Continuing Education Activity
Gram-positive organisms have highly variable growth and resistance patterns. The SCOPE project (Surveillance and Control of Pathogens of Epidemiologic Importance) found that in those with an underlying malignancy, gram-positive organisms accounted for 62 percent of all bloodstream infections in 1995 and 76 percent in 2000 while gram-negative organisms accounted for 22 percent in 1995 and 14 percent in 2000. This activity reviews the evaluation and management of gram-positive bacterial infections and explains the role of the interprofessional team in improving care for affected patients.
Objectives:
Explain how to evaluate for a gram-positive bacterial infection.
Identify common infections caused by gram-positive bacteria.
Describe treatment strategies for gram-positive bacterial infections.
Outline interprofessional team strategies to improve care coordination and communication to provide quality care to patients with gram-positive bacterial infections.
Introduction
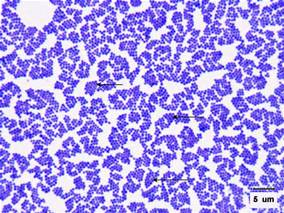
Health professionals need to understand the important difference between gram-positive and gram-negative bacteria. Gram-positive bacteria are bacteria classified by the color they turn in the staining method. Hans Christian Gram developed the staining method in 1884. The staining method uses crystal violet dye, which is retained by the thick peptidoglycan cell wall found in gram-positive organisms. This reaction gives gram-positive organisms a blue color when viewed under a microscope. Although gram-negative organisms classically have an outer membrane, they have a thinner peptidoglycan layer, which does not hold the blue dye used in the initial dying process. Other information used to differentiate bacteria is the shape. Gram-positive bacteria comprise cocci, bacilli, or branching filaments.
Etiology
Gram-positive cocci include Staphylococcus (catalase-positive), which grows clusters, and Streptococcus (catalase-negative), which grows in chains. The staphylococci further subdivide into coagulase-positive (S. aureus) and coagulase-negative (S. epidermidis and S. saprophyticus) species. Streptococcus bacteria subdivide into Strep. pyogenes (Group A), Strep. agalactiae (Group B), enterococci (Group D), Strep viridans, and Strep pneumonia.
Gram-positive bacilli (rods) subdivide according to their ability to produce spores. Bacillus and Clostridia are spore-forming rods while Listeria and Corynebacterium are not. Spore-forming rods that produce spores can survive in environments for many years. Also, the branching filament rods encompass Nocardia and actinomyces.
Gram-positive organisms have a thicker peptidoglycan cell wall compared with gram-negative bacteria. It is a 20 to 80 nm thick polymer while the peptidoglycan layer of the gram-negative cell wall is 2 to 3 nm thick and covered with an outer lipid bilayer membrane.
Epidemiology
Bloodstream infection mortality rates have increased by 78% in just two decades[1]. Gram-positive organisms have highly variable growth and resistance patterns. The SCOPE project (Surveillance and Control of Pathogens of Epidemiologic Importance) found that gram-positive organisms in those with an underlying malignancy accounted for 62% of all bloodstream infections in 1995 and 76% in 2000 while gram-negative organisms accounted for 22% and 14% of infections for these years.[2]
Pathophysiology
Gram-positive cocci:
Staphylococcus aureus is a gram-positive, catalase-positive, coagulase-positive cocci in clusters. S. aureus can cause inflammatory diseases, including skin infections, pneumonia, endocarditis, septic arthritis, osteomyelitis, and abscesses. S. aureus can also cause toxic shock syndrome (TSST-1), scalded skin syndrome (exfoliative toxin, and food poisoning (enterotoxin).
Staphylococcus epidermidis is a gram-positive, catalase-positive, coagulase-negative cocci in clusters and is novobiocin sensitive. S. epidermidis commonly infects prosthetic devices and IV catheters producing biofilms. Staphylococcus saprophyticus is novobiocin resistant and is a normal flora of the genital tract and perineum. S. saprophyticus accounts for the second most common cause of uncomplicated urinary tract infection (UTI).
Streptococcus pneumoniae is a gram-positive, encapsulated, lancet-shaped diplococci, most commonly causing otitis media, pneumonia, sinusitis, and meningitis. Streptococcus viridans consist of Strep. mutans and Strep mitis found in the normal flora of the oropharynx commonly cause dental carries and subacute bacterial endocarditis (Strep. sanguinis).
Streptococcus pyogenes is a gram-positive group A cocci that can cause pyogenic infections (pharyngitis, cellulitis, impetigo, erysipelas), toxigenic infections (scarlet fever, necrotizing fasciitis), and immunologic infections (glomerulonephritis and rheumatic fever). ASO titer detects S. pyogenes infections.
Streptococcus agalactiae is a gram-positive group B cocci that colonize the vagina and is found mainly in babies. Pregnant women need screening for Group-B Strep (GBS) at 35 to 37 weeks of gestation.
Enterococci is a gram-positive group D cocci found mainly in the colonic flora and can cause biliary tract infections and UTIs. Vancomycin-resistant enterococci (VRE) are an important cause of nosocomial infections.
Gram-positive rods:
Clostridia is a gram-positive spore-forming rod consisting of C. tetani, C. botulinum, C. perfringens, and C. difficile. C. difficile is often secondary to antibiotic use (clindamycin/ampicillin), PPI use, and recent hospitalization. Treatment involves primarily with oral vancomycin.
Bacillus anthracis is a gram-positive spore-forming rod that produces anthrax toxin resulting in an ulcer with a black eschar. Bacillus cereus is a gram-positive rod that can be acquired from spores surviving under-cooked or reheated rice. Symptoms include nausea, vomiting, and watery non-bloody diarrhea.
Corynebacterium diphtheria is a gram-positive club-shaped rod that can cause pseudomembranous pharyngitis, myocarditis, and arrhythmias. Toxoid vaccines prevent diphtheria.
Listeria monocytogenes is a gram-positive rod acquired by the ingestion of cold deli meats and unpasteurized dairy products or by vaginal transmission during birth. Listeria can cause neonatal meningitis, meningitis in immunocompromised patients, gastroenteritis, and septicemia. Treatment includes ampicillin.
History and Physical
It is important to identify patients with sepsis and order necessary blood cultures and labs.
Physical
- Bullous impetigo
- Draining sinus tracts
- Erythema
- Fever
- Murmur if endocarditis is present
- Petechiae if toxic shock syndrome is present
- Superficial abscesses
- Warmth
Evaluation
Once a gram-positive organism infection is suspected, these laboratory studies are useful:
- CBC
- Electrolytes
- Blood cultures
- Pro-calcitonin level
- Echocardiogram if endocarditis is suspected
- Joint aspiration if a septic joint is suspected
Treatment / Management
Penicillin was the first antibiotic ever introduced during World War II by Alexander Fleming in 1928. Penicillin does not cover Staph or Enterococcus but used mainly streptococcal infections. The penicillinase-resistant organisms (nafcillin, oxacillin, cloxacillin, dicloxacillin) cover Staph (MSSA) and Strep. Anti-pseudomonal penicillins include piperacillin and ticarcillin effective against gram-positive, gram-negative, pseudomonas, and anaerobes. Carbapenems cover gram-positives, gram negatives, and anaerobes.[3][4][5]
Trimethoprim/sulfamethoxazole, clindamycin, and doxycycline are oral antibiotics used for mild to moderate MRSA infections. It is important to note that trimethoprim/sulfamethoxazole increases warfarin levels leading to increased INR. Vancomycin, linezolid, daptomycin, and tigecycline cover moderate to severe community and hospital-acquired MRSA. Vancomycin requires renal dosing with trough levels between 15 to 20. Linezolid is an option if a patient is allergic to vancomycin. CBC needs to be checked weekly to avoid bone marrow suppression, neutropenia, thrombocytopenia, and anemia. Linezolid, daptomycin, and tigecycline are options to treat vancomycin-resistant enterococci.[6][7][8]
Prognosis
The prognosis following infection with gram-positive organisms is variable. The highest mortality rates are in elderly persons who tend to have suppressed immune systems and less physiologic reserve.
Enhancing Healthcare Team Outcomes
Health professionals, including doctors, nurses, and pharmacists, need to be aware of risk factors to treat patients with selected antibiotics properly. Pharmacists need to accurately monitor vancomycin trough levels to avoid mortality in patients with Staph aureus. They also need to review medication for dose and interactions and counsel patients about finishing all prescribed antibiotics. Infection control nurses evaluate nosocomial infections and implement appropriate policies. An interprofessional approach will produce the best outcomes. [Level 5]
Outcomes: Screening for methicillin-resistant Staphylococcus aureus (MRSA) risk factors enhance infection control. MRSA risk factors include patients who are above age 65, urinary catheter, previous antibiotic treatment past three months, trauma, and those admitted from a long-term facility.[9] [Level 5]