Introduction
The orbicularis oculi muscle, situated just beneath the eyelid skin, is crucial in eyelid movement (see Image. Muscles of the Head, Face, and Neck). This muscle extends from the medial to the lateral canthal region, enhancing the eyelid's structural integrity and functionality. The orbicularis oculi is a sphincter-like muscle arranged concentrically around the upper and lower eyelids. The main function of the muscle is to close the eyelids, and it also assists with tear drainage. The orbicularis oculi has orbital and palpebral sections, each further subdivided to meet specific functional demands.[1][2][3]
The orbicularis oculi is a facial expression muscle that may be affected by conditions such as Bell Palsy and blepharospasm. Botulinum toxin injections target this muscle to smooth dynamic periorbital wrinkles. Understanding the orbicularis oculi's normal anatomy and function is essential in treating various eye and cosmetic conditions.
Structure and Function
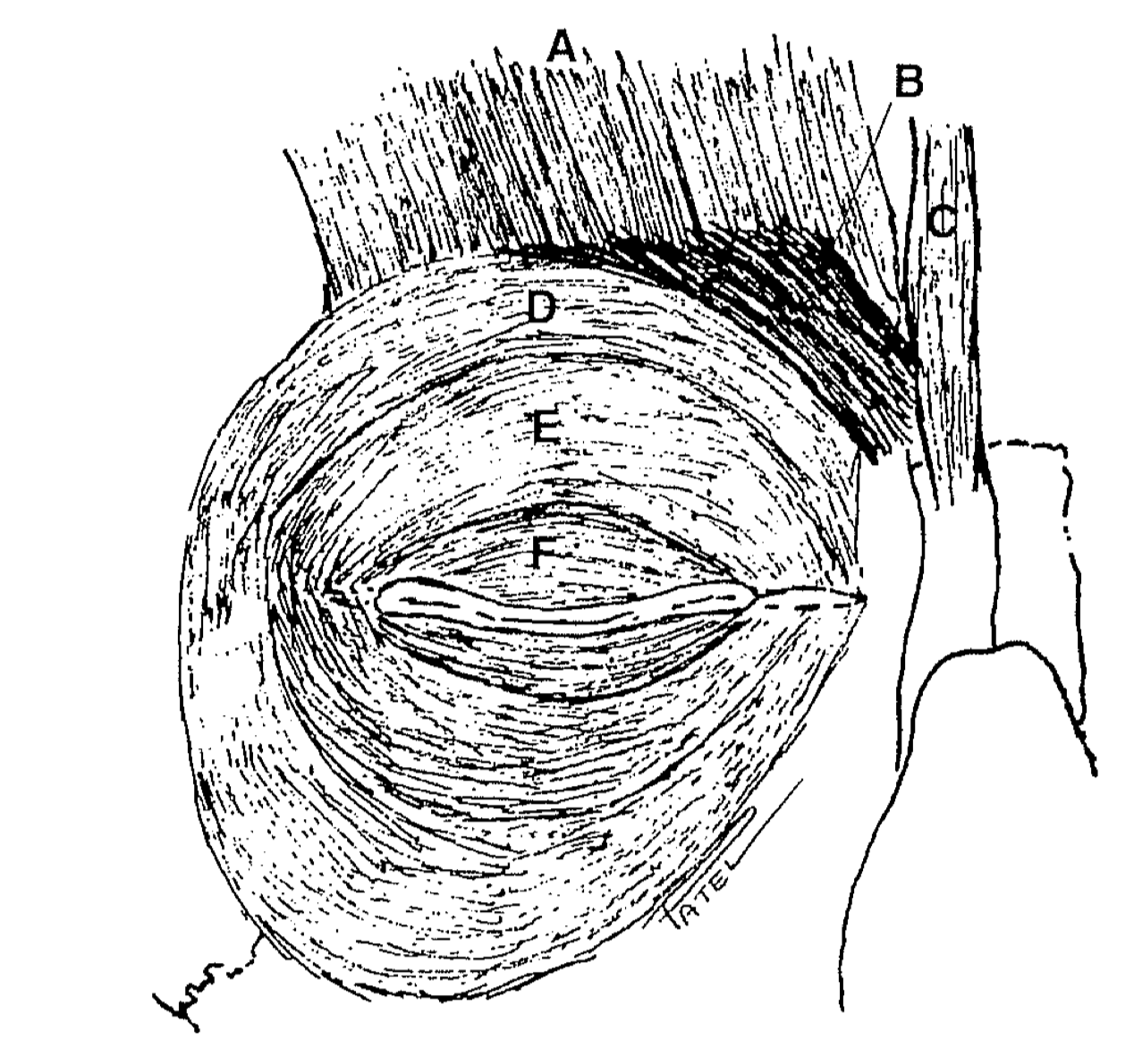
The orbicularis oculi is situated beneath the eyelid skin and is critical in eyelid movement. This muscle travels from the medial to the lateral canthal region, supporting the eyelid's structural integrity and functionality. The muscle is divided into orbital and palpebral sections, each further subdivided based on function (see Image. Orbicularis Oculi Muscle's Anatomic Relations).[4][5] The orbicularis oculi muscle inserts into the lateral palpebral raphe, the upper and lower tarsal plates, and the skin around the orbit's margin.
Orbital Section of the Orbicularis Oculi
The orbital portion of the orbicularis oculi primarily facilitates the voluntary, forceful closure of the eyelids. Medially, this section attaches to the anterior limb of the medial canthal tendon and the surrounding periosteum. Laterally, this part of the muscle connects to the lateral palpebral raphe. The orbital segment of the orbicularis oculi interdigitates with neighboring muscles along its periphery, including the frontalis, making it integral to facial expressions involving the forehead and eyebrows.
Palpebral Section of the Orbicularis Oculi
The palpebral part of the orbicularis oculi muscle is crucial for voluntary and involuntary blinking and is subdivided into the preseptal, pretarsal, and ciliary sections.
- Preseptal section: This segment of the orbicularis oculi muscle is split into deep and superficial heads. The deep head attaches to the fascia around the lacrimal sac and the posterior lacrimal crest, playing a role in the lacrimal drainage system. The superficial head attaches to the anterior limb of the medial canthal ligament. Laterally, the preseptal section connects to the Whitnall lateral orbital tubercle, situated deep to the lateral palpebral raphe.
- Pretarsal section: Similar to the preseptal section, the pretarsal section also divides into a deep and a superficial head. The deep head, often referred to as the Horner muscle, attaches posteriorly to the medial canthal tendon and the posterior lacrimal crest. The superficial head attaches anteriorly to the lacrimal crest. Laterally, this section adheres to the lateral canthal tendon. The superior and inferior aspects of the muscle section lie firmly over the upper and lower eyelid tarsi, respectively, ensuring tight closure during blinking and sleep.
- Ciliary (marginal) section: The marginal portion of the palpebral orbicularis muscle, also known as the muscle of Riolan or pars ciliaris, is adjacent to the eyelid margin. This muscle segment appears as a distinct colored line along the length of the upper and lower eyelid margins. This feature, known as the gray line, is a critical surface anatomical landmark for the surgical repair of eyelid margin lacerations, helping surgeons to precisely realign the eyelid edges for optimal healing and functional recovery.
Interaction with the Lacrimal System
The orbicularis oculi muscle interacts dynamically with the nasolacrimal duct system to facilitate tear drainage. The preseptal and pretarsal parts of the palpebral orbicularis oculi contract during blinking or eyelid closure. Consequently, the small channels draining tears from the eye's surface to the lacrimal sac called canaliculi are compressed. The muscle's action simultaneously pulls the lacrimal sac laterally and forward. These changes are critical in creating a negative pressure within the sac, effectively drawing tears and ensuring their passage down the nasolacrimal duct toward the nasal cavity.
The Orbicularis Oculi's Protective Function
Studies have focused on the anatomical specialization of the orbicularis oculi in humans, emphasizing the functional importance of its muscle fiber composition. Research has identified a predominantly type II (fast-twitch) fiber composition across the different parts of the orbicularis oculi, aligning with the muscle's rapid and protective eyelid movements. The orbicularis oculi muscle exhibits predominantly fast-twitch fibers, comprising an average of 87.8%, markedly outnumbering slow-twitch type I fibers. This characteristic is especially pronounced in the ciliary part of the muscle, where fast fibers constitute the highest percentage at 91.7%. Such fiber distribution is essential to rapid eyelid closure, facilitating a protective reflex that maintains ocular health.[6][7]
Embryology
The eyelids develop from the 8th week to the 7th month (35 mm to 250 mm) of fetal development. Specialized structures that form during this period include the orbicularis oculi. The muscle evolves through various stages along with the tarsal plates, meibomian glands, lacrimal puncta and canaliculi, skin appendages, and the conjunctiva.
The orbicularis oculi originates from the 2nd pharyngeal arch's local mesenchymal tissue and develops similarly to the extraocular muscles, evolving from mesenchymal cells to early myoblasts, myoblasts, myoblast fusion, myotubes, and ultimately, mature muscle. The orbicularis oculi initially forms as a sheet covering the lid's anterior surface. Afterward, the muscle differentiates into pretarsal, preseptal, and orbital parts by the 250-mm stage, dividing further as the upper and lower lids separate. The orbicularis oculi extends medially to attach to the medial and lateral palpebral ligaments.[8][9]
Blood Supply and Lymphatics
Arterial Supply
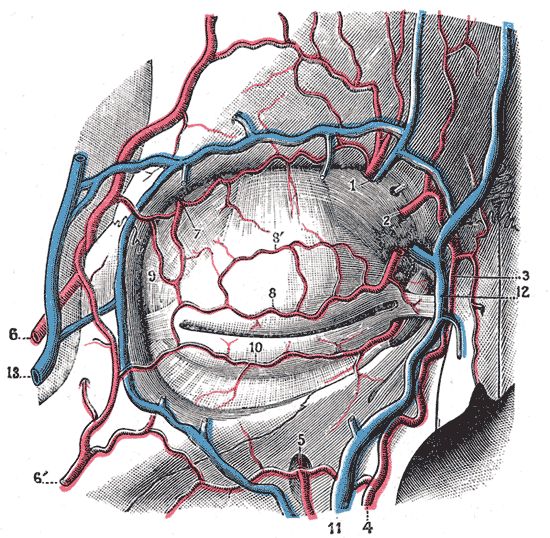
The eyelids receive arterial inflow from the distal branches of the internal and external carotid arteries. Branches of the internal carotid artery supplying the eyelids include the lacrimal, supraorbital, ophthalmic, frontal, and nasal arteries. Branches of the external carotid artery perfusing the eyelids include the superficial temporal, infraorbital, and angular arteries (see Image. Blood Vessels of the Eyelids, Front View).
Vascular Arcades in the Upper Eyelid
A significant dual-arcade system formed by the nasal and lacrimal arteries is crucial to upper eyelid vasculature. This system includes the marginal and peripheral arcades. The marginal arcade is positioned 2 to 3 mm from the eyelid margin. This arcade is crucial for the eyelid's structural integrity and function. The peripheral arcade is located along the upper tarsal border and is essential for surgical procedures, such as the creation of pedicled tarsoconjunctival flaps. By comparison, the lower eyelid's vascular structure is less defined, exhibiting more variation in arterial supply. This variability underscores the importance of precise surgical planning to achieve successful outcomes in this area.
Lymphatic Drainage of the Eyelids
Traditionally, the lymphatic drainage of the eyelids is believed to follow 2 primary pathways. Lymph from the medial parts of the eyelids typically flows toward the submandibular lymph nodes, representing medial eyelid drainage. Lymph from the lateral aspect of the eyelids typically moves toward the preauricular lymph nodes, forming the lateral eyelid drainage.[10]
However, recent studies provide a more nuanced view of eyelid lymphatic flow. Some research suggests that parts of the upper lid, the lateral lower lid, and the medial canthus drain into the parotid lymph nodes. Meanwhile, the central portion of the upper eyelid and the medial and central regions of the lower eyelid empty into the submandibular lymph nodes. These insights into the lymphatic drainage patterns are crucial for accurate diagnosis and effective therapeutic strategies, particularly in managing conditions related to lymphatic flow disruptions.[11]
Nerves
The seventh cranial nerve (facial nerve or cranial nerve VII) innervates the orbicularis oculi muscle. Intracranially, cranial nerve VII starts in the pons, transits the internal acoustic meatus, and traverses the facial canal of the temporal bone. The nerve then exits the skull through the stylomastoid foramen posterior to the styloid process of the temporal bone. Afterward, cranial nerve VII passes through the parotid gland, splitting into 5 branches that innervate the facial expression muscles. These branches are the temporal, zygomatic, buccal, marginal mandibular, and cervical branches.
The temporal branch of cranial nerve VII courses superiorly and medially to innervate the upper half of the orbicularis oculi, the frontalis, and the corrugator supercilii muscle. The zygomatic branch courses medially and innervates the lower half of the orbicularis oculi.
Muscles
About 88% of the fibers of the muscle are fast twitch (type II), while 12% are slow twitch (type 1).
Physiologic Variants
Variants of the orbicularis oculi may arise from alterations in its attachments. A case report describes muscular connections between the orbicularis oculi and orbicularis oris.[12] Another report demonstrates links between the depressor supercilii and the inferior portion of the orbicularis oculi.[13] These variants impact facial expressions and cosmetic procedure outcomes.
Surgical Considerations
The orbicularis oculi is integral to eyelid function and facial expression and significantly impacts surgical interventions, ranging from blepharoplasty to periorbital reconstruction. Blepharoplasty, often called eyelid surgery, is a cosmetic procedure that can enhance eyelid appearance while maintaining muscle integrity. The treatment corrects anatomophysiological eyelid changes due to aging. Blepharoplasties may involve the upper or lower lid or both. The procedure involves removing or repositioning excess skin, muscle, and sometimes fat, thus rejuvenating the periorbital area and making the patient look rested and alert.
The aesthetic and functional results of reconstructing periorbital defects are crucial due to the area's intricate anatomy and specialized functions. The orbicularis oculi myocutaneous flap has proven beneficial for repairing periorbital defects from conditions such as basal and squamous cell carcinoma. However, employing these flaps with diverse techniques is uncommon, depending on the location and depth of defects. This technique utilizes the orbicularis oculi muscle for its robust vascular supply and excellent color match, proving essential in reconstructing defects while maintaining eyelid functionality.[14]
Understanding the facial nerve supply around the lower eyelid is crucial for surgeries involving the orbicularis oculi to prevent inadvertent nerve damage, which could lead to functional deficits.
Clinical Significance
Proper eyelid closure is compromised if the orbicularis oculi fails to function, as observed in conditions such as Bell palsy (facial nerve paralysis). This condition requires aggressive eye lubrication using artificial tear drops and ointments to prevent exposure keratitis. Inadequate treatment can lead to severe pain, corneal scarring, ulceration, and potential corneal perforation, possibly resulting in vision loss.[15][16]
The orbicularis oculi may involuntarily contract in benign essential blepharospasm, impacting daily activities such as reading and driving due to difficulty keeping the eyes open. Periodic chemodenervation with botulinum toxin injections targeting the orbicularis oculi muscle can greatly alleviate these symptoms.[17][18]