Introduction
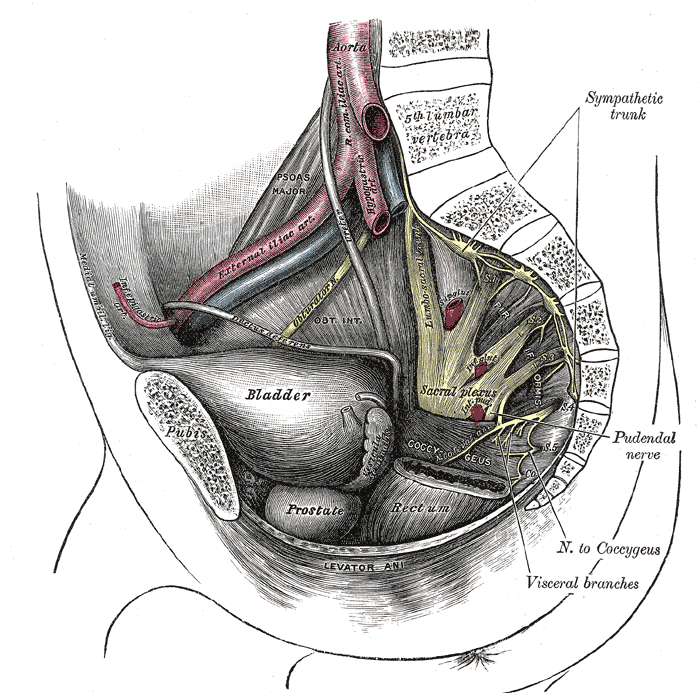
The lumbosacral plexus arises as a cordlike structure from the ventral rami of the fourth and fifth lumbar nerve roots. The nerve trunk passes over the sacral ala to join the sciatic portions of the sacral plexus. Lumbosacral branches contribute to the innervation of various parts of the lower limb (see Image. Nerves and Blood Vessels in the Pelvis).
Structure and Function
The lumbosacral trunk is a collection of neural fibers originating from L4 and L5 ventral rami and interconnecting the lumbar and sacral nerve plexi. Lumbosacral nerve fibers run on the medial side of the psoas major muscle, then inferiorly over the pelvic brim to join the first sacral nerve.
The lumbosacral trunk gives rise to the following nerves:
- Sciatic nerve
- Superior gluteal nerve
- Inferior gluteal nerve
- Nerve to the internal obturator and superior gemellus muscles
- Nerve to the quadratus femoris and inferior gemellus muscles
Embryology
The neural plate forms during the third week after fertilization, giving rise to the neural tube and neural crest cells. The neural crest cells form the peripheral nerves, including the nerves of the lumbosacral trunk. Schwann cells also arise from neural crest cells and myelinated nerves in the peripheral nervous system.
Blood Supply and Lymphatics
Peripheral nerves have 2 arterial sources. The arterial sources include intrinsic supply from the vasa nervorum within the epineurium and extrinsic supply from parallel-running arteries.
Nerves
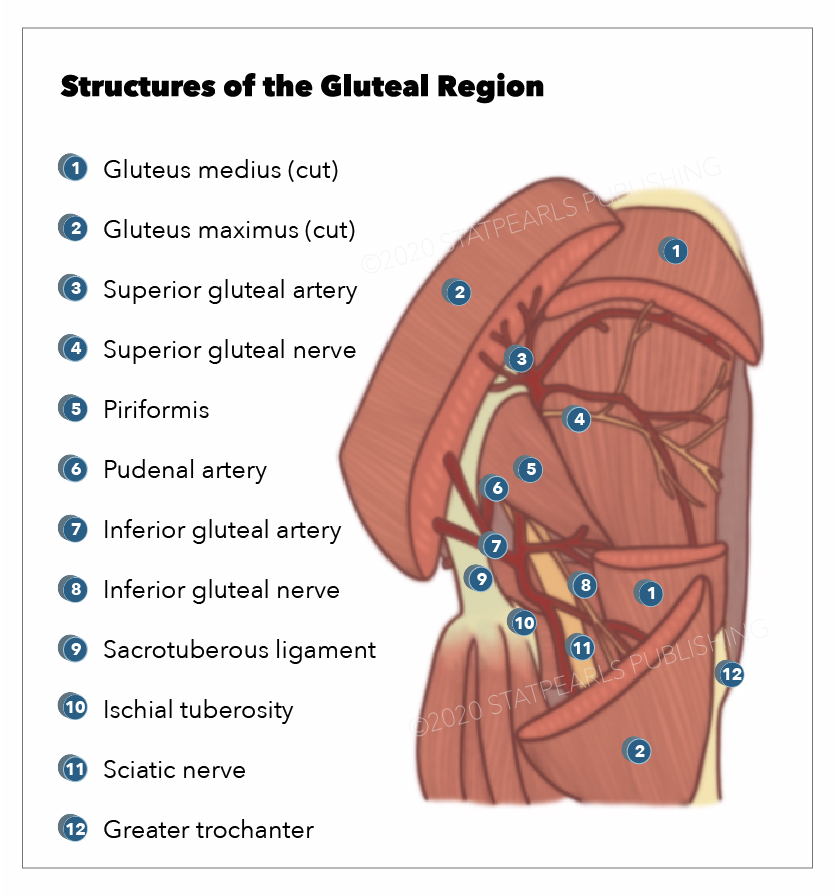
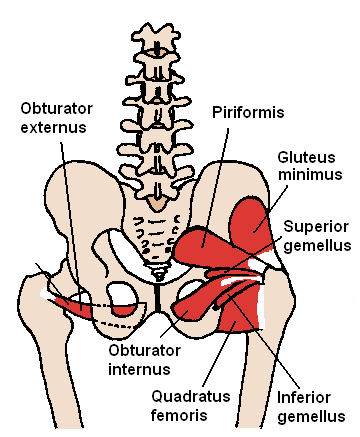
Lumbosacral nerve branches include the following nerves (see Image. Gluteal Region):
Sciatic Nerve
The sciatic nerve, the body's largest nerve, originates from the fusion of L4-S3 fibers. It runs beneath the piriformis muscle, exits the pelvis through the greater sciatic foramen, and then divides into the tibial and common peroneal (fibular) nerves in the popliteal fossa.[1]
Superior Gluteal Nerve
The superior gluteal nerve originates from dorsal fibers in the L4-S1 region and exits the pelvis through the greater sciatic foramen above the piriformis muscle. It travels alongside the superior gluteal artery and vein, taking a path above the piriformis (it is the only nerve that travels this route). The superior gluteal nerve supplies the gluteus medius, gluteus minimus, and tensor fascia lata muscles.[2]
Inferior Gluteal Nerve
The inferior gluteal nerve originates from dorsal branches in the L5-S2 region and exits the pelvis through the greater sciatic foramen beneath the piriformis muscle. Its primary function is to innervate the gluteus maximus muscle.[3]
Nerve to the Internal Obturator and Superior Gemellus Muscles
The nerve supplying the internal obturator and superior gemellus muscles originates from L5-S2 fibers and exits the pelvis through the greater sciatic foramen to innervate these muscles.
Nerve to the Quadratus Femoris and Inferior Gemellus Muscles
The nerve innervating the quadratus femoris and inferior gemellus muscles originates from L4-S1 fibers. It descends along the ischium behind the hip joint and provides innervation to these muscles.
Muscles
Muscles Innervated by the Sciatic Nerve
The sciatic nerve innervates the posterior thigh muscles (see Image. Posterior Hip Muscles), which include the biceps femoris, semitendinosus, semimembranosus, and the ischial aspect (hamstring part) of the adductor magnus. The posterior thigh muscles extend the thigh, flex the leg, and rotate the knee. The hamstring part of the adductor magnus extends the thigh.[4][5]
The sciatic nerve also innervates the posterior leg and foot sole muscles via the tibial nerve. These muscles either flex the knee, flex the toes, or plantarflex the ankle. They include the following:
- Superficial: gastrocnemius, soleus, and plantaris
- Deep: popliteus, flexor hallucis longus, flexor digitorum longus, and tibialis posterior
The common peroneal nerve innervates the following muscles:
- Anterior compartment: tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus (fibularis) tertius
- Lateral compartment: peroneus longus and peroneus brevis
The actions of the anterior leg compartment muscles include ankle dorsiflexion, toe extension, foot inversion, and slight foot eversion. Lateral leg compartment muscles evert the foot and assist in ankle plantar flexion.
Muscles Innervated by the Superior Gluteal Nerve
The superior gluteal nerve innervates the gluteus medius, gluteus minimus, and tensor fascia lata. The gluteus medius and minimus function together to abduct the hip, internally rotate the flexed hip, and externally rotate the extended hip. The tensor fascia lata flexes, medially rotates, and abducts the hip while externally rotating the leg at the knee.
Muscles Innervated by the Inferior Gluteal Nerve
The inferior gluteal nerve innervates the gluteus maximus, which externally rotates and extends the thigh at the hip joint. The nerve also attaches to the iliotibial tract laterally to support the extended knee.
Inferior gluteal nerve injuries may result in difficulty rising from a sitting position and climbing the stairs. Both movements require concerted actions from the gluteus maximus and a muscle group innervated by the femoral nerve, the quadriceps femoris.
Nerve to the Internal Obturator and Superior Gemellus Muscles
As the name implies, this nerve innervates the internal obturator and superior gemellus. The internal obturator abducts the thigh, externally rotates the extended thigh, and stabilizes the hip while walking. The superior gemellus helps with externally rotating the thigh.
Nerve to the Quadratus Femoris and Inferior Gemellus Muscles
The quadratus femoris externally rotates and adducts the thigh. The inferior gemellus is an external rotator of the thigh (see Image. Posterior Hip Muscles)
Physiologic Variants
Lumbosacral trunk variants differ in terms of root thickness, arrangement, exit direction with respect to the piriformis muscle, and course.[1][2][4][5] These differences contribute to the unique characteristics of each variant.
Surgical Considerations
Over 95% of lumbar disc herniations affect either the L4/L5 or L5/S1 disc spaces, or both. Patients commonly experience sharp, stabbing low back pain that radiates from the lower lumbar region down to the foot.[6][7][8] Nonsurgical management usually suffices in cases of lower extremity radiculopathy[9][10][11] and acute lumbar disc herniation.[8] The most common indication for surgical intervention is persistent, intractable pain despite at least 6 weeks of optimal conservative treatment.[12]
Clinical Significance
Foot Drop as an Obstetric Complication
Fetal head pressure against the lumbosacral trunk can cause foot drop late in pregnancy or during parturition.[13] The condition presents as foot slapping on the floor while walking. Foot drop can take months to resolve.[14]
Herniated Lumbar Disc
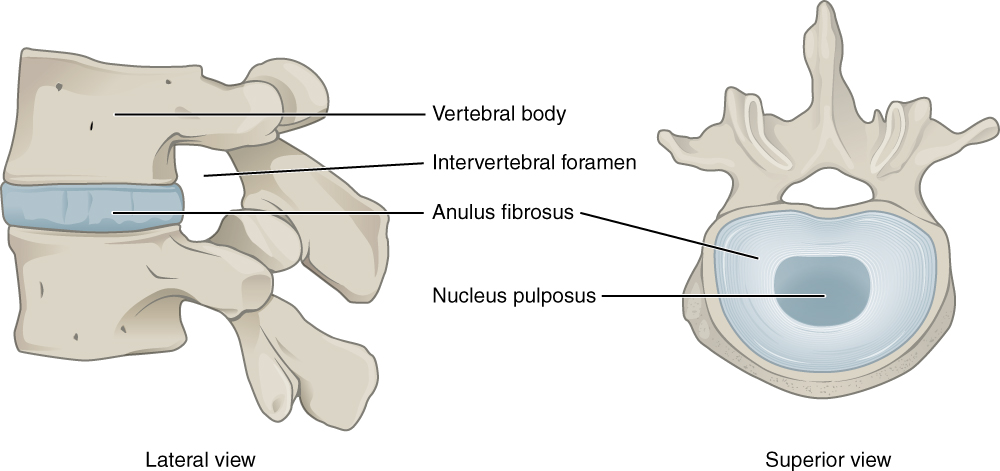
The intervertebral disc is often likened to a jelly-filled doughnut, with the tough annulus fibrosus on the outer portion and the soft nucleus pulposus in the inner portion (see Image. Intervertebral Disc). However, the integrity of the annulus fibrosus diminishes with repeated use, aging, and trauma and can lead to nucleus pulposus herniation.
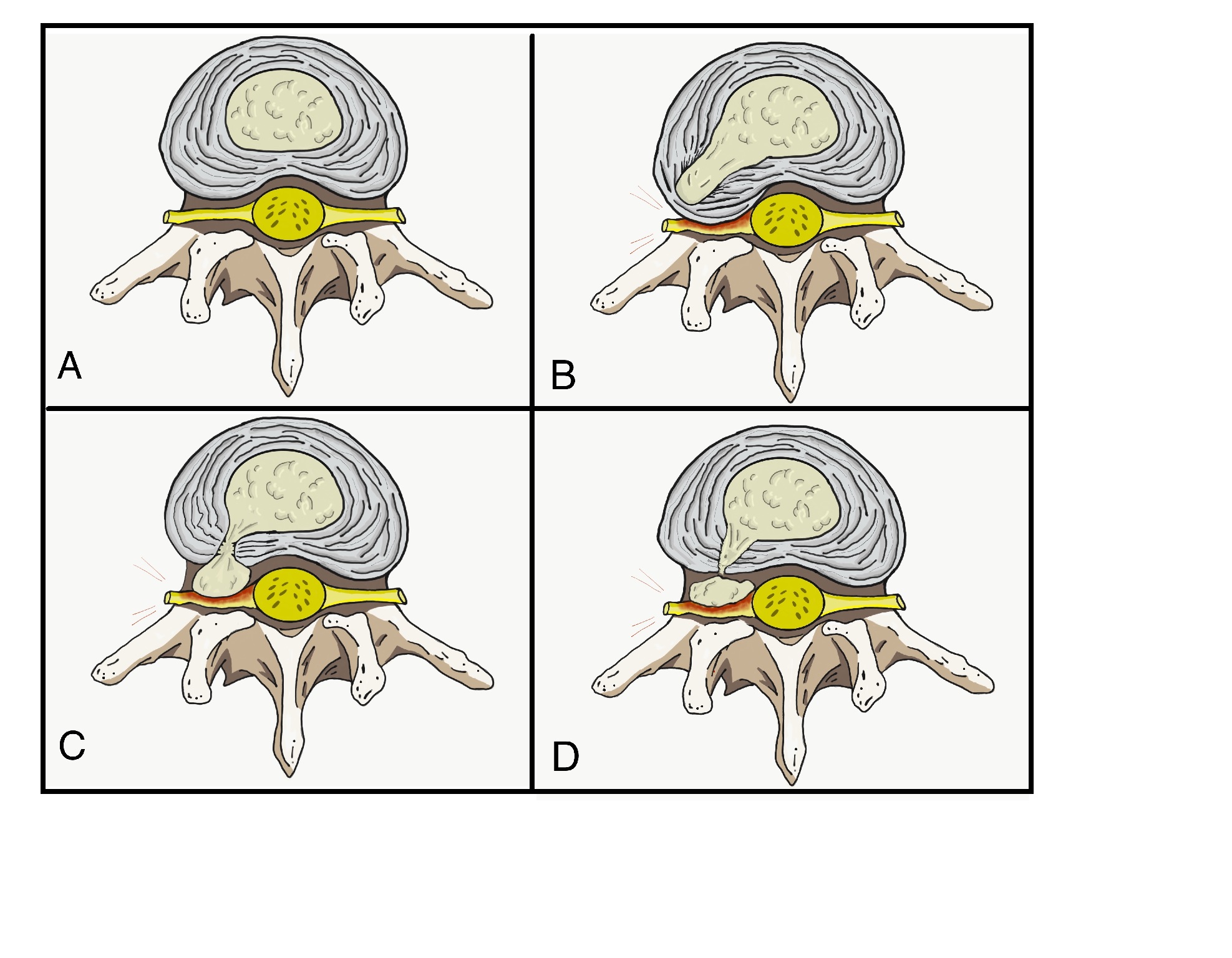
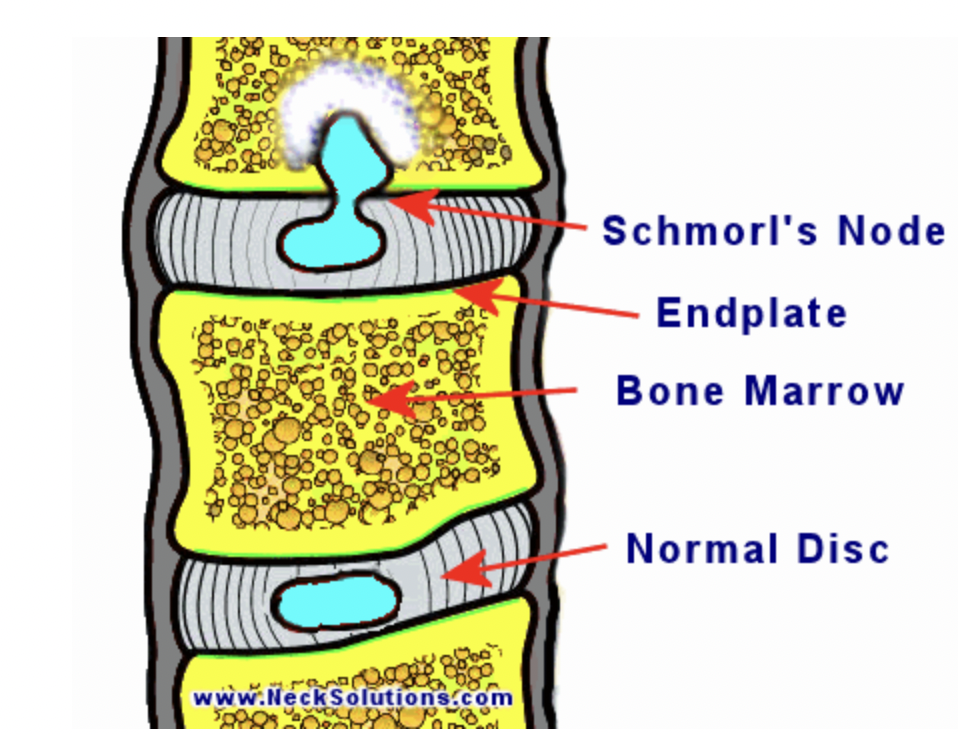
Nucleus pulposus herniation usually occurs lateral to the intervertebral disc, potentially causing nerve root compression (see Image. Stages of Nucleus Pulposus Herniation). Infrequently, a Schmorl nodule may develop when the nucleus pulposus herniates into a vertebra located either superior or inferior to it (see Images. CT, Schmorl Node and Schmorl Node Illustration).
Lower extremity radiculopathy, often ambiguously termed sciatica, is frequently attributable to nerve root compression, especially in the lumbosacral plexus or sciatic nerve. Pain is described as shooting, stabbing, or burning, radiating from the lower back to either lower extremity. Numbness and hypersensitivity may also occur.
The spinal cord usually terminates at the L2 vertebral level and is not commonly affected by lumbar disc herniation. However, nerve root compression superior to the L2 vertebrae can compress the spinal cord and higher spinal roots.
Herniated lumbar intervertebral discs can cause paralumbar muscle spasms from irritation of the meningeal branches of the nerve roots affected. The most involved areas are the following:
- L4/L5 disc, causing L5 dermatome referred pain
- L5/S1 disc, resulting in S1 dermatome referred pain
A dermatome is a cutaneous area innervated by a single nerve root. The L5 nerve root has no associated reflex actions. However, the Achilles tendon reflex is attributed to the S1 nerve root. Therefore, S1 nerve root injuries can weaken or abolish this reflex.
Spastic piriformis syndrome is a differential diagnosis of paralumbar muscle spasms. Trauma or impingement of the sciatic nerve by the piriformis can cause this condition. Paralumbar muscle pain is typically absent, but hip pain radiating to the leg is common. Thus, the condition can mimic lumbar disc herniation. To test for the presence of spastic piriformis syndrome, the examiner instructs the patient to lie prone with the legs flexed at the knee. Failure to abduct the leg from this position confirms the presence of spastic piriformis syndrome.[15]
Diabetes Mellitus
Poorly controlled diabetes mellitus can lead to widespread arterial stenosis, which may occlude the vasa nervorum or the small arteries supplying the peripheral nerves. Diabetic neuropathy is a condition with diverse presentations, as it can affect nerve function at various levels. Treatment is usually multimodal and may include tricyclic antidepressants, although their benefit is controversial. The biggest concern when diabetic neuropathy sets in is the development of skin ulcers in the extremities, which can go undetected due to sensory dysfunction.[16]
Other Pertinent Clinical Conditions
Sacral tumors can also cause lumbosacral plexopathy.[17] Surgery is indicated when mass effects like debilitating pain or neurologic deficits manifest.
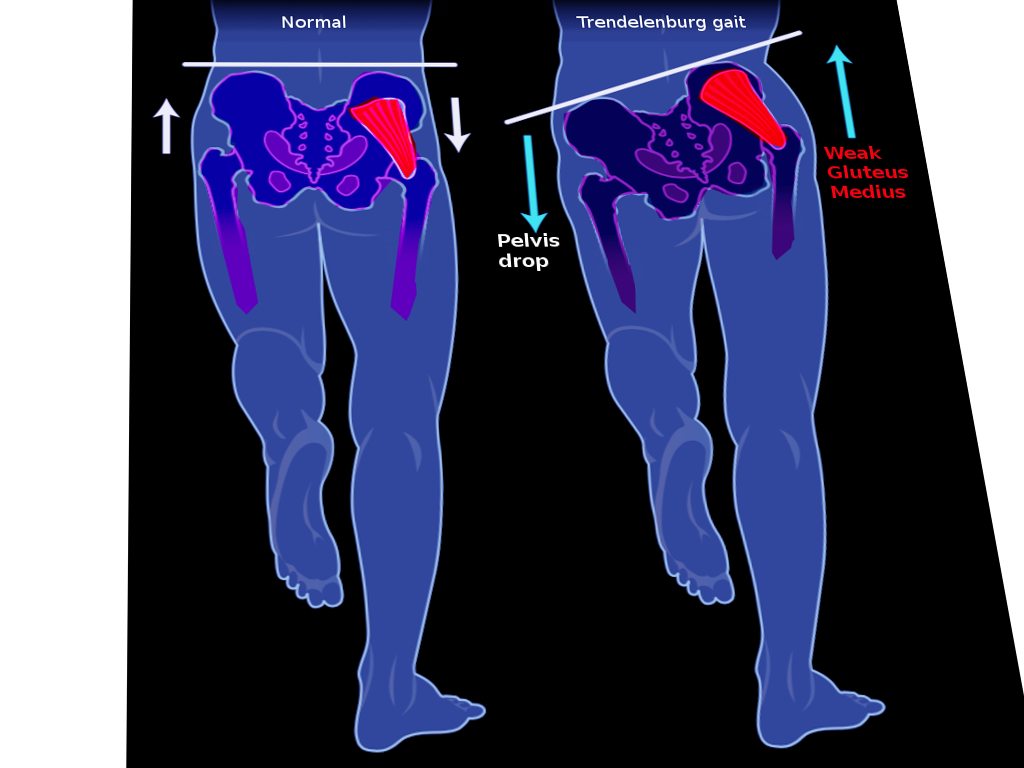
The Trendelenburg gait arises from the weakness of the gluteus medius and gluteus minimus. These muscles normally stabilize the pelvis during the stance phase of the gait cycle. A positive Trendelenburg sign is elicited when the hip falls on the side of the raised leg (see Image. Trendelenburg Gait). Using a cane on the unaffected side improves gait biomechanics. Superior gluteal nerve injury leads to gluteus medius and gluteus minimus dysfunction. Injury to this nerve may be from iatrogenic causes, such as a gluteal needle injection or hip surgery.[2][18][19]