Continuing Education Activity
The management of foreign bodies in the external auditory canal can be nuanced and, for some medical professionals, may be intimidating if not performed frequently. This activity reviews the anatomy of the external auditory canal and techniques for removing external auditory canal foreign bodies. It also highlights the interprofessional team's role in ensuring patient comfort and appropriate positioning while removing the foreign body.
Objectives:
Determine potential contraindications to removing a foreign object from the external auditory canal.
Identify objects that require emergent removal from the external auditory canal.
Assess the techniques and instruments used to remove foreign bodies from the external auditory canal.
Communicate the importance of collaboration and coordination among the interprofessional team members to facilitate safe ear foreign body removal, minimize complications, and improve patient outcomes.
Introduction
The external auditory canal (EAC) is the most common location to encounter a foreign body, particularly in children, accounting for 44% of cases, with nasal, pharyngeal, esophageal, and laryngobronchial locations representing 25%, 23%, 5%, and 2% of cases, respectively.[1][2][3] Pharyngeal foreign bodies are most common in the adult population, making up 17% of cases.[1] Many physicians who work in acute care settings, especially those who see pediatric patients, encounter foreign bodies in the external auditory canal. Depending on the specialty and location of practice, some doctors encounter this condition more frequently. This topic aims to give physicians an understanding of the problem's scope and information regarding methods for managing a foreign body in the external auditory canal.
While more common in pediatric patients, adults may also present with EAC foreign bodies, ranging from insects to hearing aid pieces and cotton balls. The most commonly removed foreign bodies include beads (most common), paper or tissue paper, and popcorn kernels.[4][5] These account for over half of the foreign bodies removed in 1 study.[5] There may also be a slight male predominance, but not all authors agree.[5][6] Certain types of foreign bodies, such as button batteries, require emergent removal. However, removal from the EAC is not emergent for most inorganic objects. However, in prolonged retention of foreign bodies, significant edema of the EAC may render removal more challenging and painful.
Anatomy and Physiology
The EAC and the outer layer of the tympanic membrane arise from the first branchial cleft. The medial two-thirds of the EAC is comprised of bone covered with stratified squamous epithelial skin, while cartilage makes up the skeleton of the outer third. The skin lining the cartilaginous portion of the EAC has hairs and modified sweat glands that secrete cerumen (earwax). Innervation of the EAC is mainly supplied by cranial nerves V3 (mandibular branch) and X via a small branch known as Arnold's nerve. Arnold's nerve is the pathway that results in coughing or gagging in some patients with instrumentation of the EAC. Cranial nerves VII and IX also contribute, but to a lesser extent; skull base lesions that involve the facial nerve may cause numbness of a portion of the EAC, and this phenomenon is known as the Hitzelberger sign.
The external auditory canal is nearly straight in children, becoming adult-sized - approximately 2.5 cm long - at about 9 years of age. The EAC assumes a gentle sigmoid contour in adults, with the cartilaginous portion angling posteriorly and superiorly and the bony portion coursing anteroinferiorly. As a result, pulling the helix posterior and superior straightens the EAC and allows for better visualization of the tympanic membrane in adults. Of significant importance for foreign body management, the EAC has 2 natural narrowings: the first narrowing is at the bony-cartilaginous junction, and the second is just lateral to the tympanic membrane.[7] Another important anatomic feature of the EAC is the potential blind spot in the tympanic sulcus caused by the oblique slope of the tympanic membrane anteroinferiorly as it nears the bulge of the temporomandibular joint.
Indications
Indications for this procedure include the presence of a foreign body in the EAC, the availability of the appropriate equipment, and the patient's cooperation (or the ability to sedate or restrain the patient safely).[8]
Contraindications
Contraindications to removing a foreign body from the external auditory canal are related to the patient's cooperativeness, location of the object in the EAC, lack of appropriate instruments for removing the foreign body, and the type of foreign body. An uncooperative patient and the inability to safely sedate an uncooperative patient are contraindications to attempting foreign body removal.
A foreign body lodged against the tympanic membrane or a foreign body that cannot be grasped easily, such as a hard, spherically shaped object, may require specialized equipment not readily available. Specific methods might also be contraindicated in certain situations. For example, irrigation would be contraindicated with a suspected tympanic membrane perforation, organic material removal, or battery removal. Irrigation may also be contraindicated if the suspected foreign body is made of a spongy material that may swell and enlarge if hydrated.[8]
Equipment
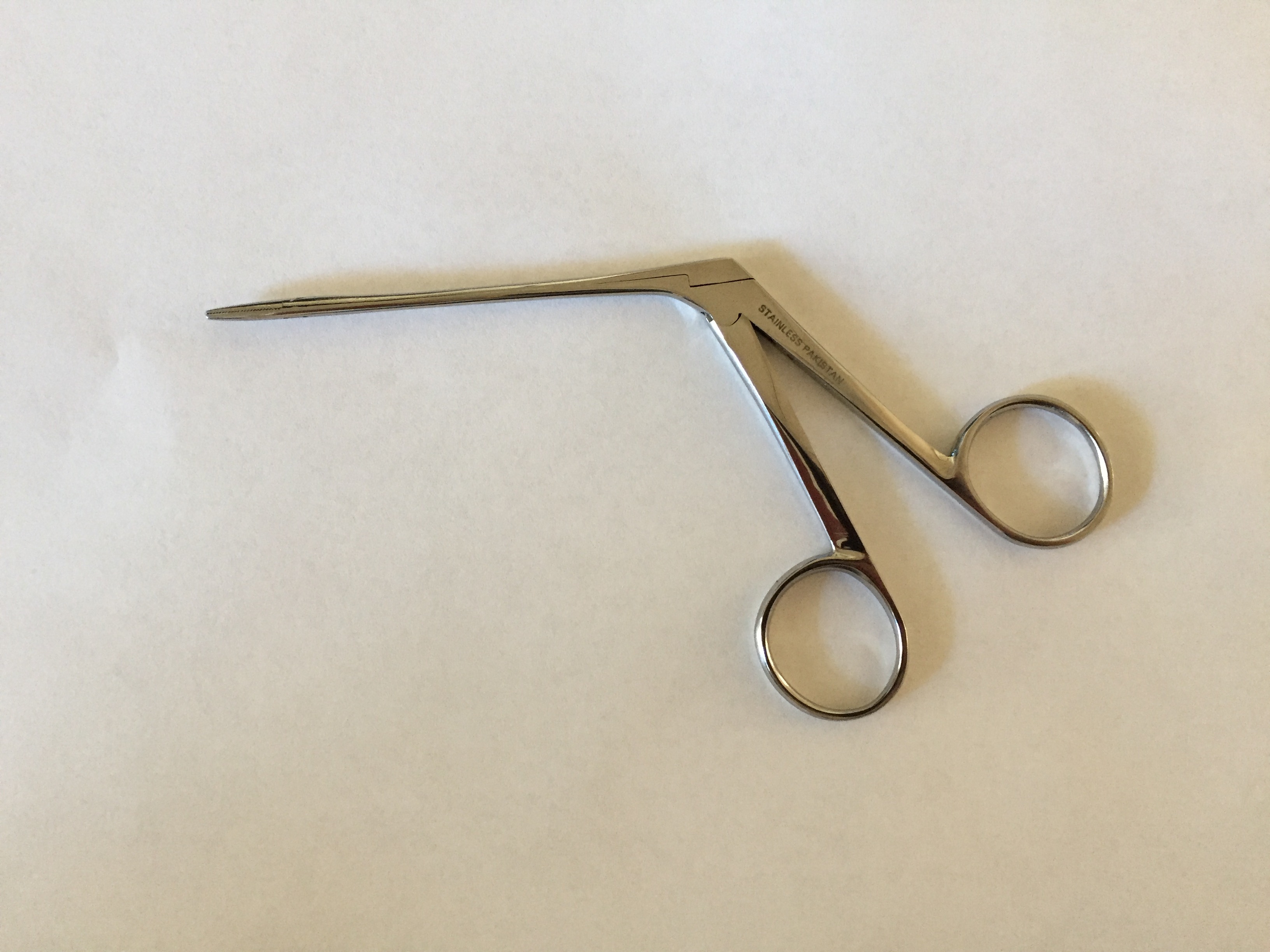
Multiple options exist for the removal of EAC foreign bodies. The type and shape of the foreign body, its location, and the patient's level of cooperation determine which piece of equipment to use.[7] Commonly used instruments include alligator forceps, cup forceps, right-angle hooks, Schuknecht foreign body suction tips, curved Rosen picks, and balloon catheters, such as a Fogarty catheter (see Image. Alligator Forceps). Binocular microscopy greatly facilitates the use of fine, sharper instruments.[7]
Irrigation is another common option, which can be performed by attaching an angiocatheter to a 20 to 30 mL syringe. Alternatively, modifying a butterfly catheter by cutting off the needle and then attaching the remaining tubing to the syringe can also be effective. Great care must be taken with blind irrigation, as an unrecognized tympanic membrane perforation may exist. Some authors advise against irrigation of the EAC unless the tympanic membrane can be visualized completely to ensure it is intact.[7]
Suction is also an option, usually performed with a Frazier tip under binocular microscopy.[7] Surgical loupes with at least 2.5x magnification and a headlight often suffice without an operating microscope. Another potential method uses cyanoacrylate (superglue) or tissue glue applied to the blunt end of a cotton-tipped applicator and then placed against the foreign body so that the glue adheres to it, and both the foreign body and applicator can be removed from the EAC together.[7][9]
Personnel
With a cooperative patient, the clinician can remove the foreign body from the EAC without assistance. Depending on how cooperative the patient is, 1 or more assistants may be required to maintain the patient in the proper position and keep the patient still. This arrangement is especially common in pediatric patients.[8][10]
Preparation
Evaluation should include noting any injury to the EAC and tympanic membrane before attempting the removal of a foreign body. The patient's hearing should also be assessed, especially if there is suspicion of tympanic membrane injury/perforation or middle ear injury once the foreign body is removed. If the patient complains of hearing loss with the foreign body in place, audiometry or tuning fork testing should be used to quantify and document the loss. Suppose a conductive hearing loss is greater than expected or a sensorineural hearing loss is encountered. In that case, the patient should be urgently referred to an otolaryngologist for evaluation and removal of the foreign body, likely in the operating room.[11]
Appropriate patient positioning is critical as well. Cooperative patients can sit or lie down with the affected ear turned towards the clinician. For younger children, there are several options for positioning. The patient can sit in the parent's lap with the parent holding the patient's body with 1 hand and the other around the head with the head turned. The patient can also lie supine or prone on the stretcher with their head turned to improve access to the EAC.[12]
Technique or Treatment
Before beginning the procedure, the physician should determine how many attempts are made (usually only 1 or 2) and, if planning more than 1 attempt, what technique should be used for the subsequent attempt. If unsuccessful after 1 or 2 attempts, further attempts should be aborted, and the patient should be referred to an otolaryngologist. Consider examining the contralateral ear and nose for other foreign bodies, particularly in children.[13] In a 2020 study, 75% of EAC foreign bodies could be removed in the outpatient setting or emergency department, with 23% requiring general anesthesia in the operating room.[14]
Specific Techniques
Manual Instrumentation (eg, forceps, curettes, angle hook)
These instruments are typically used in conjunction with the operating head of an otoscope but can also be used with the diagnostic head. Binocular microscopy is ideal, though it may not be available in all settings; likewise, otologic endoscopes can be very helpful in trained hands.[10] Retract the pinna to visualize the object in the EAC. When using forceps, the foreign body can be grasped and removed. Both curettes and right-angle hooks should be gently maneuvered behind the foreign body and rotated so the end is behind it to scoop out the foreign body.[7] In the case of a button battery or other metallic object, the use of a telescoping magnet-tipped rod, such as a mechanic might use for retrieving dropped screws, has been described to facilitate removal of the foreign body from the EAC.[15] It is essential to avoid touching the skin of the EAC with the instrument to the greatest extent possible, particularly close to the tympanic membrane, because that skin is especially sensitive, as is the tympanic membrane itself. Using an otologic speculum improves exposure and lighting; it is typically held with the non-dominant hand while the dominant hand manipulates the primary instrument.
Irrigation
This can be performed with either an angiocatheter or a section of tubing from a butterfly catheter. Using body-temperature water, retract the pinna and squirt water superiorly in the external auditory canal behind the foreign body, which then be washed out of the canal.[7] Using water that is too hot or too cold can potentially cause vertigo, nausea, and vomiting due to vestibular stimulation.
Suction
This should be performed with a suction-tipped catheter with a thumb-controlled release valve, such as a Frazier suction tip or a Schuknecht foreign body suction tip. Insert the suction tip against the foreign body under direct visualization, occlude the thumb hole, remove the object, and maintain suction until the foreign body is completely out of the EAC.[7]
Cyanoacrylate
Apply a small amount of cyanoacrylate or skin glue to the cotton end of a cotton-tipped applicator; it may help remove some of the cotton to diminish the tip size and improve visualization before application of the adhesive and insertion into the EAC. Once the glue is tacky, insert the applicator into the EAC and place the sticky end against the foreign body under direct visualization, holding it in place until the glue dries. Once the object is secured onto the applicator, it can be removed together with the applicator.[7] Avoid touching the skin of the EAC while inserting the cotton-tipped applicator, lest it adheres to the EAC rather than the foreign body and causes more injury and edema.
Arthropod Removal
The first step is to kill the arthropod, often a cockroach or a tick, allowing the patient to feel more comfortable and permit easier animal removal; multiple agents accomplish this. Studies indicate that mineral oil is the most effective, followed by lidocaine.[16] Both can be instilled into the EAC and once the arthropod is neutralized, it can be removed using any of the above methods. In practice, lidocaine offers the advantage of anesthetizing the EAC so that as the animal struggles, the patient is not bothered by any scratching of the sensitive skin.[7]
Complications
The most common complications from foreign bodies in the EAC and attempts to remove them include excoriations and lacerations of the EAC skin. As a result, it is important to document a pre-removal and post-removal examination, noting the presence of any pre-removal injuries. The EAC skin typically heals rapidly if kept clean and dry. Antibiotic eardrops can be considered as well. Less frequent and more serious foreign body removal complications include tympanic membrane perforation or ossicular chain damage.[17] These are potentially devastating and should be avoided at all costs. If the clinician is unable to or uncomfortable with removing EAC foreign bodies, the patient should be referred to an otolaryngologist.[12]
Clinical Significance
Physicians involved in acute patient care can expect to manage patients with EAC foreign bodies at some point in their careers. As such, it is crucial to recognize clinician skill and equipment limitations. The type and location of the object in the EAC, along with the patient's ability to cooperate, are the key factors in determining whether an attempt at removal should be made. Referral to a specialist or a location where sedation can be performed is recommended if the initial evaluation indicates that removal is impractical. In general, complications tend to be minor and easily managed.
Enhancing Healthcare Team Outcomes
Successful removal of an ear foreign body requires a cooperative patient and may require the assistance of family and other medical team members. Patient positioning and a well-thought-out plan are keys to the procedure's success. Explaining to patients and families what happened and securing their cooperation is important. Involving family members or staff members for positioning can also be very helpful. Another consideration is the use of medications for anxiolysis or procedural sedation to facilitate patient cooperation. This requires appropriate ancillary staff, such as nursing for intravenous line placement and medication administration, and potentially anesthesia or respiratory therapy to assist in airway monitoring. With appropriate team coordination, EAC foreign body removal can be performed safely and rapidly with a low risk for complications and minimal stress for the patient. All members of the interprofessional team, most notably clinicians, should be able to identify the problem, assist experienced hands in foreign body removal, and know when to refer the patient in more complicated cases; this results in better patient outcomes.