Continuing Education Activity
This scholarly review elucidates the intricacies of lower extremity nerve blocks, delineating the innervation of the lower limb via the lumbosacral plexus and the specific nerves implicated. The rising predilection for lower extremity nerve blocks as the anesthesia and analgesia modality of choice in ambulatory procedures is underscored, a trend propelled by the evolution of ultrasound-guided methodologies. The review methodically explicates the techniques employed for the blockade of the femoral, obturator, sciatic, and assorted foot nerves, accentuating their clinical pertinence in distinct surgical interventions and postoperative analgesic management. Furthermore, the review broaches the potential adversities concomitant with lower extremity nerve blocks. In culmination, the discourse accentuates the quintessential role of a cohesive interprofessional cadre in safeguarding efficacious and secure patient care during the instigation and oversight of lower extremity nerve blocks.
This scholarly endeavor delineates the methodology and clinical relevance of lower extremity nerve blocks, spotlighting the pivotal role of the interprofessional medical consortium in the assessment and stewardship of patients slated for surgical interventions or necessitating analgesia for the lower limb. The burgeoning adoption of ultrasound-facilitated techniques, heralding enhanced precision and patient outcomes, is emphasized. The discourse delves into the innervation dynamics and functional attributes of various lower limb nerves, offering a comprehensive understanding of the deployment of specific nerve blocks for targeted anesthetic and pain modulation. Moreover, the potential adversities inherent to lower extremity nerve blocks are discussed, with a focus on the imperative of meticulous surveillance and resuscitative protocols. Assimilating and actualizing the tenets delineated in this scholarly endeavor will bolster the interprofessional team's proficiency in delivering secure and efficacious care to patients undergoing lower extremity nerve blocks.
Objectives:
Assess the innervation of the lower extremity with the clinical application of lower extremity nerve blocks.
Identify the steps in the administration of lower extremity nerve blocks.
Determine the potential complications of lower extremity nerve blocks.
Identify the importance of improving care coordination among interprofessional team members to improve outcomes for patients undergoing lower extremity nerve blocks.
Introduction
The lumbosacral plexus, responsible for innervating the lower limb, encompasses the nerve roots from L1 to S4. Distinct from the brachial plexus, it cannot be effectively blocked using a singular injection method. Historically, neuraxial blocks were the method of choice for achieving anesthesia or analgesia in the lower extremities. However, with the rise of outpatient procedures due to technological advancements, the appeal of neuraxial techniques has diminished.[1][2][3][4][5][6] Concurrently, the advent of ultrasound-guided methods has enhanced the precision of nerve identification and the efficacy of nerve blocks in the lower extremities. While multiple injections are typically necessary for comprehensive lower extremity anesthesia, it remains a favorable choice for outpatient scenarios. The utilization of lower extremity nerve blocks has expanded, especially in contexts necessitating lower limb anesthesia or analgesia.
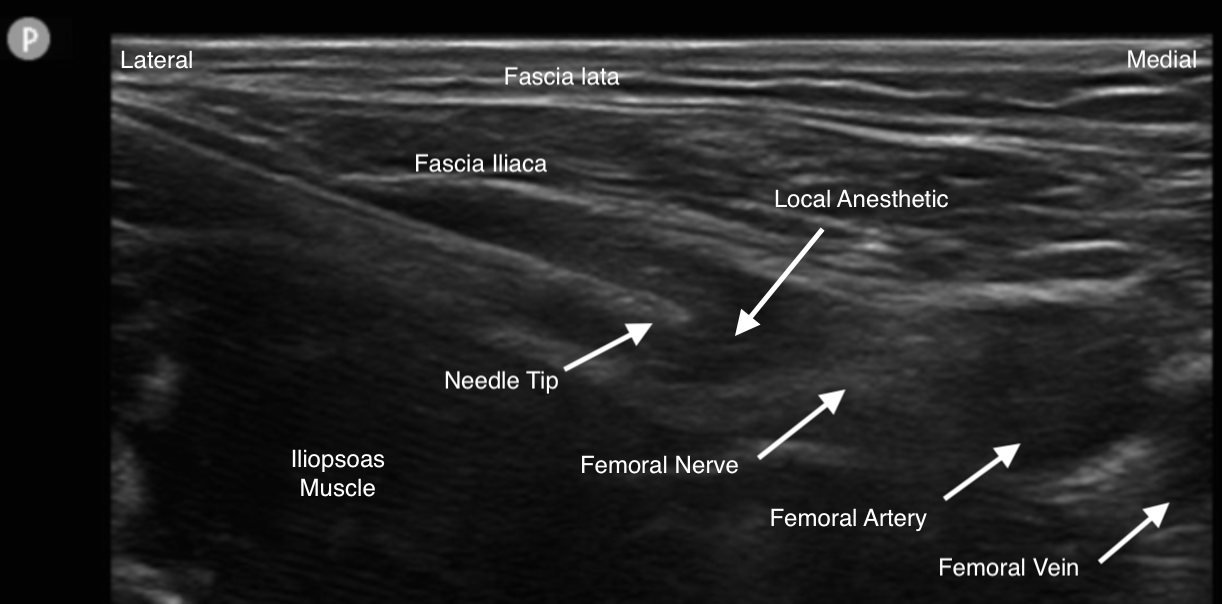
Peripheral nerve blocks are pivotal in postoperative pain management in orthopedic surgeries, forming an integral component of multimodal analgesia. The femoral nerve block (FNB) was pioneered in 1952, and subsequent advancements, especially in ultrasound-guided techniques, have transformed the application of PNBs in upper limb procedures (see Image. Femoral Nerve Block). By circumventing general anesthesia, PNBs present surgical teams with an opportunity to reduce associated risks. Initially, PNBs for the lower extremities were not extensively adopted due to the dominance of neuraxial anesthesia. Neuraxial blocks were perceived as more straightforward, requiring a single injection via bony landmarks. In contrast, PNBs for the lower extremities demanded a profound understanding of the lumbosacral plexus and the blockage of multiple nerves at varying depths.
Nevertheless, recent advancements in ultrasonography have facilitated precise block placements, reigniting interest in PNBs. This resurgence is motivated by endeavors to address the opioid crisis and escalating healthcare expenditures. The opioid epidemic remains a pressing concern in the U.S., urging orthopedic surgeons to take proactive measures. PNBs have demonstrated their potential in reducing postoperative opioid requirements and have been extensively studied in the context of hip and knee surgeries, encompassing arthroscopy, trauma, and arthroplasty. A meta-analysis of knee surgery trials revealed that multi-nerve blockade, especially the combined FNB and sciatic nerve block (SNB), produced optimal outcomes in pain alleviation, reduced opioid consumption, and enhanced range of motion. Although evidence supporting routine nerve blockade in arthroscopic hip surgeries is limited, potential benefits include diminished pain, reduced morphine dosages, and decreased hospitalization rates. Enhanced analgesia via PNBs augments patient satisfaction, promotes cost-effectiveness, accelerates recovery, and facilitates outpatient procedures while reducing complications.
Anatomy and Physiology
The lumbosacral plexus divides into the femoral, lateral femoral cutaneous, obturator, and sciatic nerves that innervate the entire lower extremity. The femoral nerve provides sensation and motor function to the anterior thigh. The femoral nerve continues as the saphenous nerve, providing sensation to the ipsilateral medial leg and foot and a portion of the ipsilateral great toe. The LFCN supplies sensation to the lateral thigh. The sensory component of the obturator nerve supplies the medial thigh; the motor component supplies the thigh adductors.
Neither the lateral femoral cutaneous nor the obturator nerve have any sensory or motor input to the leg distal to the knee. The sciatic nerve runs with the posterior cutaneous nerve of the thigh and provides sensory and motor innervation to the posterior thigh. The sciatic nerve continues posteriorly and divides into the tibial and common peroneal nerves, just cephalad to the popliteal fossa, and provides sensory and motor innervation to the anterior, lateral, and posterior lower leg.
Five nerves provide sensory and motor to the foot. The saphenous nerve supplies sensation to the medial foot and a portion of the great toe. The deep peroneal nerve supplies the web space between the great and second toes. The superficial peroneal nerve supplies most of the dorsum of the foot and toes, while the sural nerve supplies the lateral foot and a portion of the fifth toe. The posterior tibial nerve divides into the medial and lateral plantar nerves and supplies the sole and plantar surface of the toes.
Indications
Lower extremity blocks are useful in providing targeted anesthesia to the hip, knee, ankle, or foot, particularly in patients for whom general or neuraxial anesthesia is contraindicated.[7][8] Furthermore, lower extremity blocks are frequently utilized postoperatively to improve pain control and lower the acute postoperative opioid burden. Another benefit of lower extremity nerve blocks is the added effect of restoring mobility to patients who may otherwise be limited by pain in the early postoperative period. This early mobilization is important in minimizing complications such as venous thromboembolism and bedsores and promotes early progress in physical therapy.[9][10][11]
Lower extremity peripheral nerve blocks can be used as the primary anesthetic or adjuncts to general or neuraxial anesthesia. They provide effective analgesia and have minimized adverse effects such as motor blockade.[12] Some common lower extremity nerve blocks include the FNB, fascia iliaca block, SNB, saphenous nerve block, adductor canal block, iPACK block, ankle block, and LPB.
The FNB is commonly used for surgeries involving the anterior aspect of the thigh and the medial aspect of the leg below the knee. The FNB provides analgesia for knee surgery and has been shown to reduce pain and improve patient outcomes. However, it can cause quadriceps weakness, increasing the risk of falls.
The fascia iliaca block targets the femoral nerve and LFCN. This block is used for hip surgeries and provides rapid analgesic benefits. The fascia iliaca block is performed by injecting local anesthetic under the fascia iliaca.
The SNB is indicated for foot, ankle, and posterior knee surgeries. The SNB can be performed through various approaches, such as the anterior, transgluteal, subgluteal, or popliteal block. This block provides broad lower extremity coverage but may result in motor blockade.
The saphenous nerve block is used for surgeries involving the medial aspect of the knee, foot, and ankle. The saphenous nerve block can be performed through different approaches, such as the femoral triangle, medial femoral condyle, or tibial tuberosity. This block provides sensory anesthesia but does not cover the posterior capsule of the knee.
The adductor canal block targets the saphenous nerve and nerve to the vastus medialis. This block is used for surgeries involving the medial aspect of the knee, foot, and ankle. Compared to the FNB, it offers motor-sparing effects and allows for early mobilization.
The iPACK block provides analgesia to the posterior knee capsule and is used as an adjunct to the adductor canal block. This block improves pain relief, reduces opioid requirements, and promotes early ambulation.
The ankle block is used for foot surgeries and provides anesthesia to the foot using surface landmarks. The ankle block effectively relieves pain and does not require ultrasound guidance.
The LPB is indicated for hip surgeries and blocks the femoral, obturator, and LFCNs. The LPB can be performed using ultrasound guidance but has seen decreased use due to alternative regional anesthesia techniques such as the fascia iliaca block.
While these blocks have proven efficacy, they also carry potential complications such as bleeding, infection, nerve damage, and motor weakness. Careful patient selection and technique are essential to minimize these risks.[13][14]
Contraindications
Complications of lower extremity nerve blocks are few.[15][16] Lower extremity nerve blocks should not be performed under the following conditions:
- Hypercoagulable state: Lower extremity nerve blocks may blind practitioners to the early signs and symptoms of a deep venous thrombosis in patients at high risk for venous thromboembolism.
- Thrombocytopenia or anticoagulation may predispose to bleeding at the injection site and subsequent complications.
- Preexisting skin infections at the injection site frequently result in seeding the lower extremity or nerve, predisposing to deep infection.
- Patients with a demonstrated drug allergy to the anesthetic agent of choice should not undergo a lower extremity block due to the risk of anaphylaxis or other allergic responses.
Equipment
The equipment used in lower extremity nerve blocks includes:
- Povidone iodine solution or chlorhexidine
- Sterile towels and gauze
- Sterile gloves
- Sterile gown for catheter placement only
- Pre-injection aspiration control syringe
- Needles: 18 or 20 G for drawing up the local anesthetic; 25 G for injection
- Local anesthetic with epinephrine or other additives such as dexamethasone or dexmedetomidine
Personnel
A lower extremity nerve block is a minor procedure with the potential to cause significant complications. Thus, the procedure should be performed in a designated area with standard American Society of Anesthesiologists monitors, intravenous access, and resuscitation drugs and equipment immediately available, including intralipid.
Technique or Treatment
Depending on the extent of anesthesia required for the procedure, the lower extremity can be anesthetized by blocking the nerves in combination or individually. The branches of the lumbar plexus plus the sciatic nerve must be blocked to give total anesthesia coverage of the lower extremity.
The lumbar plexus block (LPB), also known as the psoas compartment block, targets multiple nerves, including the iliohypogastric nerve, ilioinguinal nerve, genitofemoral nerve, lateral femoral cutaneous nerve (LFCN), femoral nerve, and obturator nerve. The injection site for LPB is 1 cm cephalad to the intercristal line, penetrating several layers of fascia and muscles to reach the lumbar plexus. Ultrasound and peripheral nerve stimulation are commonly used for guidance during LPB. LPB has been found to provide reliable blockade of the obturator nerve and is favored for its higher success rate compared to the anterior approach of the 3-in-1 block. LPB has shown efficacy in reducing pain after arthroscopic hip surgery but risks complications such as postoperative falls, total spinal anesthesia, hematomas, and systemic toxicity.
The 3-in-1 block, the anterior approach to the LPB, targets the femoral nerve, LFCN, and obturator nerve. This block is performed by injecting anesthetic immediately distal to the inguinal ligament around the femoral nerve. The block requires a significant volume of local anesthetic and pressure to ensure adequate spread to all 3 nerve trunks. Ultrasound guidance has been shown to improve the efficacy of the 3-in-1 block. Limited evidence suggests that the block effectively relieves pain in hip surgery, particularly in cases of trauma and arthroplasty.[17]
The femoral nerve can be blocked either deep to the fascia iliaca compartment, located caudad and medial to the anterior superior iliac spine, or at the femoral crease. The fascia iliaca is a continuous band of fascia in this region, so local anesthetic injected under this fascia reliably produces a block of the femoral and LFCNs. Anatomic landmarks, nerve stimulation, and ultrasound-guided techniques have been described. The more caudad the block is performed, the less reliably the obturator nerve is blocked. The optimal needle placement for this block is just below the inguinal ligament, approximately 2 cm lateral to the femoral artery. This location provides better needle-nerve contact and easier targeting of the larger femoral nerve. Peripheral nerve stimulation and ultrasound guidance are commonly used during the procedure, with ultrasound guidance being the preferred modality when the nerve is well visualized.
The efficacy of FNB in arthroscopic hip surgery has been demonstrated in several studies. Patients who received the block experienced less time in the post-anesthesia care unit, reduced postoperative nausea, and higher patient-reported satisfaction than those who received intravenous narcotics. The block also resulted in lower pain scores and decreased opioid consumption intraoperatively and postoperatively. However, reports of increased postoperative falls and peripheral neuritis have been associated with FNB.[18]
FNB has shown superior analgesia in knee surgery compared to intra-articular local anesthetic infiltration after anterior cruciate ligament (ACL) surgery. FNB has also been effective in providing pain relief after tibial osteotomy and meniscectomy. The block can prolong motor blockade when added to spinal anesthesia but does not affect the time to ambulate under general anesthesia. Complications associated with the block include decreased quadriceps strength, inadvertent intraneural injections, and neuropathy.
Fascia iliaca compartment block (FICB), also known as the fascia iliaca block, targets the femoral nerve and LFCN. The injection site is immediately below the inguinal ligament, two-thirds lateral to a line drawn between the pubic tubercle and the ASIS. FICB can be performed using the "feel" or ultrasound-guided technique. Studies have shown that FICB provides effective pain relief and improved patient satisfaction in arthroscopic hip surgery. Complications associated with FICB include local hematomas, neuropathy, and an increased risk of falls.[19]
The LFCN block focuses on the nerve that arises from the lumbar plexus and runs laterally along the psoas muscle to the anterior superior iliac spine, providing sensation to the proximal two-thirds of the anterolateral thigh. LFCN is useful in treating conditions like meralgia paresthetica and determining the source of anterior upper thigh pain. To perform an LFCN block, the needle is advanced from a point 2 cm medial and 2 cm caudal to the anterior superior iliac spine toward the midline at a 30- to 45-degree angle, reaching a depth of approximately 1 cm.[20]
The pericapsular nerve group (PENG) block is an innovative regional anesthesia technique that provides analgesia during hip surgical interventions. This block targets the articular branches of the femoral, obturator, and accessory obturator nerves, which innervate the anterior hip capsule. Utilizing a high-frequency linear ultrasound probe, the probe is placed in a transverse orientation over the inguinal crease, slightly medial to the ASIS. The iliopsoas muscle and the femoral artery are visualized. A long, echogenic needle is introduced using an in-plane technique from lateral to medial. The needle is advanced anterior to the iliopsoas muscle, aiming for the space between the iliopubic eminence and the anterior inferior iliac spine[21].
The saphenous nerve can be blocked at the mid-shaft femur in the adductor canal or with a field block at the tibial plateau. Saphenous nerve blocks have gained popularity because while sensation is blocked, motor function is spared, an ideal situation for physical therapy and rehabilitation.
The adductor canal block (ACB) is a regional anesthesia technique primarily utilized to provide postoperative analgesia for surgeries involving the anteromedial aspect of the knee and the medial lower leg. The ACB preserves quadriceps muscle strength, making it advantageous for ambulatory surgeries and early postoperative mobilization. The patient is placed in a supine position with the leg slightly externally rotated. This exposes the medial aspect of the thigh, facilitating access to the adductor canal. Using palpation, identify and mark the femoral artery in the mid-thigh region. A high-frequency linear ultrasound probe is placed in a transverse orientation over the mid-thigh region, proximal to the knee joint. The femoral artery, sartorius muscle, and vastus medialis muscle are visualized. The adductor canal is located deep in the sartorius muscle and superficial to the vastus medialis muscle. Under real-time ultrasound guidance, a sterile, echogenic needle is introduced using an in-plane technique from the anterolateral to anteromedial direction. The needle is advanced towards the saphenous nerve, typically located lateral to the femoral artery within the adductor canal.[22]
A proximal SNB, designed to provide analgesia to the lower leg, foot, and ankle, can be achieved via several approaches. These include blocking the nerve in the thigh using either a posterior or anterior approach. The classical method, often called the Labat approach, involves blocking the sciatic nerve in the gluteal region between the greater trochanter and ischial tuberosity, deep to the gluteus muscles and superficial to the quadratus femoris. Meanwhile, the anterior approach targets the nerve as it moves through the thigh adductors. It provides analgesia to the knee and lateral femur but does not provide sensory anesthesia to the posterior thigh. Both of these approaches can utilize anatomic landmarks, nerve stimulation, and ultrasound-guided techniques, but ultrasound-guided techniques are more commonly used because of direct visualization of the nerve. Complications associated with the proximal approach to the SNB include severe pain, hematomas, temporary neuropathy, and rectal perforation during placement[23].
The distal SNB, more commonly referred to as the popliteal sciatic nerve block, administers the injection of local anesthetic about 6 cm above the popliteal fossa before the nerve divides into the tibial and common peroneal branches. This technique is especially advantageous for surgeries involving the lower extremity below the knee. For a successful PSNB, the patient is usually placed prone, with the leg to be treated slightly flexed to expose the popliteal fossa. After identifying crucial bony landmarks, a high-frequency linear ultrasound probe is positioned transversely in the popliteal fossa, revealing the sciatic nerve between the biceps femoris and semimembranosus muscles. With ongoing ultrasound guidance, an echogenic needle is introduced, either from the lateral or medial side, based on the patient's anatomy and the practitioner's preference. It is then directed toward the sciatic nerve. Possible complications with the PSNB include severe pain, hematomas, and temporary neuropathy.[24][25]
The interspace between the popliteal artery and the capsule of the posterior knee (iPACK) block is an emerging regional anesthesia technique. Designed to target pain in the posterior knee, it addresses discomfort from the joint capsule and structures innervated by the terminal branches of the tibial and obturator nerves. Particularly useful in total knee arthroplasty, it fills gaps left by other regional anesthesia methods. For the procedure, patients are typically positioned either supine or in a lateral decubitus stance, with the relevant leg slightly bent to access the popliteal fossa. A high-frequency linear ultrasound probe is placed transversely in the popliteal fossa. The popliteal artery is visualized, and the posterior joint capsule is identified deep to the artery. Under continuous ultrasound guidance, a sterile, echogenic needle is introduced using an in-plane technique from the lateral side of the probe. The needle is advanced toward the target interspace between the popliteal artery and the posterior joint capsule.[26]
The ankle block provides complete anesthesia of the foot with 5 injections around the ankle. The saphenous nerve, a terminal branch of the femoral nerve that provides sensation to the medial foot, is blocked anterior to the medial malleolus. The saphenous nerve is blocked by inserting a needle subcutaneously proximal and anterior to the medial malleolus and advancing the needle posteromedially at a 45-degree angle to deposit a local anesthetic track.
The deep peroneal nerve, originating from the common peroneal nerve, transverses the anterior compartment of the leg and ends in the first web space. The deep peroneal nerve is blocked by inserting a needle, perpendicular to the tibia, between the extensor hallucis longus and extensor digitorum longus tendons. The needle is advanced until the tibia is contacted, then slightly retracted, and local anesthetic is injected. The superficial peroneal nerve, another branch of the common peroneal nerve, gives sensation to the dorsal medial portion of the foot. This nerve is blocked by advancing the needle in the subcutaneous space anterior to the lateral malleolus at a 10- to 15-degree angle. Once at the level of the lateral malleolus, the needle is slightly retracted, and local anesthetic is deposited.
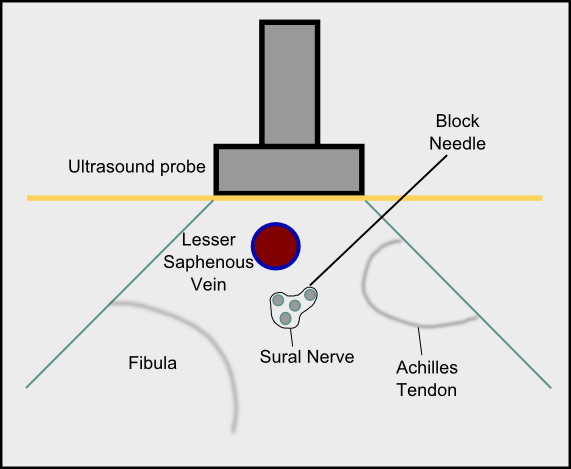
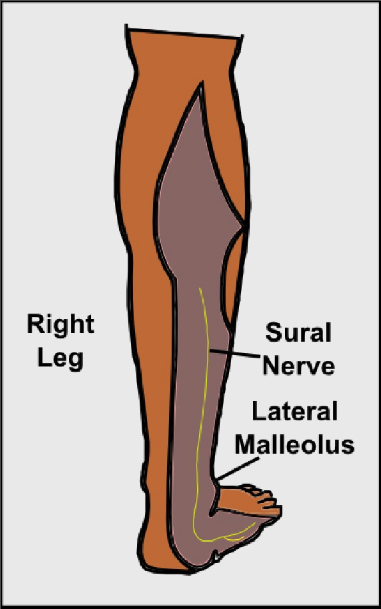
The sural nerve, a branch of the tibial nerve, courses superficially to the gastrocnemius and posterior to the lateral malleolus and gives sensation to the lateral plantar and dorsal surfaces of the foot. The sural nerve is blocked by advancing the needle perpendicular to the long axis of the Achilles tendon, just above the distal tip of the lateral malleolus, and the anesthetic is injected in a track between the fibula and Achilles tendon (see Image. Sural Nerve Block In-Plane Technique).
Lastly, the posterior tibial nerve, derived from the tibial nerve, gives most of the sensation to the plantar surface of the foot. This nerve is blocked posterior to the medial malleolus by inserting a needle in the subcutaneous tissue, directing the needle toward the posteromedial tibia at a 45-degree angle, and depositing a local anesthetic track. Ultrasound guidance may enhance the ankle block by visualizing the local anesthetic spread around the individual nerves.[27]
Complications
Local Complications from the Injection
- Hematoma
- Infection
- Injury to the nerve
- Anesthetic blockade of adjacent structures
- Block failure
Local Anesthetic Systemic Toxicity
- Dizziness, lightheadedness
- Blurred vision
- Ringing, buzzing in ears
- Metal taste in the mouth
- Numbness/tingling around mouth, fingers, or toes
- Drowsiness or confusion
- Seizures and cardiac arrest
Clinical Significance
If successful, most lower extremity nerve blocks last 6 to 24 hours; the duration of anesthesia or analgesia may be shorter.[28] Other options for lower extremity anesthesia and analgesia include spinal and epidural anesthesia.
Recent evidence suggests lower extremity nerve blocks offer compelling advantages over general anesthesia, particularly for lower-extremity surgical procedures. In addition, recent discussions of using these techniques in the clinical context highlight the potential benefits of nerve blocks, including reduced pain, faster recovery times, and fewer systemic side effects associated with general anesthesia.[29]
Two recent systematic reviews and meta-analyses offer compelling evidence supporting the use of nerve blocks over general anesthesia for lower extremity surgical procedures. First, a systematic review and meta-analysis examined general versus regional anesthesia outcomes for lower extremity amputations. The authors found that patients receiving regional anesthesia had better outcomes, fewer complications, and improved pain management than those under general anesthesia. This suggests nerve blocks may be superior for lower extremity amputations.[1]
A similar review focuses on neuraxial or regional anesthesia versus general anesthesia for lower limb revascularization surgery. The authors found that patients receiving regional anesthesia had improved outcomes and fewer postoperative complications. This finding strengthens the argument for using nerve blocks in lower limb surgery.[14]
These studies underline nerve block potential benefits in lower extremity surgery. Compared with general anesthesia, nerve blocks reduce the risk of postoperative complications, improve pain management, and accelerate recovery. However, while the current evidence strongly supports using nerve blocks, it is crucial to consider each patient's circumstances, including their comorbidities, surgical risk, and personal preference. Moreover, the administration of nerve blocks requires specialized training and expertise. It is, therefore, crucial to ensure that healthcare providers are adequately trained in these techniques to maximize their benefits and minimize potential risks.
Enhancing Healthcare Team Outcomes
Anesthesiologists usually perform lower extremity nerve blocks, but a nurse must be dedicated to patient monitoring. Resuscitative equipment must be in the room where the procedure is being performed. Complications, though rare, can potentially cause cardiac or respiratory arrest, bleeding, and nerve damage. An interprofessional team approach will provide the safest and best results for the patient.
Skills
Knowing how to manage anesthesia in patients with lower extremity blocks is essential. Recognition, treatment, and prevention of perioperative adverse events associated with lower extremity blocks is an important strategy. Therefore, management of lower extremity nerve blocks crosses over the breadth and depth of healthcare situations and settings in the perioperative environment.
Strategy
Maintaining continuous closed-loop communication between all members of the perioperative care team regarding the need, technique, and potential management issues associated with lower extremity blocks is most appropriate and ideal. Collaboration, interdisciplinary, interprofessional teamwork, and a culture of integrity and quality improvement are essential to a successful strategy.
Ethics
Obtaining comprehensive informed consent from either the patient or, in the case of patients without the capacity to consent, their designated and authorized decision-maker is necessary before administering a lower extremity nerve block. All team members should feel empowered to state any concerns regarding the process, as this provides additional layers of review and insight into any problematic matters as soon as possible.
Responsibilities
All team members must communicate their concerns, responsibilities, and activities with all other team members contemporaneously and as indicated throughout the perioperative period, based on their professional discretion. All team members are responsible for maintaining professional interactions with, respecting different opinions, and engaging in shared decision-making with all involved stakeholders.
Interprofessional Communication
All team members should respect the free flow of information and concerns among team members without allowing or producing an environment of hostility. Monitoring must be diligent and consistent between and among team members. Maintain clear and closed-loop professional communication among all team members.
Care Coordination
All interprofessional team members should consider it their duty to neither disrupt the work done by other team members nor to, through their actions or inaction, create additional issues or increase the workload for other team members.
In conclusion, the evidence from the referenced studies suggests that nerve blocks hold significant clinical value in managing pain and improving outcomes in lower extremity surgeries. Their use over general anesthesia may enhance patient comfort, reduce systemic adverse effects, and have faster recovery times. However, these benefits must be balanced against the patient's circumstances and the clinician's expertise in administering these techniques. Future research should further delineate the benefits and risks of nerve blocks in different patient populations and surgical contexts to optimize their use in clinical practice.