Introduction
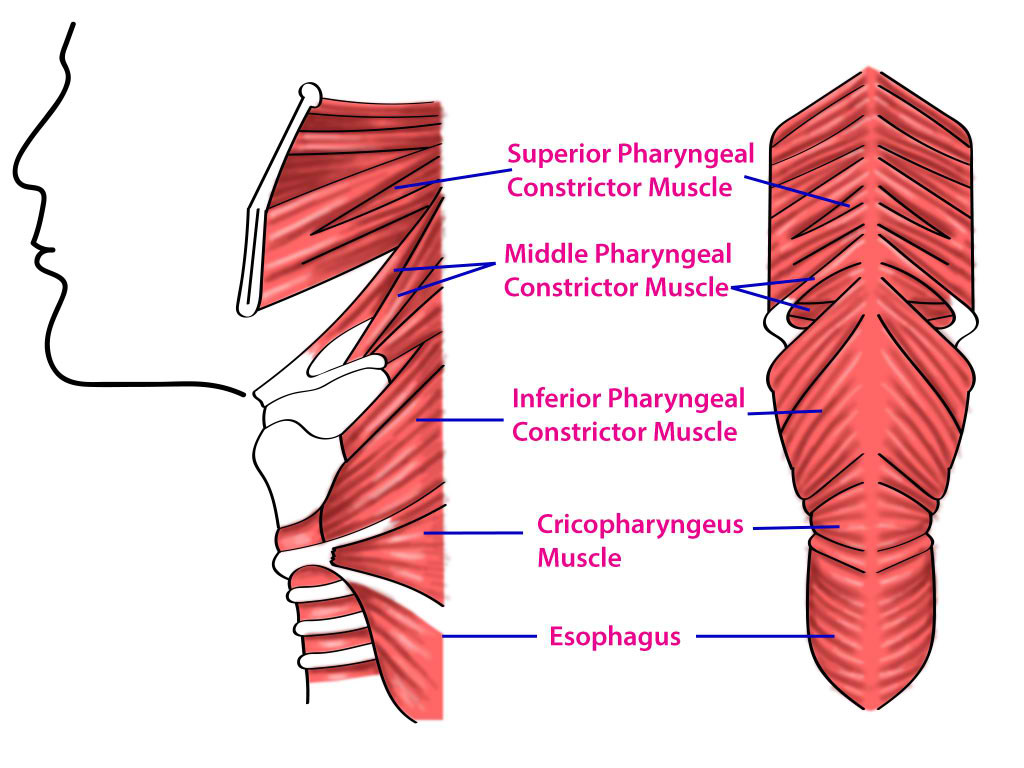
The pharynx is part of the digestive system posterior to the oronasal cavity and larynx. This muscular tube is divided into the oropharynx, nasopharynx, and laryngopharynx. Pharyngeal muscles are organized into an outer circular layer and an inner longitudinal sheet surrounding the lumen. The outer circular layer consists of the superior, middle, and inferior pharyngeal constrictor muscles (see Image. Pharyngeal Constrictors). The inner longitudinal layer comprises the palatopharyngeus, salpingopharyngeus, and stylopharyngeus muscles. The pharyngeal muscles receive dual innervation from the glossopharyngeal (ninth cranial nerve or cranial nerve IX) and vagus (10th cranial nerve or cranial nerve X) nerves, facilitating synchronous food propulsion from the oral cavity to the esophagus.[1]
Infections, muscular disorders, and malignancies can impair pharyngeal function. This structure's central location in the neck makes it a useful surgical reference point. Understanding pharyngeal anatomy and function is essential in treating various speech, deglutition, and airway disorders.
Structure and Function
The pharynx is a musculomembranous tube located posterior to the oronasal cavity, extending from the skull base to the cricoid cartilage anteriorly and the inferior C6 margin posteriorly. This tube is widest at the hyoid level and narrowest where it connects to the esophagus. The pharynx is a common pathway for the respiratory and digestive systems.
The pharyngeal tube is highly muscular. Pharyngeal muscles are arranged in layers, as described below.
Outer Circular Pharyngeal Layer
The pharyngeal constrictor muscles form the outer circular layer of the pharynx and are pivotal in swallowing. This layer consists of 3 constrictor muscles—superior, middle, and inferior.[1][2]
- Superior constrictor: This muscle originates from the pterygoid process, the posterior end of the mandible's mylohyoid line, and the pterygomandibular raphe. The superior constrictor inserts onto the pharyngeal tubercle of the skull base and the pharyngeal raphe, a midline tendinous seam where the constrictor muscles converge. Contraction of this muscle narrows the upper pharyngeal segment and closes the nasopharynx during swallowing.
- Middle constrictor: This muscle arises from the greater and lesser horns of the hyoid bone and the stylohyoid ligament. The middle constrictor also inserts onto the median pharyngeal raphe, blending with superior and inferior constrictor fibers. This muscle constricts the middle pharyngeal portion during swallowing.
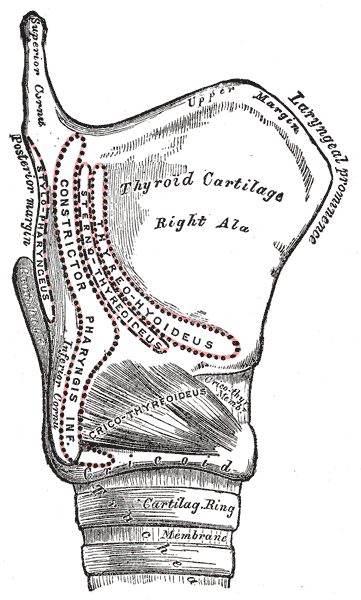
- Inferior constrictor: The inferior constrictor is subdivided into the thyropharyngeus superiorly and the cricopharyngeus inferiorly. The thyropharyngeus originates from the thyroid cartilage, whereas the cricopharyngeus arises from the cricoid cartilage and merges with the esophageal muscle. Both segments attach to the median pharyngeal raphe (see Image. Larynx, External Muscle Attachment Sites). The inferior constrictor compresses the lower pharynx.
The coordinated movements of the constrictor muscles allow them to propel food smoothly from the oral cavity into the esophagus.
Inner Longitudinal Pharyngeal Layer
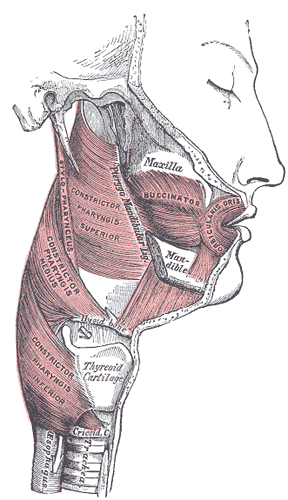
The inner longitudinal layer consists of muscles that primarily act to elevate the pharynx and larynx. This layer consists of the palatopharyngeus, salpingopharyngeus, and stylopharyngeus.[3][4][5]
- Palatopharyngeus: This muscle begins at the posterior hard palate and the palatine aponeurosis, inserting onto the thyroid cartilage. The palatopharyngeus elevates the pharynx superiorly during swallowing.
- Salpingopharyngeus: This muscle originates from the auditory tube's inferior aspect and inserts onto the palatopharyngeus muscle. Contraction of this muscle raises the pharynx and opens the auditory tube, equalizing ear pressure during swallowing.
- Stylopharyngeus: This muscle is the only pharyngeal muscle innervated by cranial nerve IX. The stylopharyngeus originates from the styloid process of the temporal bone and inserts onto the thyroid cartilage, blending with the fibers of the palatopharyngeus muscle (see Image. Muscles of the Cheek and Pharynx). Contraction of the stylopharyngeus muscle elevates both the pharynx and larynx.
These longitudinal muscles elevate the pharynx and larynx, aiding in swallowing.
Embryology
The pharyngeal muscles and their corresponding nerves originate from the third and fourth branchial (or pharyngeal) arches. The third branchial arch gives rise to the stylopharyngeus muscle and cranial nerve IX. The fourth branchial arch forms most of the pharyngeal constrictors and the superior laryngeal branch of cranial nerve X.[6]
Blood Supply and Lymphatics
The pharyngeal muscles receive their blood supply from external carotid artery branches, including the ascending pharyngeal, facial, lingual, and maxillary arteries.[7][8] Venous drainage occurs through the pharyngeal venous plexus, which empties into the internal jugular vein. Lymphatic drainage initially flows to the retropharyngeal lymph node and then to the deep cervical lymph node.[9][10]
Nerves
The pharyngeal plexus, formed by branches of cranial nerves IX and X, supplies motor and sensory innervation to the pharynx. Cranial nerve X is the principal motor nerve for the pharyngeal muscles, contributing through its pharyngeal branches. Cranial nerve X innervates all the pharyngeal muscles except the stylopharyngeus, which is supplied by cranial nerve IX.
The sensory innervation of the pharyngeal mucosa is less complex but no less critical. Cranial nerve IX provides sensory fibers to the upper pharynx and contributes mucosal membrane sensation in this region. Cranial nerve X adds to the general sensory perception of the pharynx.
Although primarily known as the motor nerve of the sternocleidomastoid and trapezius muscles, the accessory nerve (11th cranial nerve or cranial nerve XI) also contributes some fibers to the vagus nerve and indirectly influences pharyngeal muscular function. Sympathetic and parasympathetic autonomic nerves also contribute to the pharyngeal plexus. These nerves regulate the vascular and glandular elements of the pharynx but do not contribute to pharyngeal muscular function.
Physiologic Variants
The pharyngeal constrictor muscles have multiple variants. The superior constrictor can merge with the middle and inferior constrictor muscles. The inferior constrictor fuses with the superior constrictor or the posterior portion of the pharyngobasilar fascia.[11] Longitudinal muscle groups may have different insertion points, such as the palatine tonsil, epiglottis, and arytenoids. These variants may alter pharyngeal movements.
Surgical Considerations
Several surgical interventions target the pharyngeal muscles, particularly to treat conditions such as obstructive sleep apnea, dysphagia, and various pharyngeal tumors. Some of the key surgeries affecting the pharyngeal muscles are discussed below.
Uvulopalatopharyngoplasty
Uvulopalatopharyngoplasty is commonly used to treat obstructive sleep apnea. This procedure involves removing excess throat tissue to widen the airway. This surgery may include parts of the uvula, soft palate, and pharyngeal walls.[12]
Pharyngoplasty
Various pharyngoplasty techniques exist, including lateral and expansion sphincter pharyngoplasty. These procedures can reconstruct and reposition the pharyngeal muscles to reduce airway obstruction.[13]
Pharyngeal Flap Surgery
Pharyngeal flap surgery is often used to treat velopharyngeal insufficiency. This procedure involves creating a flap from the pharyngeal wall to help close the velopharyngeal sphincter during speech. The velopharyngeal sphincter is not an actual anatomical sphincter but a functional muscle and tissue group working together to close off the nasopharynx during swallowing and speaking. The muscles primarily involved in this mechanism include the palatopharyngeus, levator veli palatini, and superior constrictor muscles.[14]
Cricopharyngeal Myotomy
Cricopharyngeal myotomy may be performed to improve bolus transport in cases of block dysphagia at the cricoid level. This procedure requires cutting into the cricopharyngeus and upper esophageal muscles.[15]
Clinical Significance
Zenker Diverticulum
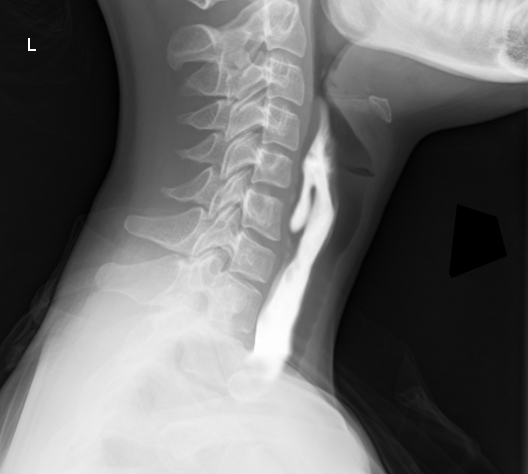
During normal swallowing, the superior thyropharyngeus contracts while the inferior cricopharyngeus relaxes, propelling food into the esophagus. Incoordination can increase intrapharyngeal pressure, promoting diverticulum formation within the weak spot between these 2 muscular segments. The pathological structure formed is called a Zenker diverticulum, which creates a site where food can accumulate and cause dysphagia (see Image. Zenker Diverticulum). Other complications of Zenker diverticula include gurgling, aspiration, foul breath, and neck mass.[16]
Pharyngitis
Pharyngitis, often caused by an infection, is characterized by pain, irritation, discomfort, and throat dysphagia. The condition may result from bacterial or viral infections. Supportive care and nonsteroidal anti-inflammatory drugs are typically recommended for viral infections. Antibiotics are prescribed for bacterial pharyngitis. Prompt treatment of Streptococcus pyogenes pharyngitis is crucial to prevent complications such as rheumatic fever and glomerulonephritis.
Fungal pharyngitis is a differential diagnosis in individuals with poor immunity or advanced age. Antifungals such as fluconazole and miconazole are typically prescribed for this condition.[17]
Dysphagia
Dysphagia is the difficulty of swallowing foods or liquids. The condition may be due to pharyngeal muscle dysmotility. Stroke may present with dysphagia if the cranial nerves supplying the pharyngeal muscles are involved.[18][19] Dysphagia in older individuals is often from an oropharyngeal or esophageal origin.[20]
Understanding pharyngeal muscle innervation helps in diagnosing and treating speech and swallowing disorders, reflecting the importance of this complex neural network.
Other Issues
Cricopharyngeal Achalasia
Cricopharyngeal achalasia is when the cricopharyngeal muscle fails to open adequately to allow food bolus passage into the esophagus. Patients may have a history of recurrent choking, regurgitation, coughing, and pneumonia. Treatment options include cricopharyngeal myotomy or botulinum toxin injection to alleviate this condition.[21]
Glossopharyngeal Neuralgia
Glossopharyngeal neuralgia is a disorder presenting with repeated pain episodes lasting seconds to minutes in the tongue, throat, ear, and tonsils. This condition is typically unilateral. The pain may be triggered or worsened by swallowing, speaking, and chewing. The etiology is believed to be due to the irritation of cranial nerve IX, although the inciting agent is rarely found. Glossopharyngeal neuralgia is often misdiagnosed as trigeminal neuralgia due to overlapping pain presentations.[22]