[1]
Kallini JR, Jain SK, Khachemoune A. Lentigo maligna: review of salient characteristics and management. American journal of clinical dermatology. 2013 Dec:14(6):473-80. doi: 10.1007/s40257-013-0044-6. Epub
[PubMed PMID: 24019181]
[2]
Cohen LM. Lentigo maligna and lentigo maligna melanoma. Journal of the American Academy of Dermatology. 1995 Dec:33(6):923-36; quiz 937-40
[PubMed PMID: 7490362]
[3]
Silvers DN. Focus on melanoma: the therapeutic dilemma of lentigo maligna (Hutchinson's freckle). The Journal of dermatologic surgery. 1976 Sep:2(4):301-3
[PubMed PMID: 1026731]
[4]
Dubow BE, Ackerman AB. Ideas in pathology. Malignant melanoma in situ: the evolution of a concept. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc. 1990 Nov:3(6):734-44
[PubMed PMID: 2263599]
[5]
DeWane ME, Kelsey A, Oliviero M, Rabinovitz H, Grant-Kels JM. Melanoma on chronically sun-damaged skin: Lentigo maligna and desmoplastic melanoma. Journal of the American Academy of Dermatology. 2019 Sep:81(3):823-833. doi: 10.1016/j.jaad.2019.03.066. Epub 2019 Mar 28
[PubMed PMID: 30930085]
[6]
Newell GR, Sider JG, Bergfelt L, Kripke ML. Incidence of cutaneous melanoma in the United States by histology with special reference to the face. Cancer research. 1988 Sep 1:48(17):5036-41
[PubMed PMID: 3409232]
[7]
Elwood JM, Gallagher RP, Worth AJ, Wood WS, Pearson JC. Etiological differences between subtypes of cutaneous malignant melanoma: Western Canada Melanoma Study. Journal of the National Cancer Institute. 1987 Jan:78(1):37-44
[PubMed PMID: 3467128]
[8]
Elwood JM, Hislop TG. Solar radiation in the etiology of cutaneous malignant melanoma in Caucasians. National Cancer Institute monograph. 1982:62():167-71
[PubMed PMID: 7167183]
[9]
Holman CD, Armstrong BK. Cutaneous malignant melanoma and indicators of total accumulated exposure to the sun: an analysis separating histogenetic types. Journal of the National Cancer Institute. 1984 Jul:73(1):75-82
[PubMed PMID: 6588237]
[10]
Holman CD, Armstrong BK, Heenan PJ. A theory of the etiology and pathogenesis of human cutaneous malignant melanoma. Journal of the National Cancer Institute. 1983 Oct:71(4):651-6
[PubMed PMID: 6578359]
[11]
Koh HK, Kligler BE, Lew RA. Sunlight and cutaneous malignant melanoma: evidence for and against causation. Photochemistry and photobiology. 1990 Jun:51(6):765-79
[PubMed PMID: 2195564]
[12]
Schreiber MM, Moon TE, Bozzo PD. Chronic solar ultraviolet damage associated with malignant melanoma of the skin. Journal of the American Academy of Dermatology. 1984 May:10(5 Pt 1):755-9
[PubMed PMID: 6725671]
[13]
Armstrong BK. Epidemiology of malignant melanoma: intermittent or total accumulated exposure to the sun? The Journal of dermatologic surgery and oncology. 1988 Aug:14(8):835-49
[PubMed PMID: 3397443]
[14]
Cox NH, Aitchison TC, Sirel JM, MacKie RM. Comparison between lentigo maligna melanoma and other histogenetic types of malignant melanoma of the head and neck. Scottish Melanoma Group. British journal of cancer. 1996 Apr:73(7):940-4
[PubMed PMID: 8611411]
[15]
McGovern VJ, Shaw HM, Milton GW, Farago GA. Is malignant melanoma arising in a Hutchinson's melanotic freckle a separate disease entity? Histopathology. 1980 May:4(3):235-42
[PubMed PMID: 7390408]
[16]
Holman CD, Mulroney CD, Armstrong BK. Epidemiology of pre-invasive and invasive malignant melanoma in Western Australia. International journal of cancer. 1980 Mar 15:25(3):317-23
[PubMed PMID: 7390655]
[17]
Osterlind A, Tucker MA, Stone BJ, Jensen OM. The Danish case-control study of cutaneous malignant melanoma. IV. No association with nutritional factors, alcohol, smoking or hair dyes. International journal of cancer. 1988 Dec 15:42(6):825-8
[PubMed PMID: 3192325]
Level 2 (mid-level) evidence
[18]
Swetter SM, Boldrick JC, Jung SY, Egbert BM, Harvell JD. Increasing incidence of lentigo maligna melanoma subtypes: northern California and national trends 1990-2000. The Journal of investigative dermatology. 2005 Oct:125(4):685-91
[PubMed PMID: 16185266]
[19]
Lemish WM, Heenan PJ, Holman CD, Armstrong BK. Survival from preinvasive and invasive malignant melanoma in Western Australia. Cancer. 1983 Aug 1:52(3):580-5
[PubMed PMID: 6861096]
[20]
Gassenmaier M, Keim U, Leiter U, Eigentler TK, Röcken M, Gesierich A, Moritz RKC, Heinzerling L, Tüting T, Wollina U, Garbe C. Age as key factor for pattern, timing, and extent of distant metastasis in patients with cutaneous melanoma: A study of the German Central Malignant Melanoma Registry. Journal of the American Academy of Dermatology. 2019 May:80(5):1299-1307.e7. doi: 10.1016/j.jaad.2019.01.044. Epub 2019 Jan 29
[PubMed PMID: 30703453]
[21]
Cox NH, Aitchison TC, MacKie RM. Extrafacial lentigo maligna melanoma: analysis of 71 cases and comparison with lentigo maligna melanoma of the head and neck. The British journal of dermatology. 1998 Sep:139(3):439-43
[PubMed PMID: 9767288]
Level 3 (low-level) evidence
[22]
Mirzoyev SA, Knudson RM, Reed KB, Hou JL, Lohse CM, Frohm ML, Brewer JD, Otley CC, Roenigk RK. Incidence of lentigo maligna in Olmsted County, Minnesota, 1970 to 2007. Journal of the American Academy of Dermatology. 2014 Mar:70(3):443-8. doi: 10.1016/j.jaad.2013.11.008. Epub 2013 Dec 24
[PubMed PMID: 24373777]
[23]
Greveling K, Wakkee M, Nijsten T, van den Bos RR, Hollestein LM. Epidemiology of Lentigo Maligna and Lentigo Maligna Melanoma in the Netherlands, 1989-2013. The Journal of investigative dermatology. 2016 Oct:136(10):1955-1960. doi: 10.1016/j.jid.2016.06.014. Epub 2016 Jun 24
[PubMed PMID: 27349862]
[24]
Higgins HW 2nd, Lee KC, Galan A, Leffell DJ. Melanoma in situ: Part I. Epidemiology, screening, and clinical features. Journal of the American Academy of Dermatology. 2015 Aug:73(2):181-90, quiz 191-2. doi: 10.1016/j.jaad.2015.04.014. Epub
[PubMed PMID: 26183967]
[25]
Buettner PG, Leiter U, Eigentler TK, Garbe C. Development of prognostic factors and survival in cutaneous melanoma over 25 years: An analysis of the Central Malignant Melanoma Registry of the German Dermatological Society. Cancer. 2005 Feb 1:103(3):616-24
[PubMed PMID: 15630700]
[26]
Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SA, Behjati S, Biankin AV, Bignell GR, Bolli N, Borg A, Børresen-Dale AL, Boyault S, Burkhardt B, Butler AP, Caldas C, Davies HR, Desmedt C, Eils R, Eyfjörd JE, Foekens JA, Greaves M, Hosoda F, Hutter B, Ilicic T, Imbeaud S, Imielinski M, Jäger N, Jones DT, Jones D, Knappskog S, Kool M, Lakhani SR, López-Otín C, Martin S, Munshi NC, Nakamura H, Northcott PA, Pajic M, Papaemmanuil E, Paradiso A, Pearson JV, Puente XS, Raine K, Ramakrishna M, Richardson AL, Richter J, Rosenstiel P, Schlesner M, Schumacher TN, Span PN, Teague JW, Totoki Y, Tutt AN, Valdés-Mas R, van Buuren MM, van 't Veer L, Vincent-Salomon A, Waddell N, Yates LR, Australian Pancreatic Cancer Genome Initiative, ICGC Breast Cancer Consortium, ICGC MMML-Seq Consortium, ICGC PedBrain, Zucman-Rossi J, Futreal PA, McDermott U, Lichter P, Meyerson M, Grimmond SM, Siebert R, Campo E, Shibata T, Pfister SM, Campbell PJ, Stratton MR. Signatures of mutational processes in human cancer. Nature. 2013 Aug 22:500(7463):415-21. doi: 10.1038/nature12477. Epub 2013 Aug 14
[PubMed PMID: 23945592]
[27]
Mar VJ, Wong SQ, Li J, Scolyer RA, McLean C, Papenfuss AT, Tothill RW, Kakavand H, Mann GJ, Thompson JF, Behren A, Cebon JS, Wolfe R, Kelly JW, Dobrovic A, McArthur GA. BRAF/NRAS wild-type melanomas have a high mutation load correlating with histologic and molecular signatures of UV damage. Clinical cancer research : an official journal of the American Association for Cancer Research. 2013 Sep 1:19(17):4589-98. doi: 10.1158/1078-0432.CCR-13-0398. Epub 2013 Jul 5
[PubMed PMID: 23833303]
[28]
Whiteman DC, Whiteman CA, Green AC. Childhood sun exposure as a risk factor for melanoma: a systematic review of epidemiologic studies. Cancer causes & control : CCC. 2001 Jan:12(1):69-82
[PubMed PMID: 11227927]
Level 1 (high-level) evidence
[29]
Davis EJ, Johnson DB, Sosman JA, Chandra S. Melanoma: What do all the mutations mean? Cancer. 2018 Sep 1:124(17):3490-3499. doi: 10.1002/cncr.31345. Epub 2018 Apr 17
[PubMed PMID: 29663336]
[30]
Sanchez MI, Grichnik JM. Melanoma's high C}T mutation rate: is deamination playing a role? Experimental dermatology. 2014 Aug:23(8):551-2. doi: 10.1111/exd.12436. Epub 2014 Aug 1
[PubMed PMID: 24815223]
[31]
Bastian BC. The molecular pathology of melanoma: an integrated taxonomy of melanocytic neoplasia. Annual review of pathology. 2014:9():239-71. doi: 10.1146/annurev-pathol-012513-104658. Epub
[PubMed PMID: 24460190]
[32]
Lee JH, Choi JW, Kim YS. Frequencies of BRAF and NRAS mutations are different in histological types and sites of origin of cutaneous melanoma: a meta-analysis. The British journal of dermatology. 2011 Apr:164(4):776-84. doi: 10.1111/j.1365-2133.2010.10185.x. Epub 2011 Mar 21
[PubMed PMID: 21166657]
Level 1 (high-level) evidence
[33]
Lang J, MacKie RM. Prevalence of exon 15 BRAF mutations in primary melanoma of the superficial spreading, nodular, acral, and lentigo maligna subtypes. The Journal of investigative dermatology. 2005 Sep:125(3):575-9
[PubMed PMID: 16117801]
[34]
Curtin JA, Busam K, Pinkel D, Bastian BC. Somatic activation of KIT in distinct subtypes of melanoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2006 Sep 10:24(26):4340-6
[PubMed PMID: 16908931]
[35]
Weyers W, Bonczkowitz M, Weyers I, Bittinger A, Schill WB. Melanoma in situ versus melanocytic hyperplasia in sun-damaged skin. Assessment of the significance of histopathologic criteria for differential diagnosis. The American Journal of dermatopathology. 1996 Dec:18(6):560-6
[PubMed PMID: 8989926]
[36]
McGuire LK, Disa JJ, Lee EH, Busam KJ, Nehal KS. Melanoma of the lentigo maligna subtype: diagnostic challenges and current treatment paradigms. Plastic and reconstructive surgery. 2012 Feb:129(2):288e-299e. doi: 10.1097/PRS.0b013e31823aeb72. Epub
[PubMed PMID: 22286443]
[37]
Green A, Little JH, Weedon D. The diagnosis of Hutchinson's melanotic freckle (lentigo maligna) in Queensland. Pathology. 1983 Jan:15(1):33-5
[PubMed PMID: 6856341]
[38]
Smoller BR. Histologic criteria for diagnosing primary cutaneous malignant melanoma. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc. 2006 Feb:19 Suppl 2():S34-40
[PubMed PMID: 16446714]
[39]
Martínez-Leboráns L, Garcías-Ladaria J, Oliver-Martínez V, Alegre de Miquel V. Extrafacial Lentigo Maligna: A Report on 14 Cases and a Review of the Literature. Actas dermo-sifiliograficas. 2016 Oct:107(8):e57-63. doi: 10.1016/j.ad.2015.10.018. Epub 2016 May 11
[PubMed PMID: 27180003]
Level 3 (low-level) evidence
[40]
Weinstock MA, Sober AJ. The risk of progression of lentigo maligna to lentigo maligna melanoma. The British journal of dermatology. 1987 Mar:116(3):303-10
[PubMed PMID: 3567069]
[41]
Bosbous MW, Dzwierzynski WW, Neuburg M. Staged excision of lentigo maligna and lentigo maligna melanoma: a 10-year experience. Plastic and reconstructive surgery. 2009 Dec:124(6):1947-1955. doi: 10.1097/PRS.0b013e3181bcf002. Epub
[PubMed PMID: 19952650]
[42]
Hazan C, Dusza SW, Delgado R, Busam KJ, Halpern AC, Nehal KS. Staged excision for lentigo maligna and lentigo maligna melanoma: A retrospective analysis of 117 cases. Journal of the American Academy of Dermatology. 2008 Jan:58(1):142-8
[PubMed PMID: 18029055]
Level 2 (mid-level) evidence
[43]
Penneys NS. Microinvasive lentigo maligna melanoma. Journal of the American Academy of Dermatology. 1987 Oct:17(4):675-80
[PubMed PMID: 3312317]
[44]
Somach SC, Taira JW, Pitha JV, Everett MA. Pigmented lesions in actinically damaged skin. Histopathologic comparison of biopsy and excisional specimens. Archives of dermatology. 1996 Nov:132(11):1297-302
[PubMed PMID: 8915306]
[45]
Jackson R, Williamson GS, Beattie WG. Lentigo maligna and malignant melanoma. Canadian Medical Association journal. 1966 Oct 22:95(17):846-51
[PubMed PMID: 5922502]
[46]
Clark WH Jr, Mihm MC Jr. Lentigo maligna and lentigo-maligna melanoma. The American journal of pathology. 1969 Apr:55(1):39-67
[PubMed PMID: 5776171]
[47]
Cognetta AB Jr, Stolz W, Katz B, Tullos J, Gossain S. Dermatoscopy of lentigo maligna. Dermatologic clinics. 2001 Apr:19(2):307-18
[PubMed PMID: 11556239]
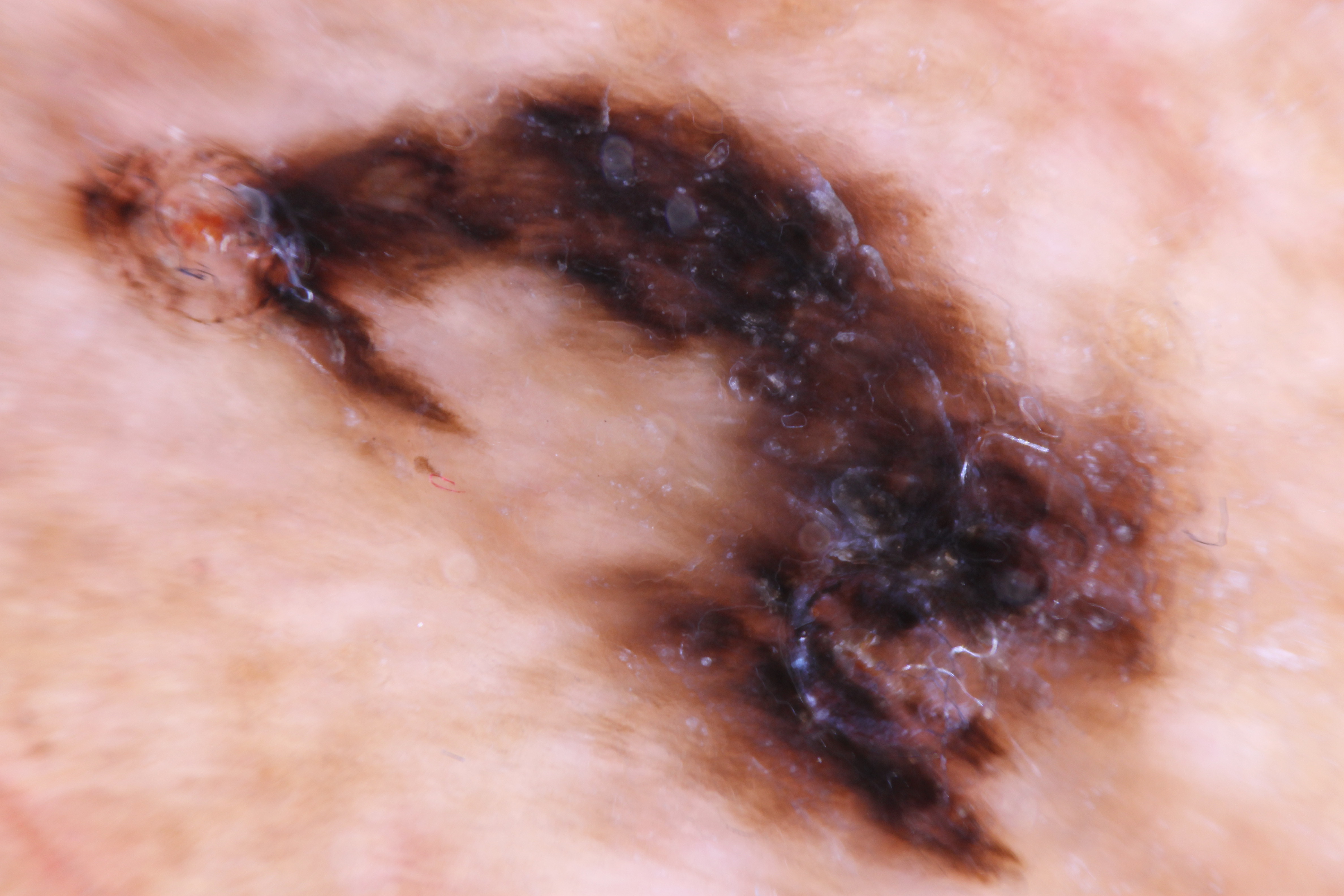
[48]
Bollea-Garlatti LA, Galimberti GN, Galimberti RL. Lentigo Maligna: Keys to Dermoscopic Diagnosis. Actas dermo-sifiliograficas. 2016 Jul-Aug:107(6):489-97. doi: 10.1016/j.ad.2016.01.001. Epub 2016 Feb 11
[PubMed PMID: 26875792]
[49]
Annessi G, Bono R, Abeni D. Correlation between digital epiluminescence microscopy parameters and histopathological changes in lentigo maligna and solar lentigo: A dermoscopic index for the diagnosis of lentigo maligna. Journal of the American Academy of Dermatology. 2017 Feb:76(2):234-243. doi: 10.1016/j.jaad.2016.08.032. Epub 2016 Oct 26
[PubMed PMID: 28341252]
[50]
Mataca E, Migaldi M, Cesinaro AM. Impact of Dermoscopy and Reflectance Confocal Microscopy on the Histopathologic Diagnosis of Lentigo Maligna/Lentigo Maligna Melanoma. The American Journal of dermatopathology. 2018 Dec:40(12):884-889. doi: 10.1097/DAD.0000000000001212. Epub
[PubMed PMID: 29933314]
[51]
Guitera P, Pellacani G, Crotty KA, Scolyer RA, Li LX, Bassoli S, Vinceti M, Rabinovitz H, Longo C, Menzies SW. The impact of in vivo reflectance confocal microscopy on the diagnostic accuracy of lentigo maligna and equivocal pigmented and nonpigmented macules of the face. The Journal of investigative dermatology. 2010 Aug:130(8):2080-91. doi: 10.1038/jid.2010.84. Epub 2010 Apr 15
[PubMed PMID: 20393481]
[52]
Chen CS, Elias M, Busam K, Rajadhyaksha M, Marghoob AA. Multimodal in vivo optical imaging, including confocal microscopy, facilitates presurgical margin mapping for clinically complex lentigo maligna melanoma. The British journal of dermatology. 2005 Nov:153(5):1031-6
[PubMed PMID: 16225620]
[53]
Robinson JK. Use of digital epiluminescence microscopy to help define the edge of lentigo maligna. Archives of dermatology. 2004 Sep:140(9):1095-100
[PubMed PMID: 15381550]
[54]
Osborne JE, Hutchinson PE. A follow-up study to investigate the efficacy of initial treatment of lentigo maligna with surgical excision. British journal of plastic surgery. 2002 Dec:55(8):611-5
[PubMed PMID: 12550112]
[55]
Coit DG, Thompson JA, Andtbacka R, Anker CJ, Bichakjian CK, Carson WE 3rd, Daniels GA, Daud A, Dimaio D, Fleming MD, Gonzalez R, Guild V, Halpern AC, Hodi FS Jr, Kelley MC, Khushalani NI, Kudchadkar RR, Lange JR, Martini MC, Olszanski AJ, Ross MI, Salama A, Swetter SM, Tanabe KK, Trisal V, Urist MM, McMillian NR, Ho M, National Comprehensive Cancer Network. Melanoma, version 4.2014. Journal of the National Comprehensive Cancer Network : JNCCN. 2014 May:12(5):621-9
[PubMed PMID: 24812131]
[56]
Kunishige JH, Doan L, Brodland DG, Zitelli JA. Comparison of surgical margins for lentigo maligna versus melanoma in situ. Journal of the American Academy of Dermatology. 2019 Jul:81(1):204-212. doi: 10.1016/j.jaad.2019.01.051. Epub 2019 Apr 20
[PubMed PMID: 31014825]
[57]
Jejurikar SS, Borschel GH, Johnson TM, Lowe L, Brown DL. Immediate, optimal reconstruction of facial lentigo maligna and melanoma following total peripheral margin control. Plastic and reconstructive surgery. 2007 Oct:120(5):1249-1255. doi: 10.1097/01.prs.0000279324.35616.72. Epub
[PubMed PMID: 17898597]
[58]
Bosbous MW, Dzwierzynski WW, Neuburg M. Lentigo maligna: diagnosis and treatment. Clinics in plastic surgery. 2010 Jan:37(1):35-46. doi: 10.1016/j.cps.2009.08.006. Epub
[PubMed PMID: 19914456]
[59]
Bichakjian CK, Halpern AC, Johnson TM, Foote Hood A, Grichnik JM, Swetter SM, Tsao H, Barbosa VH, Chuang TY, Duvic M, Ho VC, Sober AJ, Beutner KR, Bhushan R, Smith Begolka W, American Academy of Dermatology. Guidelines of care for the management of primary cutaneous melanoma. American Academy of Dermatology. Journal of the American Academy of Dermatology. 2011 Nov:65(5):1032-47. doi: 10.1016/j.jaad.2011.04.031. Epub 2011 Aug 25
[PubMed PMID: 21868127]
[60]
Coit DG, Thompson JA, Algazi A, Andtbacka R, Bichakjian CK, Carson WE 3rd, Daniels GA, DiMaio D, Ernstoff M, Fields RC, Fleming MD, Gonzalez R, Guild V, Halpern AC, Hodi FS Jr, Joseph RW, Lange JR, Martini MC, Materin MA, Olszanski AJ, Ross MI, Salama AK, Skitzki J, Sosman J, Swetter SM, Tanabe KK, Torres-Roca JF, Trisal V, Urist MM, McMillian N, Engh A. Melanoma, Version 2.2016, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network : JNCCN. 2016 Apr:14(4):450-73
[PubMed PMID: 27059193]
Level 1 (high-level) evidence
[61]
Nosrati A, Berliner JG, Goel S, McGuire J, Morhenn V, de Souza JR, Yeniay Y, Singh R, Lee K, Nakamura M, Wu RR, Griffin A, Grimes B, Linos E, Chren MM, Grekin R, Wei ML. Outcomes of Melanoma In Situ Treated With Mohs Micrographic Surgery Compared With Wide Local Excision. JAMA dermatology. 2017 May 1:153(5):436-441. doi: 10.1001/jamadermatol.2016.6138. Epub
[PubMed PMID: 28241261]
[62]
Beaulieu D, Fathi R, Srivastava D, Nijhawan RI. Current perspectives on Mohs micrographic surgery for melanoma. Clinical, cosmetic and investigational dermatology. 2018:11():309-320. doi: 10.2147/CCID.S137513. Epub 2018 Jun 20
[PubMed PMID: 29950878]
Level 3 (low-level) evidence
[63]
Hou JL, Reed KB, Knudson RM, Mirzoyev SA, Lohse CM, Frohm ML, Brewer JD, Otley CC, Roenigk RK. Five-year outcomes of wide excision and Mohs micrographic surgery for primary lentigo maligna in an academic practice cohort. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2015 Feb:41(2):211-8. doi: 10.1097/DSS.0000000000000248. Epub
[PubMed PMID: 25590473]
[64]
Etzkorn JR, Sobanko JF, Elenitsas R, Newman JG, Goldbach H, Shin TM, Miller CJ. Low recurrence rates for in situ and invasive melanomas using Mohs micrographic surgery with melanoma antigen recognized by T cells 1 (MART-1) immunostaining: tissue processing methodology to optimize pathologic staging and margin assessment. Journal of the American Academy of Dermatology. 2015 May:72(5):840-50. doi: 10.1016/j.jaad.2015.01.007. Epub 2015 Mar 13
[PubMed PMID: 25774012]
[65]
Marsden JR, Fox R, Boota NM, Cook M, Wheatley K, Billingham LJ, Steven NM, NCRI Skin Cancer Clinical Studies Group, the U.K. Dermatology Clinical Trials Network and the LIMIT-1 Collaborative Group. Effect of topical imiquimod as primary treatment for lentigo maligna: the LIMIT-1 study. The British journal of dermatology. 2017 May:176(5):1148-1154. doi: 10.1111/bjd.15112. Epub 2017 Apr 10
[PubMed PMID: 27714781]
[66]
Mora AN, Karia PS, Nguyen BM. A quantitative systematic review of the efficacy of imiquimod monotherapy for lentigo maligna and an analysis of factors that affect tumor clearance. Journal of the American Academy of Dermatology. 2015 Aug:73(2):205-12. doi: 10.1016/j.jaad.2015.05.022. Epub 2015 Jun 16
[PubMed PMID: 26088690]
Level 1 (high-level) evidence
[67]
Fogarty GB, Hong A, Scolyer RA, Lin E, Haydu L, Guitera P, Thompson J. Radiotherapy for lentigo maligna: a literature review and recommendations for treatment. The British journal of dermatology. 2014 Jan:170(1):52-8. doi: 10.1111/bjd.12611. Epub
[PubMed PMID: 24032599]
[68]
Farshad A, Burg G, Panizzon R, Dummer R. A retrospective study of 150 patients with lentigo maligna and lentigo maligna melanoma and the efficacy of radiotherapy using Grenz or soft X-rays. The British journal of dermatology. 2002 Jun:146(6):1042-6
[PubMed PMID: 12072074]
Level 2 (mid-level) evidence
[69]
Tsang RW, Liu FF, Wells W, Payne DG. Lentigo maligna of the head and neck. Results of treatment by radiotherapy. Archives of dermatology. 1994 Aug:130(8):1008-12
[PubMed PMID: 8053696]
[70]
Gershenwald JE, Scolyer RA. Melanoma Staging: American Joint Committee on Cancer (AJCC) 8th Edition and Beyond. Annals of surgical oncology. 2018 Aug:25(8):2105-2110. doi: 10.1245/s10434-018-6513-7. Epub 2018 May 30
[PubMed PMID: 29850954]
[71]
Gambichler T, Kempka J, Kampilafkos P, Bechara FG, Altmeyer P, Stücker M. Clinicopathological characteristics of 270 patients with lentigo maligna and lentigo maligna melanoma: data from a German skin cancer centre. The British journal of dermatology. 2014 Dec:171(6):1605-7. doi: 10.1111/bjd.13204. Epub 2014 Oct 22
[PubMed PMID: 24958545]
[72]
Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Atkins MB, Byrd DR, Buzaid AC, Cochran AJ, Coit DG, Ding S, Eggermont AM, Flaherty KT, Gimotty PA, Kirkwood JM, McMasters KM, Mihm MC Jr, Morton DL, Ross MI, Sober AJ, Sondak VK. Final version of 2009 AJCC melanoma staging and classification. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2009 Dec 20:27(36):6199-206. doi: 10.1200/JCO.2009.23.4799. Epub 2009 Nov 16
[PubMed PMID: 19917835]
[73]
Walling HW, Scupham RK, Bean AK, Ceilley RI. Staged excision versus Mohs micrographic surgery for lentigo maligna and lentigo maligna melanoma. Journal of the American Academy of Dermatology. 2007 Oct:57(4):659-64
[PubMed PMID: 17870430]
[74]
Swetter SM, Tsao H, Bichakjian CK, Curiel-Lewandrowski C, Elder DE, Gershenwald JE, Guild V, Grant-Kels JM, Halpern AC, Johnson TM, Sober AJ, Thompson JA, Wisco OJ, Wyatt S, Hu S, Lamina T. Guidelines of care for the management of primary cutaneous melanoma. Journal of the American Academy of Dermatology. 2019 Jan:80(1):208-250. doi: 10.1016/j.jaad.2018.08.055. Epub 2018 Nov 1
[PubMed PMID: 30392755]
[75]
Kantor J, Kantor DE. Routine dermatologist-performed full-body skin examination and early melanoma detection. Archives of dermatology. 2009 Aug:145(8):873-6. doi: 10.1001/archdermatol.2009.137. Epub
[PubMed PMID: 19687416]
[76]
Gerbert B, Maurer T, Berger T, Pantilat S, McPhee SJ, Wolff M, Bronstone A, Caspers N. Primary care physicians as gatekeepers in managed care. Primary care physicians' and dermatologists' skills at secondary prevention of skin cancer. Archives of dermatology. 1996 Sep:132(9):1030-8
[PubMed PMID: 8795541]
[77]
Roetzheim RG, Pal N, van Durme DJ, Wathington D, Ferrante JM, Gonzalez EC, Krischer JP. Increasing supplies of dermatologists and family physicians are associated with earlier stage of melanoma detection. Journal of the American Academy of Dermatology. 2000 Aug:43(2 Pt 1):211-8
[PubMed PMID: 10906640]