis following corpus callosotomy.[28] The postsurgical appearance of pneumocephalus is also a predictor of chronic subdural hematoma recurrence after evacuation. Thus, pneumocephalus is a component of the Puerto Rico Recurrence Scale.[29]
Complications
The potential complications of pneumocephalus include meningitis, seizures, brain abscess, brain herniation secondary to tension pneumothorax, and death. Early intervention can prevent these complications and improve patient outcomes.
Deterrence and Patient Education
The following methods can help prevent the development of pneumocephalus during or after surgical procedures:
- Filling of the surgical site with saline at the time of dural closure
- Administering the Valsalva maneuver during closure, before the last dural suture, to allow air to escape outside
- Using a smaller-gauge spinal needle for lumbar puncture to make a smaller dural perforation and minimize CSF leakage
- Keeping the patient in the supine position with no head-end of bed elevation following chronic subdural hematoma evacuation
- Positioning the head during dural closure so that the last part of the dural defect becomes the highest point. This facilitates the escape of residual air while filling the subdural space with saline.
- Using saline rather than air to identify the epidural space during epidural injections
- Avoiding high airway pressure and hyperventilation during invasive ventilation
The inhalational anesthetic nitrous oxide was previously thought to cause pneumocephalus if not withdrawn before dural closure. However, a randomized control trial demonstrated that nitrous oxide did not cause a significant ICP increase or produce large pneumocephalus volumes even if administered postoperatively.[30]
Evidence does not support the prophylactic administration of ceftriaxone for preventing meningitis in patients with traumatic pneumocephalus.[31]
Neurosurgical procedures may result in residual intracranial air and also cause continuous air entry into the cranial cavity. Hence, patients must be advised to wait at least 7 days before taking a flight as cabin pressure changes can introduce air intracranially.[32] Air travel is not advisable for patients with an intracranial air volume of more than 30 ml. Intracranial air volume of 20 ml and initial ICP of 15 mmHg were identified as conservative thresholds for safe air travel among such patients.[33]
Patients may be advised the following to avoid complications from pneumocephalus during a flight:
- Taking a low-level flight or maintaining ground-level cabin pressure during the flight
- Avoiding frequent cabin pressure changes
- Seeking a position that reduces CSF leaks
- Administering supplementary oxygen
- Taking preflight decongestants
- Avoiding Valsalva maneuvers
- Preventing hypoventilation and carbon dioxide accumulation if the patient is ventilated
- Obtaining imaging studies immediately before the flight to assess the volume of pneumocephalus and rule out an extracranial-intracranial fistulous process
- Educating patients regarding patient activity-related pathophysiology and the time course of pneumocephalus
- Reducing the stresses induced by acceleration (including changing g-forces), noise, or hypoxemia.[34]
Avoiding air travel for 2 to 8 weeks after intracranial surgery is recommended.[35]
Pearls and Other Issues
The most important points to remember about evaluating and managing pneumocephalus are the following:
- Pneumocephalus has various causes, but most are trauma-related.
- The condition presents variably. Most patients have the simple type and are asymptomatic, but complications can develop if tension pneumocephalus is not treated immediately.
- The management of all patients with suspected head trauma should follow ATLS protocol.
- CT scan is the imaging modality of choice for pneumocephalus.
- Simple pneumocephalus may be managed conservatively. Antibiotics have little effect on intracranial infection risk in patients with pneumocephalus.
- Surgery is reserved for patients with symptomatic pneumocephalus, tension pneumocephalus, recurrent pneumocephalus, persistent traumatic pneumocephalus lasting more than 1 week, and tension pneumoventricle.
- The prognosis is generally good for patients with simple pneumocephalus. Prompt intervention improves the prognosis of tension pneumocephalus significantly.
Notably, the definite treatment depends on the specific etiology of pneumocephalus and the patient's clinical condition.
Enhancing Healthcare Team Outcomes
The management of pneumocephalus must involve an interprofessional healthcare team to produce the best outcomes. The team members should include the following providers:
- Emergency medicine physician: often the first healthcare professional to encounter patients with head trauma or acute neurological symptoms. This provider performs the initial assessment, stabilizes the patient, and coordinates with specialists for further management.
- Radiologist: interprets imaging studies to confirm the diagnosis, assess the extent of pneumocephalus, and identify any associated injuries or conditions. The radiologist's expertise is crucial in guiding the treatment plan.
- Neurosurgeon: assesses the extent of pneumocephalus and may perform necessary surgical procedures.
- Intensivist: may be involved in managing patients in the intensive care unit with pneumocephalus.
- Anesthesiologist: may be involved in cases requiring surgical intervention.
- Infectious disease specialist: may be consulted to guide the appropriate antimicrobial therapy and overall management if an intracranial infection develops as a complication of pneumocephalus.
- Respiratory therapist: assists in managing ventilator settings, ensuring adequate oxygenation, and monitoring the patient's respiratory status when mechanical ventilation is required.
- Occupational and physical therapists: providers who may be involved in the later stages of care to assess and facilitate the patient's recovery, especially if neurological deficits or functional impairments exist.
- Primary care physician or pediatrician: monitors patients and coordinates care in the outpatient setting.
Effective communication and collaboration among these healthcare professionals are essential to ensure a coordinated and well-rounded approach to the short- and long-term management of pneumocephalus.