Continuing Education Activity
Low back pain is a pervasive musculoskeletal complaint and one of the prevalent issues encountered in clinical practice. Given its prevalence and impact, the broad spectrum of differential diagnoses for low back pain includes lumbosacral radiculopathy—the leading cause of disability in the developed world for individuals aged 45 and younger. Lumbosacral radiculopathy is characterized by pain resulting from compression or irritation of nerve roots in the lumbosacral region of the spine, along with numbness, weakness, and reflex changes. This condition can manifest without overt lumbar pain, making its recognition crucial for timely intervention. The condition often arises due to degenerative changes such as disc herniation, ligamentum flavum changes, facet hypertrophy, or spondylolisthesis, leading to nerve root compression.
Diagnosis involves a thorough physical examination, including tests such as the Lasègue test, and may require magnetic resonance imaging if symptoms persist despite conservative approaches such as nonsteroidal anti-inflammatory drugs, acetaminophen, and gabapentin. Effective management often necessitates the involvement of an interprofessional healthcare team to enhance patient outcomes. This activity meticulously reviews the pathophysiology, symptomatology, and clinical presentation of lumbosacral radiculopathy, elucidating the diagnosis and differential considerations of the condition. This activity also highlights the essential roles of the interprofessional healthcare team in the comprehensive management of lumbosacral radiculopathy, underscoring the significance of recognizing lumbosacral radiculopathy, even in the absence of overt lumbar pain, to ensure timely intervention. By enhancing patient outcomes and fostering effective collaborative care, clinicians can better address the needs of individuals experiencing this complex pain syndrome.
Objectives:
Identify the key anatomical structures and pathophysiological mechanisms involved in lumbosacral radiculopathy.
Screen patients presenting with low back pain for red-flag symptoms indicative of emergent conditions associated with lumbosacral radiculopathy.
Implement evidence-based conservative management strategies for patients with lumbosacral radiculopathy, including pharmacological and non-pharmacological interventions.
Collaborate with interprofessional healthcare team members to coordinate care transitions and optimize the comprehensive treatment of patients with lumbosacral radiculopathy.
Introduction
Low back pain is among the most prevalent musculoskeletal complaints in clinical practice. Low back pain ranks as one of the primary causes of disability in individuals aged 45 and younger in the developed world, trailing closely behind the common cold as the second most common reason for work absenteeism.[1] Furthermore, low back pain imposes significant annual healthcare costs on society. Although epidemiological studies may vary, the incidence of low back pain is estimated to exceed 5%, with a lifetime prevalence ranging from 60% to 90%.[2] Fortunately, many instances of low back pain are self-limited and are resolved without medical intervention. Roughly half of cases resolve within 1 to 2 weeks, with 90% resolving within 6 to 12 weeks. Given the wide array of potential causes, the broad spectrum of differential diagnoses for low back pain should include consideration of lumbosacral radiculopathy.
Lumbosacral radiculopathy refers to a pain syndrome characterized by the compression or irritation of nerve roots in the lumbosacral region of the spine. This compression often stems from degenerative changes such as disc herniation, ligamentum flavum alterations, facet hypertrophy, and spondylolisthesis, culminating in the compression of one or more lumbosacral nerve roots. Symptoms typically include low back pain radiating into the lower extremities in a dermatomal pattern corresponding to the affected nerve root. Additional symptoms may include numbness, weakness, and loss of reflexes, although the absence of these symptoms does not exclude the diagnosis of lumbosacral radiculopathy.[3]
Etiology
The noxious stimulus of a spinal nerve root creates ectopic nerve signals that are perceived as pain, numbness, and tingling along the nerve distribution, as well as weakness in the nerve root's myotome distribution when severe enough. Lesions of the intervertebral discs and degenerative disease of the spine are the most common causes of lumbosacral radiculopathy. In the degenerative setting, the intervertebral disc undergoes desiccation and fibrosis, then fissuring or tearing, which results in an increased risk of herniation of disc material outside of the normal confines of the disc space. Disc herniations may compress one or more nerve roots, producing lumbosacral radiculopathy. In severe cases with a large disc herniation that compresses multiple nerve roots, patients may present with cauda equina syndrome.[4] In addition to degenerative etiology, any process irritating spinal nerve roots can result in lumbosacral radiculopathy.
Epidemiology
The lifetime prevalence rates of low back pain within the general population range from 60% to 90%, of which 5% to 10% will suffer from radiculopathy.[2][5] The condition constitutes a significant reason for patient referral to neurologists, neurosurgeons, or orthopedic spine surgeons. Low back pain is the second greatest cause of workplace absenteeism after upper respiratory tract infections. About 25 million people miss work due to low back pain, and more than 5 million are disabled from it. Patients with chronic back pain account for a significant proportion of healthcare expenditures.[3] Known risk factors for progressive lumbar degenerative changes include smoking, genetics, and repetitive trauma.[6]
Pathophysiology
Lumbosacral radiculopathy is the clinical term that describes a predictable constellation of symptoms occurring secondary to mechanical or inflammatory cycles compromising at least one of the lumbosacral nerve roots. Patients can present with radiating pain, numbness or tingling, weakness, and gait abnormalities across a spectrum of severity. Depending on the nerve root affected, patients can present with these symptoms in predictable patterns affecting the corresponding dermatome or myotome.[7]
The intervertebral disc experiences desiccation and fibrosis in the degenerative setting, leading to fissuring or tearing. This increases the risk of herniation of disc material beyond the normal confines of the disc space. The posterior longitudinal ligament is the strongest in the midline, and the posterolateral annulus fibrosus may bear a disproportionate portion of the load exerted from the weight above. This may explain why most lumbosacral disc herniations occur posterolaterally within the central canal or lateral recess. Herniated discs may compress one or more nerve roots, producing lumbosacral radiculopathy. In the lumbosacral region, herniated discs characteristically compress the traversing nerve root as they enter the lateral recess before exiting through the neural foramen of the level below. For instance, in the case of an L5-S1 disc herniation, this compression would typically affect the S1 nerve root.
History and Physical
As with any disease process, a comprehensive history and physical examination are essential for diagnosing lumbosacral radiculopathy. Pain is the most commonly reported symptom. However, patients may also experience numbness or weakness along the dermatome/myotome distribution supplied by the affected nerve root. Radicular pain is often described as "electrical shocks" or "shooting pains" that radiate along the course of the nerve root's dermatome. During history-taking, screening for any red-flag symptoms that could indicate an urgent or emergent clinical condition is essential.
Before evaluating a patient, clinicians must first rule out any associated "red-flag" symptoms, as these symptoms could indicate a more severe underlying condition that requires immediate attention. The symptoms include thoracic pain, fever/unexplained weight loss, intravenous drug use, immunosuppression, prolonged use of steroids, night sweats, bowel or bladder dysfunction, and malignancy. In addition, any previous surgeries, chemo/radiation, recent imaging, bloodwork, or history of metastatic disease should be documented. This can be seen in association with pain at night, pain at rest, unexplained weight loss, or night sweats. Significant medical comorbidities, neurologic deficit or serial exam deterioration, gait ataxia, saddle anesthesia, acute onset of urinary retention or overflow incontinence, progressive lower extremity weakness, and age of onset (bimodal; younger than 20 or older than 55) should be considered.
A full neurological examination should be performed, including assessing upper motor neuron findings (eg, Babinski sign, clonus, and spasticity). During physical examination, various maneuvers can aid clinicians in diagnosing lumbosacral radiculopathy. The Lasègue test, or straight leg test, involves passively raising one leg into the air, creating increased tension on the sciatic nerve between 30° to 60° from the exam table. While the crossed straight leg test is less sensitive, it offers greater specificity. A positive sign is noted if the patient's symptoms are reproduced during passive movement between 30° and 60°, suggesting lower lumbar nerve root involvement (L4 to S1). Similarly, the reverse straight leg (Ely) test stretches the femoral nerve and the L2 to L4 nerve roots by extending the hip and flexing the knee with the patient in a prone position. Additionally, radicular symptoms can be provoked by seating the patient with the neck in full flexion and knees in full extension (slump test).[8][9]
In the setting of lumbosacral radiculopathy, diminished deep tendon reflexes can be expected. Specifically, the knee-jerk reflex may be affected for the L4 nerve root, the medial hamstring reflex for the L5 nerve root, and the Achilles reflex for the S1 nerve root. Motor weakness associated with lumbosacral radiculopathy typically affects specific muscle groups—the quadriceps femoris (knee extension) for the L4 nerve root, the tibialis anterior and extensor hallucis longus (dorsiflexion) for the L5 nerve root, and the gastrocnemius (plantarflexion) for the S1 nerve root. Additionally, decreased sensation is often noted along specific dermatomes: the medial malleolus and medial foot for the L4 nerve root, the dorsum of the foot for the L5 nerve root, and the lateral malleolus and lateral foot for the S1 nerve root.
Evaluation
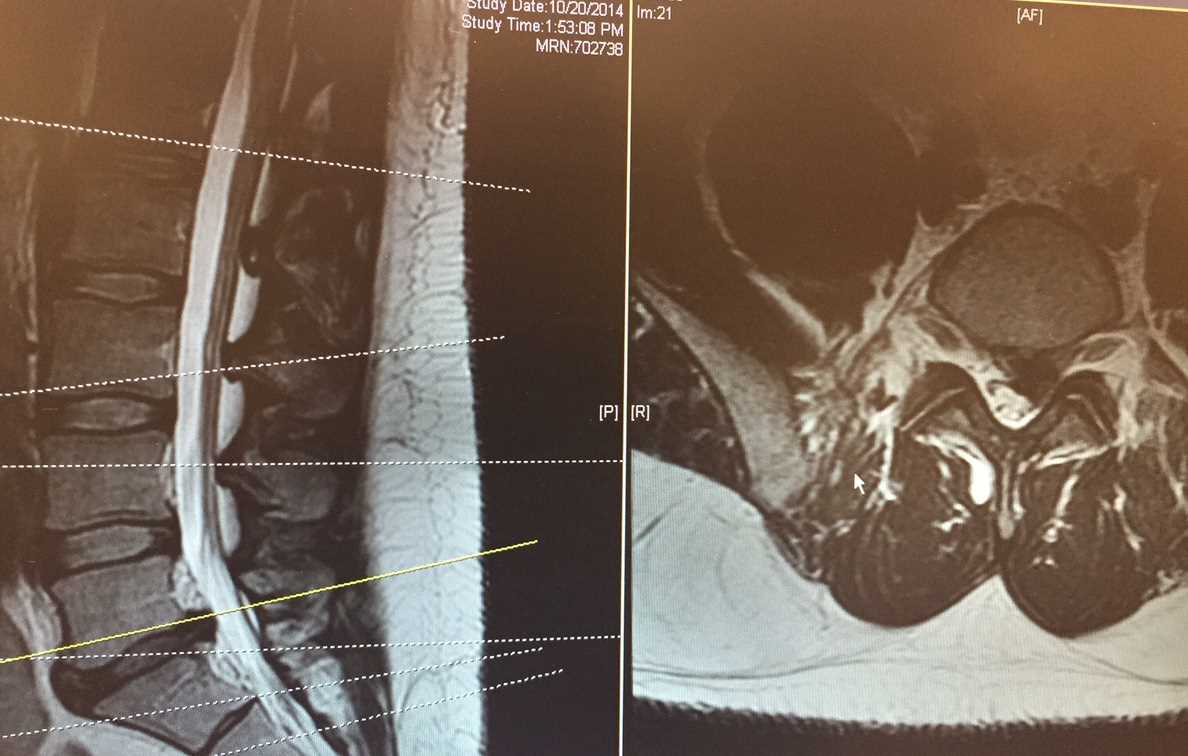
Given the favorable outcome and often spontaneous resolution of the vast majority of low back pain symptoms and lumbosacral radiculopathy, extensive imaging is usually not necessary in patients with symptoms of less than 4 to 6 weeks duration. The diagnostic process should be initiated with a comprehensive physical examination. Neurological deficits, particularly focal weakness, detected during examination warrant further investigation. If symptoms persist beyond 1 to 2 months despite conservative management, magnetic resonance imaging (MRI) without contrast is considered the gold standard for evaluating lumbosacral radiculopathy. In cases where infection needs to be ruled out, MRI with contrast is recommended, especially for patients with a history of previous spinal surgeries (see Image. Lumbar MRI).
A computed tomography (CT) myelogram is an alternative option for patients who cannot undergo MRI. However, CT is not as sensitive in visualizing soft tissue or tumors and is not recommended for routine use. On the other hand, x-rays are simple and readily available in most developed countries. They can reveal gross bony abnormalities such as fractures, spondylolisthesis, disc space narrowing, and other degenerative changes. In cases where radiographic findings do not align with the patient's clinical presentation, electromyography and nerve conduction studies can help localize a lesion with relatively high diagnostic specificity.[10]
Treatment / Management
Treatment varies depending on the etiology and severity of symptoms. Conservative management of symptoms is generally considered the first-line treatment. Medications are used to manage pain symptoms, including nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, anti-epileptic medications that can be used to treat nerve-related pain (eg, gabapentin), and in severe cases, low-dose opiates. Systemic steroids are an option for lumbosacral radiculopathy, which can result in modest benefits.[11]
Nonpharmacological interventions are often utilized as well. Physical therapy, acupuncture, chiropractic manipulation, and traction are all commonly used to treat lumbosacral radiculopathy. Notably, the data supporting the use of these treatment modalities are equivocal. Interventional techniques are also commonly used and include epidural steroid injections and percutaneous disc decompression. In refractory cases, surgical decompression can be performed, in addition to instrumented fusion, if there is concern for instability.[12][13][14]
Differential Diagnosis
The broad spectrum of differential diagnoses for lumbosacral radiculopathy includes, but is not limited to, the following conditions:
- Degenerative conditions of the spine (most common causes):
- Spondylolisthesis: In the degenerative setting, this arises from a pathologic cascade involving intervertebral disc degeneration, subsequent intersegmental instability, and facet joint arthropathy.
- Spinal stenosis
- Adult isthmic spondylolisthesis: Typically caused by an acquired defect in the pars interarticularis. However, the degenerative subtype is more common in adults.
- Pars defects (spondylolysis) in adults are often secondary to repetitive microtrauma.
- Trauma (burst fractures with bony fragment retropulsion):
- Clinicians should recognize that spinal fractures can occur in younger, healthy patient populations secondary to high-velocity injuries, such as motor vehicle accidents and falls from height, as well as in older individuals, particularly those with osteoporosis, where low-velocity injuries or spontaneous fractures may occur.
- Associated bleeding from the injury can result in a deteriorating neurological examination.
- Benign or malignant tumors: They include metastatic tumors, which are most common, and primary tumors, including ependymoma, schwannoma, neurofibroma, lymphoma, lipomas, paraganglioma, ganglioneuroma, osteoblastoma, and multiple myeloma.
- Infections: Infections may manifest as osteodiscitis, osteomyelitis, epidural abscess, fungal infections, or additional conditions such as Lyme disease, HIV/AIDS-defining illnesses, and herpes zoster.[15]
- Vascular conditions: Vascular conditions include hemangioblastoma, vascular claudication, and arteriovenous malformations.[16]
- Inflammatory conditions: Inflammatory conditions may include trochanteric bursitis of the hip.[17]
- Peripheral conditions: Peripheral conditions may encompass neuropathy and piriformis syndrome.[18]
- Congenital conditions: Congenital conditions may involve conjoined nerve roots.
- Acquired conditions: Acquired conditions may include juxtafacet cyst, which can be ganglion or synovial cyst,[19] and arachnoiditis ossificans.[20]
Prognosis
The majority of cases of lumbosacral radiculopathy tend to resolve with conservative management. However, for those necessitating surgical intervention, a study indicated that among 100 patients undergoing discectomy, 73% experienced complete relief of leg pain and 63% had complete relief of back pain at the 1-year follow-up.[21] These numbers remained stable at the 5- to 10-year follow-up, with 62% reporting complete relief in both categories. Notably, only 5% qualified as having failed back syndrome at the 5- to 10-year follow-up.[22]
Complications
Common complications resulting from surgical intervention for lumbosacral radiculopathy include, but are not limited to, superficial wound infection (1% to 5%),[23] increased motor deficit, unintended incidental durotomy, recurrent herniated lumbosacral disc (4% with 10-year follow-up),[24] and postoperative urinary retention.
Deterrence and Patient Education
Lumbosacral radiculopathy refers to a pain syndrome resulting from compression or irritation of nerve roots in the lumbosacral region, commonly characterized by symptoms such as low back pain, leg pain, lower extremity numbness or tingling, and weakness. Typically attributed to degenerative changes, this condition can often be managed conservatively with approaches including medications, non-pharmacological interventions such as physical therapy, and localized pain treatments such as targeted injections.
If symptoms remain refractory to conservative management, further evaluation through radiographic imaging and surgical intervention may be warranted in some instances. If an individual is experiencing symptoms suggestive of lumbosacral radiculopathy, seeking evaluation from a healthcare provider to rule out red-flag symptoms is advisable. Prompt assessment and treatment are essential for conditions associated with these symptoms.
Pearls and Other Issues
Lumbosacral radiculopathy is a prevalent complaint in clinical practice, accounting for numerous annual doctor visits. Although most cases are benign and resolve spontaneously, conservative management is the initial approach for patients lacking clinical red-flag symptoms. However, if symptoms persist despite conservative measures or if weakness or red-flag symptoms are evident, diagnostic tools such as radiographic studies, electromyography, and nerve conduction studies can aid in establishing a diagnosis.[16][7][14]
Enhancing Healthcare Team Outcomes
Lumbosacral radiculopathy is a prevalent issue, and it is crucial for advanced practice providers and physicians working collaboratively to be vigilant about recognizing red-flag symptoms, which necessitates emergent interventions. Timely reporting to the physician and coordinated team management are essential for optimizing patient outcomes.