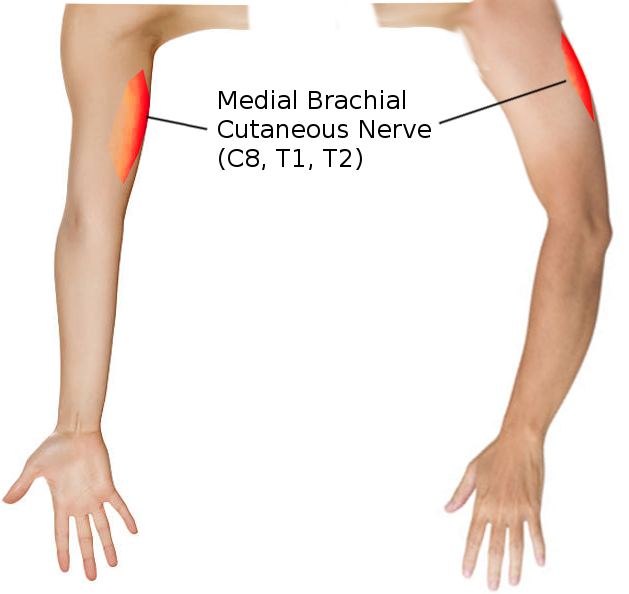
Introduction
The medial brachial cutaneous nerve, also known as the medial cutaneous nerve of the arm, provides sensation to the medial cutaneous aspect of the arm (see Image. Medial Brachial Cutaneous Nerve). It is the smallest and most medial branch of the brachial plexus, originating from C8 and T1 nerve roots.[1] As it descends the arm, it courses with the basilic vein, terminating at the distal third of the medial arm.[2] Variants exist in the amount of proximal and distal branches and the course of the median cord from which this nerve arises. Clinically, knowledge of the anatomic course of the medial brachial cutaneous nerve is essential for surgical procedures such as brachioplasty, breast augmentation, and axillary lymph node dissection.
Structure and Function
The brachial plexus originates in the cervical spine, from the anterior divisions of spinal nerves C5 to T1. It divides into roots, trunks, divisions, cords, and branches. The medial brachial cutaneous nerve arises from the medial cord of the brachial plexus, originating from the nerve roots of C8 and T1, the lower trunk, and the anterior division of the plexus.[3][4] This nerve, along with the medial antebrachial cutaneous nerve, is the only cutaneous branch that arises from the medial cord for the brachial plexus. As the medial brachial cutaneous nerve passes through the axilla, it first lies posterior to the axillary vein and then runs medial to it as its course progresses. As it descends, the medial brachial cutaneous nerve courses along the medial side of the basilic vein and then pierces the deep brachial fascia of the middle arm. It communicates with the intercostobrachial nerve proximally near its origin and distally with the ulnar branch of the medial antebrachial cutaneous nerve near the medial epicondyle.[3] It provides pain and pressure sensation to the distal third of the medial arm, the olecranon, and the medial epicondyle.[5]
Embryology
The brachial plexus, and therefore the medial brachial cutaneous nerve, have an ectodermal origin, with the bones, blood vessels, and muscles of the limbs arising from mesoderm. The limb buds are paddle-shaped structures that grow outwards gradually, starting in the fifth week of development.[6] The brachial plexus forms as spinal cord segmental nerves invade the limb bud mesenchyme. It arises from cervical segments 5 through 8 and the first thoracic segment. Early in development, a dorsal branch forms to supply the extensor muscles, and a ventral branch supplies the flexor muscles, and the pattern is conserved as the plexus becomes more complex. The limbs are positioned at birth through growth factors, including fibroblast growth factor (FGF), sonic hedgehog (SHH), and homeobox (Hox) genes.[7] FGF signaling molecules are important for anterior-posterior patterning of limb development and induce the formation of the apical ectodermal ridge at the limb bud, which controls cell death. The loss of this gene leads to the webbing between digits. The SHH signaling molecule regulates the growth of limbs and is secreted at the zone of polarizing activity on the posterior side of the limb buds. The Hox genes contribute to proximodistal limb patterning, and mutations lead to limb formation in abnormal locations.
Blood Supply and Lymphatics
Vasa nervorum are thin, tortuous arteries that supply blood to peripheral nerves, especially to the inner parts of nerves and their coverings. They are an irregular nutrient source that supplies each peripheral nerve from the neighboring blood vessels. The medial brachial cutaneous nerve gets its blood supply from the vasa nervorum arising from the axillary vein and basilic veins, respectively, along its path.
Nerves
The nerve conduction velocity of the medial brachial cutaneous nerve is about 61 +/- 4 m/s. It is possible to record the conduction velocity about 2 centimeters above the medial condyle of the humerus.
Muscles
The nerve pathway is traceable as a line between the axilla and the medial condyle of the humerus. It touches the coracobrachialis muscle and the medial area of the brachial biceps. If anatomical abnormalities are present, such as accessory coracobrachialis muscle or biceps brachialis, the nerve may have functional abnormalities in the absence of direct trauma.
Physiologic Variants
There are many anatomic variants in the medial brachial cutaneous nerve. In most individuals, proximal to the medial epicondyle, there is an arborization of 2 to 3 cutaneous branches, although few have been found to have 4 or 5.[3] On average, the number of distal branches ranges from 2 to 4.[3] In one study, the mean distance from the medial epicondyle to the distal branches was 7.8 cm, with specimens ranging from 6.5 cm to 8.6 cm. The mean distance from the medial epicondyle to the proximal branches was 15.3 cm, with specimens ranging from 13.0 cm to 16.2 cm, where it sends branches across the ulnar nerve.[3]
The variability in the course of this nerve is important for surgical dissections of the medial part of the arm. The course of the medial brachial cutaneous nerve is quite variable. One study on ten fresh cadaver specimens showed that in 9 out of 10 cadavers (18 arms), there was a link to the intercostobrachial cutaneous nerve (ICBCN).[2] This relation was rendered in the form of an ansa. The nerve travels medially and posteriorly to the ulnar nerve as it courses distally. There is a wide variety of single branches from the medial brachial cutaneous nerve to the medial part of the limb. A terminal arborization of 2 to 5 branches begins at 2 to 3 cm proximal to the medial epicondyle.[2] In 40% of the specimens, the medial brachial cutaneous nerve sent this small branch in an anterolateral direction, which crossed the ulnar nerve 10 to 12 cm proximal to the medial epicondyle. Moreover, in 1 cadaver (2 arms), the medial brachial cutaneous nerve stretched directly over the ulnar nerve for 14 cm from the root of the ulnar nerve at the medial cord before its posteromedial path.[2]
Additionally, research has found some variants in the brachial plexus where the posterior cord is absent, causing the lateral and medial cords to connect with the communicating branches and that course in front of the axillary artery.[8] As the medial brachial cutaneous nerve originates from the medial cord, this would change its course in these individuals. Therefore, caution should always be used in surgery when dissecting the arm's medial aspects, noting individual variations. In some patients, the nerve may be absent.
Surgical Considerations
The medial brachial cutaneous nerve has a significant clinical role in brachioplasty surgeries. With the rise of bariatric surgery procedures, there has also been an increased demand for plastic surgery focusing on the upper arm. Brachioplasty procedures emphasize correcting the soft tissue laxity of the middle to the upper third of the arm. Traditional procedures involve incisions from the axilla to the medial epicondyle, with the elevation of cutaneous tissue proximal to the medial epicondyle. One of the complications of Brachioplasty is an injury to cutaneous nerves within the tissues dissected, mainly the ulnar nerve and terminal branches of the medial brachial cutaneous nerve and medial antebrachial cutaneous nerve. Unfortunately, the medial antebrachial cutaneous nerve and medial brachial cutaneous nerve's anatomic path make it necessary for these nerves to cross the area where the older skin incision is typically placed.[2] Compromise of the medial brachial cutaneous nerve and the ulnar and medial antebrachial cutaneous nerves leads to decreased pressure and pain sensation in the arm. It can result in pressure ulcers over the elbow.[3] For plastic surgeons to avoid this and provide a maximal aesthetic outcome, incisions must be placed more posteriorly on the arm.[3][2]The surgeon must also avoid dissecting the deep fat layer near the axilla to avoid injuring this nerve's lymphatic vessels and the intercostobrachial nerve.[9] This nerve can also cause an injury during lymph node dissections and breast augmentation, which involves dissection of the axillary fossa.[5]
Clinical Significance
The medial brachial cutaneous nerve plays a role in upper extremity nerve entrapment syndromes, especially following axillary lymph node dissections and breast augmentation. Entrapment of this nerve should be a consideration with complaints of paresthesia over the upper arm.[5] This condition is diagnosable via ultrasound with the transducer placed on the teres major and latissimus dorsi muscles. It can be found on the distal arm parallel to the ulnar nerve. Possible entrapment of the nerve is identifiable by changes in nerve size and echogenicity, as well as hypertrophic scars on adjacent structures causing possible compression.[5]
Other Issues
The medial brachial cutaneous nerve crosses the brachial fascia. The pectoralis major muscle, latissimus dorsi muscle, and the deltoid muscle with some muscle fibers manage and influence the tension of the brachial fascia. Each arm movement influences the force vectors on the band.[10] If there is fascial dysfunction, such as adherence, a scar, or a previous trauma, the brachial fascia can abnormally draw the medial brachial cutaneous nerve, causing an entrapment syndrome. The nerve can be the subject of sports injuries, in particular, due to continuous elbow movements (extension).[11]