Continuing Education Activity
Lung cancer or bronchogenic carcinoma refers to tumors originating in the lung parenchyma or within the bronchi. It is one of the leading causes of cancer-related deaths in the United States. Since 1987, lung cancer has been responsible for more deaths in women than breast cancer. It is estimated that there are 225,000 new cases of lung cancer in the United States annually, and approximately 160,000 die because of lung cancer. It is interesting to note that lung cancer was a relatively rare disease at the beginning of the 20th century. Its dramatic rise in later decades is attributable primarily to the increase in smoking among both males and females. This activity reviews the causes, pathophysiology, and presentation of lung cancer and highlights the role of the interprofessional team in its management.
Objectives:
- Describe the pathophysiology of lung cancer.
- Review the causes of lung cancer.
- Summarize the different types of lung cancers.
- Outline the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by lung cancer.
Introduction
Lung cancer or bronchogenic carcinoma refers to tumors originating in the lung parenchyma or within the bronchi. It is one of the leading causes of cancer-related deaths in the United States. Since 1987, lung cancer has been responsible for more deaths in women than breast cancer. It is estimated that there are 225,000 new cases of lung cancer in the United States annually, and approximately 160,000 people die because of lung cancer. It is interesting to note that lung cancer was a relatively rare disease at the beginning of the 20th century. Its dramatic rise in later decades is mostly attributable to the increase in smoking among both males and females.[1][2]
Etiology
Smoking is the most common cause of lung cancer. It is estimated that 90% of lung cancer cases are attributable to smoking.[3] The risk is highest in males who smoke. The risk is further compounded with exposure to other carcinogens, such as asbestos. There is no correlation between lung cancer and the number of packs smoked per year due to the complex interplay between smoking and environmental and genetic factors. The risk of lung cancer secondary to passive smoking increases by 20 to 30%.[3] Other factors include radiation for non-lung cancer treatment, especially non-Hodgkins lymphoma and breast cancer.[4] Exposure to metals such as chromium, nickel, arsenic, and polycyclic aromatic hydrocarbons is also associated with lung cancer. Lung diseases like idiopathic pulmonary fibrosis increase the risk of lung cancer independent of smoking.[5]
Asbestos and radon are established risk factors for lung cancer as well. Asbestos exposure, particularly occupational exposure, increases the risk for lung cancer in a dose-dependent manner but varies according to the type of asbestos fiber. Nonoccupational asbestos exposure risk is less defined. However, the United States Environmental Protection Agency (EPA) has set standards for low-level acceptable nonoccupational asbestos exposure, stating that the health risk to occupants of a building in which asbestos is undisturbed without respirable particles is not significant.[6] Radon exposure in uranium miners was associated with a small but significant risk of lung cancer.[7] Radon has also been shown to accumulate in homes as a decay product of uranium and radium. A meta-analysis of European studies reported appreciable hazards from residential radon, particularly for smokers, and was responsible for approximately 2% of all deaths from lung cancer in Europe.[8]
Epidemiology
Lung cancer is the most commonly diagnosed cancer worldwide, accounting for approximately 12.4% of all cancers diagnosed worldwide, and is the leading cause of cancer-related deaths.[9] The American Cancer Society estimates an annual incidence of more than 234,000 new lung cancer cases and over 154,000 lung cancer-associated deaths in the United States.[9] According to the Global Cancer Statistics report from 2020, lung cancer remained the leading cause of cancer death worldwide, with an estimated 1.8 million deaths.[10]
Historically, the lung cancer epidemic seems to involve the developed world only. Recent data suggest that the incidence of lung cancer is dramatically rising, with nearly half of new cases, 49.9%, diagnosed in the underdeveloped world.[11] In the United States, mortality is high in men compared to women. Overall, there is no racial difference in the incidence of lung cancer, but the age-adjusted mortality rate is higher in African American males than their Caucasian counterparts. No such distinction exists between women.[3]
Pathophysiology
The pathophysiology of lung cancer is very complex and incompletely understood. It is hypothesized that repeated exposure to carcinogens, such as cigarette smoke leads to dysplasia of lung epithelium. If the exposure continues, it leads to genetic mutations and affects protein synthesis.[12] This, in turn, disrupts the cell cycle and promotes carcinogenesis. The most common genetic mutations responsible for lung cancer development are MYC, BCL2, and p53 for small cell lung cancer (SCLC) and EGFR, KRAS, and p16 for non-small cell lung cancer (NSCLC).[13][14]
Histopathological classification of lung cancers is based on cellular and molecular subtypes, which is an essential part of diagnosing and managing lung cancers. The 2021 World Health Organization (WHO) classification system of lung tumors divides the lung cancers as follows:
- Precursor glandular lesions
- Adenocarcinomas
- Adenosquamous carcinomas
- Squamous precursor lesions
- Squamous cell carcinomas
- Large cell carcinomas
- Sarcomatoid carcinomas
- Lung neuroendocrine neoplasms
- Salivary gland-type tumors
- Neuroendocrine tumors
- Neuroendocrine carcinomas
- And other epithelial tumors
According to the WHO, identifying histologic features, measuring the depth of invasion, and mode of spread is of prognostic value. For example, they state that tumor spread through air spaces is associated with a higher recurrence rate after limited resections and should be reported on pathological evaluation. Also, the previously described clear cell, rhabdoid, and signet ring subtypes have been discontinued by the most recent WHO classification as they appear to be cytologic features that can occur in any adenocarcinomas. The WHO classification places significant emphasis on immunohistochemical staining to classify cancers that may not have typical cytologic features on light microscopy. In the 2015 WHO classification system, poorly differentiated carcinomas were reclassified as squamous cell carcinomas if they had p40 expression; as adenocarcinomas with solid subtype if they had thyroid transcription factor 1 expression; and neuroendocrine carcinomas if they had chromogranin and synaptophysin positivity.
Precursor Glandular Lesions
These include atypical adenomatous hyperplasia (AAH) and adenocarcinoma in situ. AAH is a preinvasive lesion for lung adenocarcinoma and generally measures 5 mm or less. Adenocarcinoma in situ can be mucinous or nonmucinous and is generally a localized lesion of less than or equal to 3 cm. It shows a "lepidic" growth pattern defined as growth-restricted along the alveolar structures. It is noninvasive and shows intact alveolar septae.
Adenocarcinoma
Adenocarcinoma pathology consists of either neoplastic gland formation, pneumocyte marker expression (thyroid transcription factor 1 (TTF-1) with or without napsin expression, or intracytoplasmic mucin. It is further classified based on the extent and architecture of the neoplastic gland formation as mucinous or nonmucinous. Acinar, papillary, micropapillary, lepidic, and solid are nonmucinous subtypes. Pathological identification of these subtypes is important for prognosis. Solid, micropapillary, and cribriform (a subtype of acinar nonmucinous adenocarcinoma) patterns have adverse prognostic significance.[15] Although mucinous adenocarcinomas can have papillary, micropapillary, solid, and cribriform architecture, the WHO does not make any grading recommendations for mucinous carcinomas based on the growth patterns in a tumor. Other less frequent forms of adenocarcinoma include colloid, enteric-like, lymphoepithelial, and fetal.
Minimally invasive adenocarcinoma (MIA) is a small, solitary adenocarcinoma less than or equal to 3 cm with minimal invasion (less than 5 mm) and a predominant lepidic growth pattern, resembling other similar precursor glandular lesions. If the invasion is greater than 5 mm, it is defined as lepidic-predominant adenocarcinoma. Invasive mucinous adenocarcinoma, previously described as mucinous bronchioloalveolar carcinoma, comprises mucinous lesions that cannot be classified as MIA. If more than 10% of mucinous and nonmucinous growth patterns are present, the lesion should be classified as mixed adenocarcinoma.
Adenosquamous Carcinoma
Adenosquamous carcinomas are lung tumors with more than 10% glandular and squamous components. This is an uncommon and highly aggressive lung tumor, and current recommendations propose adjuvant chemotherapy even in Stage I radically resected tumors with whole-brain postoperative prophylactic radiotherapy due to the high risk of recurrence and brain metastasis with this subtype.[16]
Squamous Cell Carcinoma
Squamous cell pathology is defined by the presence of keratin and/or intercellular desmosomes on cytology or by immunohistochemistry (IHC) evidence of p40, p63, CK5, CK5/6, or desmoglein expression. Subtypes of squamous cell carcinoma include nonkeratinizing, keratinizing, and basaloid. Squamous cell carcinomas show extensive central necrosis with resulting cavitation. Squamous cell cancers can present as Pancoast tumors and hypercalcemia. A Pancoast tumor is a tumor in the superior sulcus of the lung. The brain is the most common site of recurrence postsurgery in cases of Pancoast tumors.
Large Cell Carcinoma
Large cell carcinoma (LCC) is a malignant epithelial neoplasm that does not have cytologic features consistent with glandular, squamous, or neuroendocrine cancers. They do not typically express p40 and TTF-1 on immunohistochemistry and lack cytologic features of small cell carcinoma. Typically LCC is comprised of round to polygonal cells with prominent nucleoli. The cells are large with abundant cytoplasm that does not have any defining features. LCC is a diagnosis of exclusion.[17]
Sarcomatoid Carcinoma
These are rare carcinomas that exhibit malignant epithelial components and features that suggest sarcomas. Subtypes include pleomorphic carcinoma, carcinosarcoma, and pulmonary blastoma.
Small Cell Carcinoma
Small cell carcinoma (SCLC) is composed of round, oval, or angulated cells, with a small amount of cytoplasm and size roughly that of a resting lymphocyte. No distinct nucleoli are seen. SCLCs are extensively necrotic. They usually stain positive with chromogranin or synaptophysin. The WHO previously classified SCLC into three cell subtypes: oat cell, intermediate cell, and combined cell (SCLC with NSCLC component, squamous, or adenocarcinoma). However, studies have shown that such classification does not have much clinical significance or prognostic value.[18]
History and Physical
No specific signs and symptoms exist for lung cancer. Most patients already have advanced disease at the time of presentation. Lung cancer symptoms occur due to local effects of the tumor, such as cough due to bronchial compression by the tumor due to distant metastasis, stroke-like symptoms secondary to brain metastasis, paraneoplastic syndrome, and kidney stones due to persistent hypercalcemia.[19]
Cough is present in 50 to 75% of patients with lung cancer.[2] Cough productive of large volumes of thin, mucoid secretions is seen in mucinous adenocarcinoma. In some cases, especially those with exophytic bronchial masses, a cough may signify secondary post-obstructive pneumonia. Hemoptysis is present in 15 to 30% of patients with lung cancer.[2] Chest pain is present in approximately 20 to 40% of patients with lung cancer, and dyspnea may be present in as many as 25 to 40% of the cases at the time of diagnosis.[2] These symptoms, however, may be primarily due to lung cancer or due to underlying bronchopulmonary disease.
Pleural involvement in lung cancer can manifest as pleural thickening/nodules or a malignant pleural effusion. During the course of their illness, approximately 10 to 15% of patients with lung cancer will have a malignant pleural effusion, with some showing a unilateral pleural effusion as the only presenting feature.[20] Bronchogenic carcinoma with associated ipsilateral malignant pleural effusion is considered unresectable; however, it must be noted that not all pleural effusions in patients with lung cancer are malignant.[21] A benign pleural effusion may occur due to lymphatic obstruction, post-obstructive pneumonitis, or atelectasis. If two consecutive cytology specimens are negative for malignancy in patients with bronchogenic carcinoma, surgical thoracoscopy or medical pleuroscopy is recommended to evaluate the pleural space before surgical resection of a primary lesion.[22] Medical pleuroscopy has a sensitivity of greater than 90% for detecting malignancy when present in patients with bronchogenic carcinomas.[23]
Superior vena cava syndrome with dilated neck veins, edema of the face, neck, and upper extremities, and a plethoric appearance is a common feature of small cell lung cancer. It might be the primary presentation of the disease. The chest radiograph will show widening of the mediastinum or a right hilar mass.[24] As stated above, lung cancers in the superior sulcus present as Pancoast syndrome. This presents as shoulder pain, Horner syndrome, and evidence of bony destruction, with atrophy of hand muscles.
Metastasis from lung cancer to bone is frequently symptomatic, and patients may present with bone pain at the site of metastasis in the setting of elevated serum alkaline phosphatase and hypercalcemia. Up to 20% of the patients with non-small cell lung cancer may have bone pain secondary to metastasis on initial presentation;[25] whereas the percentage is as high as 30 to 40% in patients with small-cell lung cancer.[26] Imaging usually reveals osteolytic lesions with vertebral bodies as the most common site of metastasis. Adrenal metastases also occur in lung cancer, but they are rarely symptomatic and are usually seen on staging. However, not all adrenal lesions are malignant lesions, and positron emission tomography (PET) scanning is recommended to differentiate benign from malignant adrenal lesions.[27] Brain metastasis is another common feature of lung cancer in small cell lung cancers (SCLC) and non-small cell lung cancers (NSCLC). In SCLC, brain metastases may be present in as high as 20 to 30% of the patients at diagnosis.[28] Other common sites of metastases in lung cancer include the liver, which is usually only symptomatic in advanced disease.
Paraneoplastic Syndromes Associated with Lung Cancer
Symptomatic hypercalcemia secondary to lung cancer may be due to secretion of the parathyroid hormone-related protein or due to extensive bony metastases. They present with anorexia, nausea, constipation, and lethargy as typical symptoms of hypercalcemia and have an overall poor prognosis as they tend to be associated with advanced disease.[29] The syndrome of inappropriate antidiuretic hormone secretion (SIADH) is associated with SCLC and presents with symptoms of hyponatremia.
Neurologic paraneoplastic syndromes are immune-mediated syndromes associated with SCLC and include Lambert-Eaton myasthenic syndrome (LEMS), encephalomyelitis, limbic encephalitis, cerebellar ataxia, sensory neuropathy, and autonomic neuropathy.[30] Ectopic adrenal corticotropin production can cause Cushing syndrome and is associated with SCLC, large cell neuroendocrine carcinoma, and carcinoid tumors of the lung, and it portends a worse prognosis.[31] Other extrapulmonary clinical manifestations of lung cancers include hypertrophic pulmonary osteoarthropathy, dermatomyositis, and polymyositis.
Evaluation
Lung cancer is the leading cause of death in both men and women. NSCLC accounts for 85% of diagnosed lung cancer cases in the United States.[3] The overall goal is a timely diagnosis and accurate staging. As per the American College of Chest Physicians (ACCP) guidelines, the initial evaluation should be complete within six weeks in patients with tolerable symptoms and no complications. Only 26% and 8% of cancers are diagnosed at stages I and II, respectively, whereas 28% and 38% are diagnosed at stages III and IV respectively. Therefore, curative surgery is an option for only a minority of patients.
Lung cancer evaluation can be divided as:
- Radiological staging
- Invasive staging
Goals of Initial Evaluation
- Clinical extent and stage of the disease
- Optimal target site and modality of 1st tissue biopsy
- Specific histologic subtypes
- Presence of co-morbidities, para-neoplastic syndromes
- Patient values and preferences regarding therapy
Radiologic Staging
Every patient suspected of having lung cancer should undergo the following tests:
- Contrast-enhanced CT chest with extension to upper abdomen up to the level of adrenal glands
- Imaging with PET or PET-CT directed at sites of potential metastasis when symptoms or focal findings are present or when chest CT shows evidence of advanced disease.
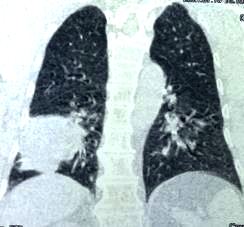
CT Scan
Intravenous (IV) contrast enhancement is preferable as it may distinguish mediastinal invasion of the primary tumor or metastatic lymph nodes from vascular structures.
The significant advantage of CT is that it provides an accurate anatomic definition of the tumor within the thorax, which helps clinicians decide the optimal biopsy site.
CT can also identify the following:
- Tumor-related atelectasis
- Post obstructive pneumonitis
- Intra- or extrathoracic metastatic disease
- Co-existing lung disease
The main objective of a CT scan is to identify the extent of the tumor, its anatomical location, and the lymph node involvement. TNM staging relies heavily on lymph node involvement. Therefore, most societies in Europe and the United States agree to regard a lymph node of 1 centimeter or more in the short axis to be considered highly suspicious for malignancy. Lymph nodes can be enlarged secondary to acute inflammation, such as congestive heart failure exacerbation or recent viral infection. The overall sensitivity and specificity of CT scan to identify malignancy are 55% and 81%, respectively. Hence, CT is not a good test for lung cancer staging.
Radiological Groups
The American College of Chest Physicians (ACCP) has proposed grouping patients based on tumor extent and lymph node involvement. Although CT is not the right staging tool, it helps the clinician select the site for tissue biopsy. In other words, based on these groups, further staging via non-invasive or invasive methods is planned.
Group A
- Patients with bulky tumors encircling/invading mediastinal structures cannot distinguish remote lymph nodes from the primary tumor.
- Mediastinal invasion is implied; therefore, no need for LN sampling. Tissue diagnosis suffices.
Group B
- Patients with discrete lymph node enlargement greater than 1 centimeter such that an isolated lymph node can be distinguished from the primary tumor
- Lymph node sampling is required for pathologic confirmation before curative intent therapy.
Group C
- Patients with a central tumor and an elevated risk of nodal disease despite normal-sized nodes, such as a high risk for N2/N3 disease.
- Lymph node sampling is needed even if CT/PET is negative due to a high N2/N3 disease risk.
Group D
- Patients with low risk of N2/N3 involvement or distant metastatic disease, such as peripheral T1 tumors.
- Invasive testing is not done routinely except if suspicion of N1 disease is high or the patient is not a candidate for surgery but going for stereotactic body radiation therapy (SBRT).
PET Scan
PET scanning allows in vivo determination of metabolic and pathologic processes. It provides limited anatomic resolution but provides information on the primary tumor's metabolic activity, mediastinal involvement, and potential distant metastases. The new integrated PET/CT scanners have eliminated the problem of unclear anatomy. The primary advantage of PET scanning is that it has reduced the number of futile thoracotomies by accurately identifying metastasis and thus excluding curative surgery as an option. PET scan is also helpful in excluding recurrent tumors after initial therapy. It also can identify recurrence versus metabolic changes post radiation therapy. False positives occur in patients with active infection and inflammation with increased glycolysis. In cases of recent lymph node sampling, a PET scan may be falsely positive. False-negative PET scans occur when there is impaired blood flow and low metabolic activity, such as with carcinoid tumors and some adenocarcinomas, and smaller lymph nodes.
PET scan has a sensitivity of 80% and specificity of 88%, which is higher than CT but not sufficient to stage lung cancer independently. Therefore, the ACCP recommends that a positive PET does not obviate the need for lymph node sampling except for group A disease.
Invasive Staging[32]
After CT and PET scans, the next step is to obtain tissue or pathologic confirmation of malignancy, confirm the staging and histological differentiation of cancer. One of the following procedures achieves this.
- Bronchoscopic endobronchial ultrasound-transbronchial needle aspiration (TBNA)
- Endoscopic-TBNA
- Mediastinoscopy
- Thoracoscopy or video-assisted thoracoscopy(VATS)
A CT-guided transthoracic biopsy is an option for peripheral lesions with a low risk of pneumothorax. Certain older procedures, such as the Chamberlain procedure, are sometimes required.[33]
Bronchoscopic TBNA
- Convex probe-endobronchial ultrasound-guided (CP-EBUS)-TBNA
- Radial probe-EBUS-TBNA (RP-EBUS)
- Navigation bronchoscopy
CP-EBUS Bronchoscopy
This is a bronchoscopic technique in which a miniature convex ultrasound of 7.5 MHZ is attached to the tip of the bronchoscope. It provides direct visualization of structures in the mediastinum or lung parenchyma through the bronchial wall. A biopsy is performed in real-time. It is mainly used to sample the mediastinal and hilar lymph nodes. The image can be frozen and measured, and there is also a Doppler available to identify blood vessels. It is the procedure of choice for this purpose. CP-EBUS is also the procedure of choice postinduction chemotherapy before surgery to confirm complete remission. CP-EBUS can be used to sample upper and lower paratracheal nodes as well as stations 10, 11, and 12. Stations 3, 5, and 6 are not accessible via CP-EBUS.
RP-EBUS Bronchoscopy
Instead of a convex probe, there is a miniature (20 to 30 MHz) probe. The advantages are that smaller lesions or more peripheral lesions can be reached, and it provides a 360-degree view of lung parenchyma. A real-time biopsy cannot be performed.
Navigation Bronchoscopy
The concept is to construct a navigational map of airways using either a CT scan or an electromagnetic field. After the map is constructed, the software creates the path to reach the location of the nodule. The bronchoscopist can create the pathway, and the software then navigates the bronchoscopist to the biopsy site.
Endoscopic-TBNA
Endoscopic ultrasonography (EUS) is becoming an increasingly useful tool for diagnosing and staging lung cancer. It can sample lymph nodes through the esophageal wall and provides a real-time sampling of stations 2, 4, 7, 8, and 9. The latter two stations cannot be sampled by endobronchial ultrasound (EBUS). It has the same sensitivity and specificity as EUS, 89%, and 100% respectively. There is also a growing trend to combine EBUS and EUS as minimally invasive lung cancer staging techniques.[33]
Mediastinoscopy
Mediastinoscopy was formerly the gold standard for lung cancer diagnosis and staging. It is mainly used to sample lymph nodes after negative needle technique and when the patient is still at high risk for cancer due to lymph node size or FDG uptake on a PET scan. Most commonly, para-tracheal lymph nodes are sampled. Alternatively, an anterior mediastinoscopy (Chamberlain procedure) can be performed to access subaortic and para-aortic nodes, stations 5 and 6, respectively. Mediastinoscopy has a sensitivity of 78% and specificity of 100%. Like all surgical procedures, mediastinoscopy has some risks. General anesthesia is required, and the procedure carries a mortality risk of 0.08%.[32][34]
Thoracoscopy
Traditionally, thoracoscopy was performed by dividing the ribs and opening the chest cavity. Like laparoscopic surgery, it has largely replaced open abdominal surgeries. Video-assisted thoracoscopy surgery (VATS) has replaced thoracoscopy. It is used to treat several chest wall, pleural, pulmonary, and mediastinal conditions. Mediastinal lymph node sampling and full dissection during lung resection for cancer can be performed with VATS. A newer version of VATS is called RATS (robotic-assisted thoracoscopy). There are no trials comparing VATS and RATS for mediastinal lymph node biopsy.
Treatment / Management
Treatment of Non-Small Cell Lung Cancer (NSCLC)
Stage I
Surgery is the mainstay of treating stage 1 NSCLC. The procedure of choice is either lobectomy or pneumonectomy with mediastinal lymph node sampling. The 5-year survival is 78% for IA and 53% for IB disease. In patients who do not have the pulmonary reserve to tolerate pneumonectomy or lobectomy, a more conservative approach with wedge resection or segmentectomy can be done. The disadvantage is a higher local recurrence rate, but survival is the same. Local postoperative radiation therapy or adjuvant chemotherapy has not been shown to improve outcomes in stage I disease.
Stage II
The survival of stage IIA and IIB lung is 46% and 36%, respectively. The preferred treatment is surgery followed by adjuvant chemotherapy. If the tumor has invaded the chest wall, then an en-bloc resection of the chest wall is recommended. Pancoast tumor is a unique tumor of stage II. It arises from the superior sulcus and is usually diagnosed at a higher stage, IIB or IIIA. The treatment of choice in cases of Pancoast tumor is neoadjuvant chemotherapy, usually with etoposide and cisplatin and concurrent radiotherapy followed by resection. Overall survival is 44% to 54% depending on postsurgery presence or absence of microscopic disease in the resected specimen.
Stage III
This is the most heterogeneous group, consisting of a wide variety of tumor invasion and lymph node involvement.
In stage IIIA disease with N1 lymph nodes, surgery with curative intent is the treatment of choice. Unfortunately, a significant number of patients are found to have an N2 disease at the time of resection. The current consensus is to perform surgery as planned, followed by adjuvant chemotherapy. There is no agreement on treatment for patients with stage IIIA tumors with N2/N3 lymph nodes. If the patient has good performance status and no weigh-loss, then concurrent chemo-radiotherapy affords the best outcome. However, concurrent chemo-radiotherapy is not as tolerated and can cause severe esophagitis. Sequential therapy is better tolerated. Survival is 40% to 45% in the first two years, but five-year survival is only 20%.
T4 tumors are usually treated exclusively with chemoradiation. Surgery may be an option in T4 N0-1 tumors with carinal involvement. The operative mortality of carinal resection is 10% to 15%, and survival is approximately 20%. If a tumor is T4 due to ipsilateral nonprimary lobe nodules with no mediastinal involvement, then surgery alone renders five-year survival of 20%
Stage IIIB tumors are treated the same way unresectable IIIA cancers are treated, with concurrent chemo-radiotherapy. For a select few patients, post-induction chemo-radiotherapy, surgery might be an option. The trials on the survival of patients with IIIB tumors also included inoperable IIIA tumors; therefore, the survival in IIIB patients is unknown.
Stage IV
Stage IV disease is considered incurable, and therapy is aimed at improving survival and alleviating symptoms. Only 10% to 30% of patients respond to chemotherapy, and only 1% to 3% survive five years after diagnosis. Single or double drug-based chemotherapy is offered to patients with functional performance status. There is a small survival benefit from chemotherapy.
In highly select patients, non-squamous NSCLC without brain metastasis or hemoptysis might benefit from the addition of bevacizumab, a vascular endothelial growth factor (VEGF) inhibitor.[35]
Targeted Therapy for NSCLC
In the early 2000s, researchers discovered that specific mutations encode critical proteins for cell growth and replication. These mutations were named “driver mutations.” It was proposed that blocking these mutation pathways may improve survival in lung cancer patients. The current practice is to check for the following mutations in every advanced NSCLC. Each of these mutations has a specific inhibitor available:
- EGFR (epidermal growth factor receptor) is a mutation inhibited by tyrosine kinase inhibitors erlotinib, gefitinib, and afatinib.[36]
- ALK (Anaplastic lymphoma kinase) includes the specific inhibitors crizotinib, ceritinib, and alectinib. A structurally similar mutation is ROS-1. The FDA recently approved crizotinib for treating cancers expressing ROS-1 mutation.
Immunotherapy for NSCLC
Immunotherapy boosts the immune system and helps it recognize cancer cells as foreign, and increases their responsiveness. There are several check-points to decrease autoimmunity and autodestruction of the body’s cells by the immune system. Malignant cells co-opt these check-points and create tolerance in the immune system. Of these check-points, programmed-death receptor 1 (PD-1) has been of particular interest recently. PD-1 plays an important role in down-regulating T-cells and promotes self-tolerance. However, it also renders the immune system less effective against tumor cells. PD-1 interacts with two proteins: PD-L1 and PD-L2. This binding results in the inactivation of activated T-cells. At the moment, there are antibodies approved for PD-1 and its ligand, PD-L1 only. They inhibit the PD-1 receptor directly or bind to PD-L1, thus preventing it from inactivating the activated T-cell.
Nivolumab is an IgG4 monoclonal antibody against PD-1. It is approved by the FDA for squamous and non-squamous NSCLC that has progressed after platinum-based chemotherapy. It can be used in patients with high or low PD-L1 expression status. Pembrolizumab is also an IgG4 monoclonal antibody against PD-1. It is approved for pre-treated metastatic NSCLC with greater than 50% expression of PD-L1 and does not harbor EGFR and ALK mutations. It is also combined with pemetrexed and carboplatin for metastatic non-squamous NSCLC with less than 50% expression of PD-L1. Atezolizumab is an IgG1 antibody against PD-L1. It is approved for use in metastatic, progressive NSCLC during or following treatment with platinum-based chemotherapy. It can be used in patients who express EGFR and ALK mutations and fail targeted therapy. Bevacizumab is not considered immune therapy. It is an anti-angiogenesis antibody that inhibits vascular endothelial growth factor A (VEGF-A). It is primarily used in combination with platinum-based chemotherapy to treat non-squamous NSCLC. It is contraindicated in squamous cell NSCLC due to the risk of severe and often fatal hemoptysis. It is also used to treat breast, renal, colon, and brain cancers.[37][13]
Small Cell Lung Cancer Treatment
SCLC is very sensitive to chemotherapy, but unfortunately, has a very high recurrence rate. Treatment for SCLC is according to the stage of the disease.
Treatment of Limited-stage Small Cell Lung Cancer
Stage I limited-stage small cell lung cancer (LS-SCLC) is lobectomy followed by adjuvant chemotherapy. These include SCLC presenting as peripheral nodules without mediastinal or hilar lymphadenopathy. Care should be taken in completely ruling out lymph node involvement. This is done by PET-CT followed by lymph node sampling by EBUS bronchoscopy or mediastinoscopy even if PET-CT was negative for lymph node size or FDG uptake.
LS-SCLC with mediastinal or hilar lymph node involvement is 4 to 6 cycles of chemotherapy followed by radiation therapy. Radiation therapy is indicated to avoid recurrence since nearly 80% of SCLC will recur locally without radiation therapy. There are multiple approaches to treatment, including concurrent and alternate chemo-radiotherapy or sequential treatments. Concurrent and alternative paths have slightly better outcomes, although they are more toxic than other approaches. Sequential therapy is much better tolerated.
In patients who achieve remission, prophylactic whole brain radiation is also done. This significantly reduces symptomatic brain metastasis and increases overall survival.
Treatment of Extensive-stage Small Cell Lung Cancer (ES-SCLC)
Extensive stage small cell lung cancer (ES-SCLC) includes distant metastasis, malignant pleural or pericardial effusions, contralateral hilar, or supraclavicular lymph node involvement. Treatment is with platinum-based chemotherapy. Up to 50% to 60% of patients show remission and should be offered radiation therapy followed by prophylactic whole-brain irradiation. Median survival from the time of diagnosis of ES-SCLC is only 8 to 13 months, and only about 5% of patients survive two years postdiagnosis.
Differential Diagnosis
- Bacterial pneumonia
- Bronchitis
- Mycoplasmal pneumonia
- Pleural effusion
- Pneumothorax
- Tuberculosis
- Viral pneumonia
- Fungal pneumonia
Staging
Lung Cancer Staging
After a lung cancer diagnosis, the most crucial step is to stage the disease because the state dictates treatment options, morbidity, and survival. It is of paramount importance that this is done with utmost vigilance. Staging is primarily done for NSCLC using the TNM classification. SCLC also can be staged in the same way, but a much more straightforward approach is used for limited disease and extensive disease.
Tumor, node, metastasis staging of non-small cell lung cancer
Tumor (T), node (N), and metastasis (M) is internationally accepted way of staging NSCLC. It is comprehensive in defining tumor size and extent, location, and distant spread, which helps clinicians draw meaningful conclusions regarding the best treatment, avoid unnecessary surgeries and provide a timely referral to palliative care if the cure is not an option. The most recent TNM classification is the eighth edition, and it is effective in the United States from January 1, 2018. Outside the United States, it was accepted on January 1, 2017, by the Union of International Cancer Control (UICC).
For the eighth edition, Ithe International Association of the Study of Lung Cancer (IASLC) studied and analyzed data from 16 countries, including approximately 95,000 patients from 1999 to 2010.[38]
Tumor
A primary tumor is divided into five categories, and each category is then further subdivided depending on the size, location, and invasion of surrounding structures by the tumor.
T0
- No primary tumor
- T Carcinoma in situ
T1 (less than 3 cm)
- T1mi: minimally invasive tumor
- T1a: superficial tumor confined to central airways (tracheal or bronchial wall)
- T1a: Less than 1 cm
- T1b: Greater than 1 cm but less than 2cm
- T1C: Greater than 2 cm but less than 3cm
T2
- T2: Greater than 3 cm but less than 5 cm
- T2a: Greater than 3 cm but less than 4cm
- T2b: Greater than 4 cm but less than 5cm
- Also considered a T2 tumor if involving main bronchus but not carina, visceral pleura or causes atelectasis to the hilum.
T3
- T3: Greater than 5 cm but less than 7 cm)
- T3 Inv: invasion of the chest wall, pericardium, or phrenic nerve
- T3 Satell: separate tumor nodules in the same lobe
- Also considered T3 tumor if involving the pericardium, phrenic nerve, chest wall, or separate tumor nodules in the same lobe
T4
- T4: Greater than 7 cm)
- T4inv: Invading the above structures
- T4Ipsi nod: Nodules in an ipsilateral lobe
It is also considered T4 tumor if it involves the heart, esophagus, trachea, carina, mediastinum, great vessels, recurrent laryngeal nerve, spine or tumor nodules in the different ipsilateral lobe. Invasion of the diaphragm is now considered a T4 tumor compared to a T3 tumor in the seventh edition of TNM classification.[39]
Thoracic Lymph Nodes
Lung cancer staging also depends upon the extension of cancer to the lymph nodes corresponding to the primary tumor as well as the opposite hemithorax. It is imperative to rule out lymph node metastasis before attempting curative surgery. Lung resection in itself carries high morbidity and mortality. Therefore, it should not be attempted if a cure is not possible.
Historically, thoracic lymph nodes were first classified in the 1960s by Naruke. This map was accepted by North America, Europe, and Japan. Later, in the 1980s and early 90s, further refinements were made to improve imaging and invasive testing improvements. Hence, two lymph node maps gained popularity in North America.
- American thoracic society (ATS-Map)
- American Joint Committee on Cancer (AJCC). This was an adaptation of the Naruke map.
In 1996, the differences in the above two were resolved in the Mountain-Dressler modification, MD-ATS Map. It was accepted in North America but only sporadically in Europe.
The International Association of Study of Lung Cancer (IASLC) attempted to resolve the differences between the MD-ATS and the Naruke maps. The IASLC lymph node map is now the most widely accepted lymph node classification system utilized worldwide.
Thoracic lymph nodes can be divided into mediastinal or N2 and hilar or N1 lymph nodes. N2 nodes are more important because they differentiate in cancer stages and, therefore, treatment options.
Much care has been taken in defining the N2 nodes in all the lymph node maps. We will attempt to explain the classification under the broad headings of the mediastinal and hilar groups and then further explain the individual mediastinal stations per the IASLC map.
Mediastinal Lymph Nodes
They are subdivided into the following groups or stations:[40]
- Supraclavicular nodes, station 1
- Superior mediastinal nodes, station 2 to 4
- Aortic nodes, station 3
- Inferior mediastinal lymph nodes, station 4
Supraclavicular Nodes (Station 1)
It includes lower cervical, supraclavicular and sternal notch nodes. Lymph nodes are further divided into 1R and 1L, corresponding to the right and left sides of the body, respectively. The distinction between 1R and 1L is an imaginary midline of the trachea that serves as the boundary. Below station 1, the left tracheal border is considered the boundary is differentiating between right and left-sided lymph nodes.
Superior Mediastinal Lymph Nodes (Station 2 to 4)
These lymph nodes occupy the superior mediastinum, hence, named accordingly. They are further subdivided into the following groups:
Upperparatracheall (station 2R and 2L)
- 2R nodes extend to the left lateral border of the trachea.
This extends from the upper border of the manubrium to the intersection of the caudal margin of the innominate (left brachiocephalic) vein with the trachea.
- 2L nodes extend from the upper border of the manubrium to the superior border of the aortic arch. 2L nodes are located to the left of the left lateral border of the trachea
Pre-vascular (station 3A)
These nodes are not adjacent to the trachea like the nodes in station 2, but they are anterior to the vessels.
Pre-vertebral (station 3P)
Nodes not adjacent to the trachea like the nodes in station 2, but behind the esophagus, which is pre-vertebral
Lower para-tracheal (station 4R and 4L)
- 4R nodes extend from the intersection of the caudal margin of the innominate (left brachiocephalic) vein with the trachea to the lower border of the azygos vein. 4R nodes extend from the right to the left lateral border of the trachea.
- 4L nodes extend from the upper margin of the aortic arch to the upper rim of the left main pulmonary artery
Aortic Lymph Nodes (5 and 6)
This group includes:
Sub-aortic nodes (station 5)
These nodes are located lateral to the aorta and pulmonary trunk in the so-called AP window.
Para-aortic node (station 6)
These are ascending aorta or phrenic nodes lying anterior and lateral to the ascending aorta and the aortic arch.
Inferior Mediastinal Lymph Nodes (Station 7 to 9)
This group includes sub-carinal and para-esophageal nodes:
Sub-carinal nodes (station 7)
They extend in a triangular fashion from the division of carina superiorly to the lower border of the bronchus intermedius on the right and the upper border of the lower lobe bronchus on the left.
Para-esophageal nodes (station 8)
These nodes are situated adjacent to the right and left sides of the esophageal wall. Both stations 7 and 8 are located below the carina.
Pulmonary Ligament (station 9) They are located within the pulmonary ligaments extending from the inferior pulmonary vein up to the diaphragm.
Hilar Lymph Nodes (Station 10 to 14)
These are all N1 nodes. These include nodes adjacent to the main stem bronchus and hilar vessels. On the right, they extend from the lower rim of the azygos vein to the interlobar region. On the left, from the upper rim of the pulmonary artery to the inter-lobar region.
Lymph Node Classification (N)
N0: No lymph node involvement
N1: Involvement of ipsilateral hilar nodes
- N1a: single station N1 nodes
- N1b: multiple-station N1 nodes
N2: Involvement of mediastinal nodes
- N2a1: Single station N2 nodes without N1 involvement (skip metastasis)
- N2a2: Single station N2 nodes with N1 involvement
- N2b: Multiple station N2 involvement
N3: Involvement of contralateral mediastinal or hilar lymph nodes[41]
Metastasis (M)
- M0: No distant metastasis
- M1a: Malignant pleural / pericardial effusion or nodules
- M1b: Single extra-thoracic metastasis
- M2: Multiple extra-thoracic metastases
Tumor Node Metastasis Staging of Lung Cancer
Occult cancer: TX N0 M0
Primary cancer not found; no lymph node or distant metastasis.
Stage 0
Stage I
IA1
IA2
IA3
IB
Stage II
IIA
IIB
- T1a / T1b / T1c N 1 M 0
- T2a / T2b N 1 M 0
- T3 N 0 M 0
Stage III
IIIA
- T1a / T2b / T2c N 2 M 0
- T2a / T2b N2 M 0
- T3 N 1 M 0
- T4 N 0 / N 1 M0
IIIB
- T1a / T1b / T1c N 3 M 0
- T2a / T2b N 3 M0
- T3 N 2 M 0
- T4 N 2 M 0
IIIC
Stage IV
IVA
IV B
Staging for all Small Cell Lung Cancer
- SCLC staging can be done using the TNM system, but since SCLC is considered a systemic disease, a more straightforward classification has been used successfully since the 1950s. There is a growing body of evidence that TNM rating may better define SCLC, but there is no consensus on this approach yet.
- SCLC is classified as LS-SCLC and ES-SCLC small cell based on the Veterans Affairs Lung study group (VALSG) classification.
- LS-SCLC is confined to the ipsilateral hemithorax and local lymph nodes, both mediastinal and hilar and supraclavicular nodes can be included in a single tolerable radiotherapy port (corresponding to TNM stages I through IIIB).
- ES-SCLC has tumors beyond the boundaries of limited disease, including distant metastases, malignant pericardial or pleural effusions, and contralateral supraclavicular and contralateral hilar involvement.[14]
Prognosis
Prognosis of NSCLC
The TNM stage at presentation in patients with NSCLC has the most significant impact on prognosis. A higher TNM stage correlates with advanced disease and poor outcomes. Other factors indicative of poor prognosis include performance status at the time of diagnosis, anorexia, weight loss, and the presence of liver or skin metastases.[42] Molecular studies have revealed that patients with activating mutations of EGFR in patients with adenocarcinoma have a better prognosis than those without EGFR mutations.[43]
Prognosis of SCLC
The extent of disease and the stage at presentation is the most important prognostic factor for SCLC. Patients with the limited-stage disease have a five-year survival rate of 10 to 13%, whereas patients with the extensive-stage disease have a five-year survival rate of 1 to 2%.[44] Similar to NSCLC, performance status and weight loss are independent prognostic factors for SCLC, where patients with poor performance status and/or weight loss at the time of diagnosis have a decreased survival rate.
Complications
Complications of lung cancer such as thrombosis and paraneoplastic syndromes are discussed above. Common complications seen in patients undergoing treatment for lung cancer include:
- Chemotherapy-induced nausea and vomiting
- Fatigue
- Anorexia
- Weight loss
- Anemia
- Neutropenia
- Nephrotoxicity (especially in patients receiving cisplatin-based therapies)
- Neurotoxicities
Deterrence and Patient Education
The single most important preventive measure is smoking cessation in all individuals. Patients should be advised about the clinical correlation of lung cancer with smoking at every clinician visit. Another important method of decreasing the morbidity and mortality associated with lung cancer is effective screening. A low-dose helical computed tomography (LDCT) is indicated for high-risk individuals for primary prevention. Smokers between the ages of 66 to 80 years benefit more from screening than those aged 55 to 64 years.[45]
Patients without a history of smoking do not benefit from lung cancer screening. Multiple other models incorporating clinical factors such as a history of lung disease, family history of lung cancer, and asbestos exposure have been developed. They can be applied to determine at-risk individuals who may benefit from screening. Current guidelines by the United States Preventive Services Task Force (2021) recommend an annual LDCT for patients aged 50 to 80 years who are at high risk of lung cancer due to their smoking history.[46] High-risk individuals are defined as those who have a greater than or equal to 20 pack-year smoking history and are either actively smoking or have quit within the past 15 years.
Pearls and Other Issues
Palliative Care in Lung Cancer
All therapeutic options, surgery, chemotherapy, and radiation have a role in managing pain and other symptoms in terminal lung cancer patients.
Surgery results in better outcomes in patients with at least three months of expected survival and good performance status. Surgical procedures for palliation include tumor bypass procedures, partial resection of the tumor, and removal of metastasis. Surgical intervention may be beneficial in patients with lung cancer if there is airway obstruction, hemoptysis, pleural or pericardial exudate, or metastases to the brain or bone. Almost 30% of lung cancer patients experience central airway occlusion, and bronchoscopic laser destruction followed by stent placement provides immediate relief in such patients.[47] Chemotherapy helps alleviate symptoms of pain and cough and may prolong survival. Palliative radiation provides symptomatic relief in 41% to 95% of lung cancer patients. Almost 60% of lung cancer patients, regardless of type and stage, receive radiation treatments during their course of illness. Radiation plays a crucial role in alleviating pain symptoms due to metastasis, particularly brain and bone metastasis. Endoscopic treatment, such as brachytherapy, helps control symptoms due to airway narrowing.[48][49]
Enhancing Healthcare Team Outcomes
Despite all the advances, the outcomes for lung cancer remain abysmal. The key reason is that most patients are diagnosed with advanced-stage disease. To improve outcomes, an interprofessional team approach with close communication between the members may perhaps lead to earlier diagnosis and treatment.
Most patients with lung cancer are first seen by the primary care provider, nurse practitioner, or internist. These clinicians need to have a high suspicion of lung cancer in smokers and others with occupational exposures and order the appropriate imaging tests when indicated. Referral to a thoracic surgeon should be done on a timely basis.
The thoracic surgeon's definitive diagnosis and management plan for lung cancer are made in collaboration with the radiologist and pathologist.
After surgery, nurses usually monitor the patients for oxygenation, ventilation, and pain. Since many of these patients are smokers, they also have other comorbidities like heart disease and peripheral vascular disease, which often present with symptoms in the post-operative period. Thus, nurses must be extra vigilant for physical abnormalities and communicate with the surgeon.
After surgery, patients need prolonged rehabilitation. Some may need chemotherapy and radiation, and hence the oncology nurse should educate the patients on the procedures and protocols. The specialized oncology pharmacist should educate the patient on the chemotherapeutic drugs, their benefits, and their adverse effects. Oncology board-certified pharmacists can consult with the oncologist on the regimens for chemotherapy and the alternatives based on patient response.
Due to high incidence and mortality, there has been a worldwide interest in developing a screening program for lung cancer. A landmark study, the National Lung Screening Trial, showed an overall decrease in mortality of 6.7% with screening. Currently, lung cancer screening is offered to men and women 55 years or older who have smoked 30 pack-years or more or have quit smoking less than 15 years ago.[50][51]
Lung cancer screening uses a low-dose helical CT scan of the chest which takes less than 25 seconds. A significant drawback of screening is the detection of benign lesions, resulting in a relatively high number of unnecessary biopsies, surgeries, or continued radiological follow-ups.[5] The key is for the interprofessional team to communicate and determine the best course of action. A collaborative interprofessional team can greatly improve clinical outcomes for this disease. [Level 5]