Continuing Education Activity
Intercostal nerve blockade is a selective superficial regional anesthesia technique easily performed at the bedside with or without ultrasound guidance. Intercostal nerve blockade is a diagnostic and therapeutic procedure that can provide analgesia or augment anesthesia in various circumstances, such as blunt thoracic trauma, chest wall surgeries, and postherpetic neuralgia. The procedure is generally well-tolerated and has a low complication rate, particularly when performed under ultrasound guidance. In addition, when used in the perioperative period, intracostal nerve blockade can reduce patient opioid consumption. This activity describes the anatomy clinically relevant to intercostal nerve blockade and the indications, contraindications, and complications of this procedure. The activity also reviews the best practices in performing the procedure and the role of the interprofessional team in providing care to patients undergoing ultrasound-guided intercostal nerve blockade.
Objectives:
- Identify the indications for intercostal nerve blockade based on the patient's clinical condition.
- Employ best practices when performing ultrasound-guided intercostal nerve blockade as a part of multimodal pain management.
- Assess and manage the adverse events most commonly associated with intercostal nerve blocks.
- Apply effective interprofessional team strategies for improving care coordination and communication to better manage pain, reduce opioid usage, and improve patient outcomes.
Introduction
Intercostal nerve blockade is a selective superficial regional anesthesia technique easily performed at the bedside with or without ultrasound guidance. Intercostal nerve blockade is a diagnostic and therapeutic procedure that can provide analgesia or augment anesthesia in various circumstances, such as blunt thoracic trauma, chest wall surgeries, and postherpetic neuralgia. The procedure is generally well-tolerated and has a low complication rate, particularly when performed under ultrasound guidance.
Anatomy and Physiology
The intercostal nerves are the anterior/ventral rami of the T1-T11 spinal nerves. Intercostal nerves are mixed nerves that carry sensory and motor fibers. The intercostal sensory afferent nerves are to the skin of the chest wall and abdomen, ribs, pleurae, and peritoneum. The motor innervation is to the intercostal and abdominal wall muscles. The intercostal nerves are located within or near the inferior groove of their corresponding rib between the posterior intercostal membranes and the parietal pleura. The anterior/ventral ramus of the T12 spinal nerve runs inferior to the bottom rib and is called the subcostal nerve. There are typical and atypical intercostal nerves; atypical intercostal nerves go beyond the thoracic wall to supply other anatomical regions.[1]
Generally, each typical intercostal nerve gives off six branches. The first branch is the rami communicantes, which connects to its correlating sympathetic ganglion. The second branch is the posterior communicating nerve which innervates the skin and muscles in the paraspinal area. The third branch is the muscular branch; muscles innervated by this branch include the serratus anterior, latissimus dorsi, and the intercostal and abdominal wall muscles. The fourth branch of a typical intercostal nerve is the anterior cutaneous branch which travels along the subcostal groove. The branch exits near the midline and divides into medial and lateral branches to supply the anterior portion of the chest. Collateral branches of intercostal nerves, when present, run along the superior border of the rib below. Finally, the last branch of a typical intercostal nerve is the lateral cutaneous branch, which pierces the external intercostal muscle near the midaxillary line and divides into anterior and posterior branches to supply the lateral side of the chest.
The third through sixth intercostal nerves are considered typical and innervate the parietal pleura of the thorax.
The first, second, and seventh through eleventh intercostal nerves are considered atypical. The first intercostal nerve is derived from the anterior ramus of the T1 spinal nerve. This nerve bifurcates into superior and inferior branches around the neck of the first rib. The superior branch joins the brachial plexus, and the inferior or intercostal branch runs below the first rib. The lateral cutaneous branch of the second intercostal nerve, the intercostobrachial nerve, supplies the axillary floor and the upper posteromedial region of the upper extremity. The fifth through eleventh intercostal nerves innervate the parietal peritoneum and the musculature and skin of the anterior abdominal wall.
Except for the first intercostal and subcostal nerves, the intercostal nerves do not constitute a plexus and trace an autonomous course.
Indications
Intercostal nerve blockade has both diagnostic and therapeutic applications. Blocking sensation from the skin and subcutaneous tissues of the thoracic wall provides analgesia for conditions such as costochondritis, shingles, and postherpetic neuralgia. Intercostal nerve blockade may augment postoperative analgesia after procedures involving the chest wall, including the breast tissue; intercostal nerve blockade has been shown to alleviate pain after lumpectomy, partial mastectomy or wide local excision, complete mastectomy, and breast reconstruction.[2][3]
The simplicity of intercostal nerve blockade allows for its use at the bedside in the emergency department, making it an excellent option in the therapeutic approach to blunt thoracic trauma, sternal fractures, and fractures of multiple ribs.[4] Intercostal nerve blockade provides adequate anesthesia for chest tube placement.
Patients with pain originating from the thoracic spine or atypical chest wall pain may also benefit from intercostal nerve blockade. In circumstances of atypical chest wall pain, intercostal nerve blockade may be diagnostic and therapeutic.
Contraindications
Intercostal nerve blockade has both absolute and relative contraindications. Therefore, it is essential to consider these contraindications when evaluating the suitability of intercostal nerve blockade for a patient.
Absolute contraindications include patient rejection, presence of infection at the injection site, patient allergy to local anesthetics, unavailability of sterile equipment, high risk of local anesthetic toxicity after previous attempts or bilateral blocks, lack of skills to perform the block, and unavailability of a resuscitation kit.
On the other hand, relative contraindications encompass unresponsive patients who cannot report toxicity, the presence of bleeding disorders or use of blood thinners, risk of tissue ischemia from distal extremity or organ blockade, and potential worsening of previous peripheral nerve neuropathies. Additionally, the procedure is relatively contraindicated in the pediatric patient population and patients with dementia or severe agitation.
Equipment
The following supplies are necessary for intercostal nerve blocks.
- Ultrasound machine with a high-frequency 8- to 13-MHz linear transducer
- Sonographic sterile cover
- Marking pen
- Sterile gloves
- Clear drapes
- 2% chlorhexidine gluconate antimicrobial skin cleanser
- 20- to 22-gauge, 4- to 5-cm needle
- Lidocaine 1%
- Gauze, 2 inch
- 3-, 12-, and 20-mL syringes
The following equipment is required when performing intercostal nerve blocks.
- Standard American Society of Anesthesiologists (ASA) monitors: 3-lead ECG, blood pressure, pulse oximetry, and nasal cannula with EtCO2 detector
- Resuscitation equipment and ACLS medications
- Lipid Emulsion 20% (an accepted treatment for severe local anesthetic systemic toxicity). Epinephrine and benzodiazepines are also helpful during this severe adverse event.
Personnel
Intercostal nerve blockade is traditionally performed by a board-certified anesthesiologist skilled in providing competent and safe ultrasound-guided regional anesthesia. A qualified assistant is usually required.
Preparation
Monitors are available to decrease the risk of complications related to regional anesthesia, such as intraneural injection or needle-nerve damage. An expendable in-line pressure-monitoring mechanism for controlling the pressure during local anesthetic injection allows for documentation of injection pressures. Documentation of every stage of this procedure is essential in every institution performing regional anesthesia to ensure effective and safe practice.[5][6]
Technique or Treatment
Intercostal nerve blocks may be performed with or without ultrasound guidance.
Intercostal Nerve Block Without Ultrasound Guidance
- Position the patient in the upright seated, lateral decubitus, or prone position. If seated, place the patient leaning forward over a support to retract the scapulae.
- Cleanse the skin with an antiseptic solution.
- Mark the intended block sites approximately 6 to 8 cm from the midline.
- Infiltrate the injection sites with a preferred local anesthetic.
- Introduce the injection needle in the sagittal plane. Advance the needle approaching the inferior edge of the correspondent rib ending in the subcostal groove.
- Inject a small amount of local anesthetic to desensitize the periosteum.
- Advance the needle forward another 2 to 3 mm; a "pop" may be felt as the needle traverses the internal intercostal fascia.
- Aspirate for blood to ensure the needle is not positioned intravascularly.
- Inject 3 to 5 mL of local anesthetic.
- Repeat these steps as needed to achieve the desired level of anesthesia.[3]
Intercostal Nerve Block With Ultrasound Guidance
- Position the patient in the upright seated, lateral decubitus, or prone position. If seated, place the patient leaning forward over a support to retract the scapulae.
- Cleanse the skin with an antiseptic solution.
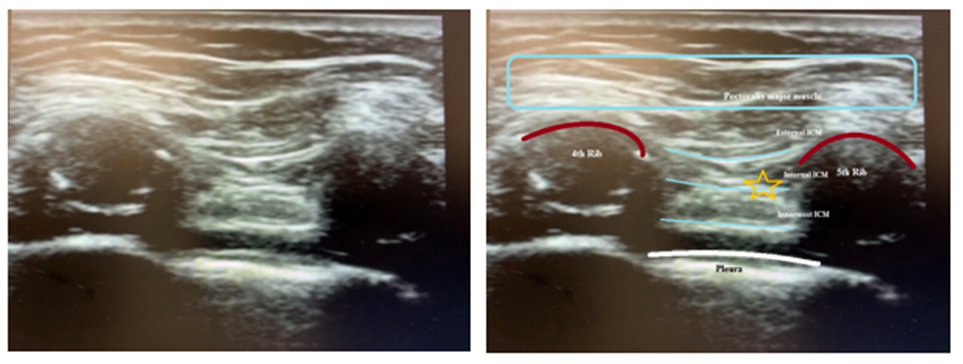
- Place the high-frequency linear transducer in a transverse orientation to identify the external, internal, and innermost intercostal muscles (see Image. Intercostal Nerve Block Landmark).
- Utilize power Doppler or B-mode to localize the blood vessels.
- Identify the angle of the rib with a long-axis view
- Insert the needle in-plane and aim centrally.
- Aspirate for blood.
- Inject the local anesthetic between the innermost and internal intercostal muscle layers.
- Ultrasonography will reveal an indentation in the pleura after injection of the local anesthetic.
While a single injection can provide the adequate central spread of the anesthetic to anesthetize different intercostal spaces, injections at multiple levels are often required to provide a better quality of analgesia. Detailed calculation of the local anesthetic total dose is required; the peak plasma levels after intercostal nerve blockade are high and occur quickly.[5][6]
After ensuring the needle tip is in the proper tissue plane, the injection of 0.1 to 0.15 mL/kg per intercostal space, with a maximum dose of 2 to 3 mL per space, is usually adequate to achieve analgesia. Common medications for this blockade are ropivacaine 0.2%, levobupivacaine 0.25%, or bupivacaine 0.25%.[7][8][9] Liposomal bupivacaine is a safe option for managing severe pain in patients undergoing a thoracotomy or mastectomy.[10][11][12]
Complications
Intercostal nerve blockade, while generally safe, is not without potential complications. These complications can include injuries to surrounding tissues, such as the anterior thoracic artery, nearby nerves, parietal pleura resulting in pneumothorax or hemothorax, and muscle laceration. Patients may also experience pain during the procedure; in some cases, the procedure may fail to provide sufficient analgesia. Additionally, there is a risk of infection at the injection sites. It is important to note that local anesthetic systemic toxicity (LAST) is a rare complication that can occur with regional anesthesia. Vigilance and adherence to proper technique and safety protocols are essential in minimizing complications during intercostal nerve blockade.[13]
Clinical Significance
Intercostal nerve blockade typically provides 8 to 12 hours of analgesia with fewer complications than other anatomical blocks or epidural injections. If liposomal bupivacaine is administered during intercostal nerve blockade, analgesia may last up to 72 hours.[10] Intercostal nerve blockade results in decreased postoperative opioid use.[14]
Enhancing Healthcare Team Outcomes
Clinicians performing intercostal nerve blocks must be well-trained in ultrasonographically recognizing the thoracic anatomy and its common variants. All the necessary equipment should be readily available, and good communication with the assistant during the procedure is crucial. Early recognition and urgent management of complications are imperative. Multiple randomized trials have shown that a well-organized interprofessional team of healthcare workers decreases the risk of severe adverse events while performing successful regional anesthesia.
Intercostal nerve blocks are important anesthetic and pain management techniques. Choosing a regional anesthesia technique must consider various factors, in particular, the opinion of the patient, the surgeon, and the preferences of the anesthesiologists who must be able to perform the nerve block without difficulty. For patient safety, it is advisable to follow specific guidelines and protocols to conduct adequate regional anesthesia procedures. Maintaining continuous closed-loop communication between all healthcare team members regarding the need, technique, and potential management issues associated with the regional anesthetic technique is required.
It is necessary to obtain specific and comprehensive informed consent from the patient or their designated and authorized decision maker before initiating regional anesthesia. All team members must communicate their concerns, responsibilities, and activities contemporaneously and as indicated throughout the periprocedural period based on their professional discretion. All team members should respect the free flow of information and concerns among team members without allowing or producing an environment of hostility. All team members should consider it their duty to neither disrupt the work done by other team members nor, through their action or inaction, create additional issues or increase the workload for other team members.