[1]
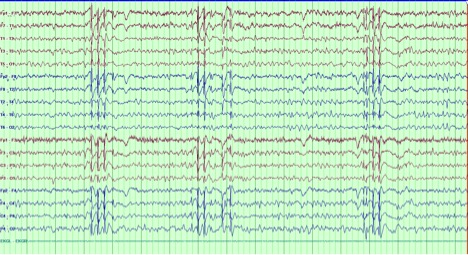
Koutroumanidis M, Arzimanoglou A, Caraballo R, Goyal S, Kaminska A, Laoprasert P, Oguni H, Rubboli G, Tatum W, Thomas P, Trinka E, Vignatelli L, Moshé SL. The role of EEG in the diagnosis and classification of the epilepsy syndromes: a tool for clinical practice by the ILAE Neurophysiology Task Force (Part 1). Epileptic disorders : international epilepsy journal with videotape. 2017 Sep 1:19(3):233-298. doi: 10.1684/epd.2017.0935. Epub
[PubMed PMID: 28984246]
[2]
Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J, Guilhoto L, Hirsch E, Jain S, Mathern GW, Moshé SL, Nordli DR, Perucca E, Tomson T, Wiebe S, Zhang YH, Zuberi SM. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017 Apr:58(4):512-521. doi: 10.1111/epi.13709. Epub 2017 Mar 8
[PubMed PMID: 28276062]
[4]
Asadi-Pooya AA, Emami M, Sperling MR. A clinical study of syndromes of idiopathic (genetic) generalized epilepsy. Journal of the neurological sciences. 2013 Jan 15:324(1-2):113-7. doi: 10.1016/j.jns.2012.10.014. Epub 2012 Nov 10
[PubMed PMID: 23149265]
[5]
Sidenvall R, Forsgren L, Blomquist HK, Heijbel J. A community-based prospective incidence study of epileptic seizures in children. Acta paediatrica (Oslo, Norway : 1992). 1993 Jan:82(1):60-5
[PubMed PMID: 8453224]
[6]
Jallon P, Latour P. Epidemiology of idiopathic generalized epilepsies. Epilepsia. 2005:46 Suppl 9():10-4
[PubMed PMID: 16302871]
[7]
Olafsson E, Hauser WA, Ludvigsson P, Gudmundsson G. Incidence of epilepsy in rural Iceland: a population-based study. Epilepsia. 1996 Oct:37(10):951-5
[PubMed PMID: 8822693]
[8]
Wirrell E. Infantile, Childhood, and Adolescent Epilepsies. Continuum (Minneapolis, Minn.). 2016 Feb:22(1 Epilepsy):60-93. doi: 10.1212/CON.0000000000000269. Epub
[PubMed PMID: 26844731]
[9]
Heron SE, Khosravani H, Varela D, Bladen C, Williams TC, Newman MR, Scheffer IE, Berkovic SF, Mulley JC, Zamponi GW. Extended spectrum of idiopathic generalized epilepsies associated with CACNA1H functional variants. Annals of neurology. 2007 Dec:62(6):560-8
[PubMed PMID: 17696120]
[10]
Trinka E, Baumgartner S, Unterberger I, Unterrainer J, Luef G, Haberlandt E, Bauer G. Long-term prognosis for childhood and juvenile absence epilepsy. Journal of neurology. 2004 Oct:251(10):1235-41
[PubMed PMID: 15503104]
[11]
Glauser T, Ben-Menachem E, Bourgeois B, Cnaan A, Guerreiro C, Kälviäinen R, Mattson R, French JA, Perucca E, Tomson T, ILAE Subcommission on AED Guidelines. Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2013 Mar:54(3):551-63. doi: 10.1111/epi.12074. Epub 2013 Jan 25
[PubMed PMID: 23350722]
[12]
Moosa ANV. Antiepileptic Drug Treatment of Epilepsy in Children. Continuum (Minneapolis, Minn.). 2019 Apr:25(2):381-407. doi: 10.1212/CON.0000000000000712. Epub
[PubMed PMID: 30921015]
[13]
Pearl PL. Epilepsy Syndromes in Childhood. Continuum (Minneapolis, Minn.). 2018 Feb:24(1, Child Neurology):186-209. doi: 10.1212/CON.0000000000000568. Epub
[PubMed PMID: 29432243]
[14]
Bouma PA, Westendorp RG, van Dijk JG, Peters AC, Brouwer OF. The outcome of absence epilepsy: a meta-analysis. Neurology. 1996 Sep:47(3):802-8
[PubMed PMID: 8797483]
Level 1 (high-level) evidence
[15]
Healy L, Moran M, Singhal S, O'Donoghue MF, Alzoubidi R, Whitehouse WP. Relapse after treatment withdrawal of antiepileptic drugs for Juvenile Absence Epilepsy and Juvenile Myoclonic Epilepsy. Seizure. 2018 Jul:59():116-122. doi: 10.1016/j.seizure.2018.05.015. Epub 2018 May 20
[PubMed PMID: 29807291]
[16]
Shinnar S, Berg AT, Moshé SL, Kang H, O'Dell C, Alemany M, Goldensohn ES, Hauser WA. Discontinuing antiepileptic drugs in children with epilepsy: a prospective study. Annals of neurology. 1994 May:35(5):534-45
[PubMed PMID: 8179299]
[17]
Aiguabella Macau M, Falip Centellas M, Veciana de Las Heras M, Climent Perín MA, Miró Lladó J, Moreno Gómez I, Elices Palomar E. Long term prognosis of juvenile absence epilepsy. Neurologia (Barcelona, Spain). 2011 May:26(4):193-9. doi: 10.1016/j.nrl.2010.09.005. Epub 2010 Nov 13
[PubMed PMID: 21163225]
[18]
Verducci C, Hussain F, Donner E, Moseley BD, Buchhalter J, Hesdorffer D, Friedman D, Devinsky O. SUDEP in the North American SUDEP Registry: The full spectrum of epilepsies. Neurology. 2019 Jul 16:93(3):e227-e236. doi: 10.1212/WNL.0000000000007778. Epub 2019 Jun 19
[PubMed PMID: 31217259]
[19]
Holtkamp M, Janz D, Kirschbaum A, Kowski AB, Vorderwülbecke BJ. Absence epilepsy beyond adolescence: an outcome analysis after 45 years of follow-up. Journal of neurology, neurosurgery, and psychiatry. 2018 Jun:89(6):603-610. doi: 10.1136/jnnp-2017-317052. Epub 2018 Jan 18
[PubMed PMID: 29348303]
[20]
Beghi M, Beghi E, Cornaggia CM, Gobbi G. Idiopathic generalized epilepsies of adolescence. Epilepsia. 2006:47 Suppl 2():107-10
[PubMed PMID: 17105478]
[21]
Tovia E, Goldberg-Stern H, Shahar E, Kramer U. Outcome of children with juvenile absence epilepsy. Journal of child neurology. 2006 Sep:21(9):766-8
[PubMed PMID: 16970883]
[22]
Fonseca Wald ELA, Klinkenberg S, Voncken TPC, Ebus SCM, Aldenkamp AP, Vles JSH, Vermeulen RJ, Hendriksen JGM, Debeij-Van Hall MHJA. Cognitive development in absence epilepsy during long-term follow-up. Child neuropsychology : a journal on normal and abnormal development in childhood and adolescence. 2019 Nov:25(8):1003-1021. doi: 10.1080/09297049.2019.1614156. Epub 2019 May 30
[PubMed PMID: 31145023]
[23]
Caplan R, Siddarth P, Stahl L, Lanphier E, Vona P, Gurbani S, Koh S, Sankar R, Shields WD. Childhood absence epilepsy: behavioral, cognitive, and linguistic comorbidities. Epilepsia. 2008 Nov:49(11):1838-46. doi: 10.1111/j.1528-1167.2008.01680.x. Epub 2008 Jun 13
[PubMed PMID: 18557780]
[24]
Cheng D, Yan X, Gao Z, Xu K, Zhou X, Chen Q. Common and Distinctive Patterns of Cognitive Dysfunction in Children With Benign Epilepsy Syndromes. Pediatric neurology. 2017 Jul:72():36-41.e1. doi: 10.1016/j.pediatrneurol.2016.12.005. Epub 2017 Jan 4
[PubMed PMID: 28533141]
[25]
Montouris G, Aboumatar S, Burdette D, Kothare S, Kuzniecky R, Rosenfeld W, Chung S. Expert opinion: Proposed diagnostic and treatment algorithms for Lennox-Gastaut syndrome in adult patients. Epilepsy & behavior : E&B. 2020 Sep:110():107146. doi: 10.1016/j.yebeh.2020.107146. Epub 2020 Jun 18
[PubMed PMID: 32563898]
Level 3 (low-level) evidence