Introduction
The extensor hallucis longus (EHL) muscle is 1 of 4 muscles in the lower limb's anterior compartment.[1] The 3 other muscles in this region are the tibialis anterior, extensor digitorum longus (EDL), and fibularis tertius. The anterior compartment is innervated by the deep fibular nerve and receives blood from the anterior tibial artery. Muscles in this compartment dorsiflex the ankle and extend the toes. The EHL specifically extends the hallux (big toe), dorsiflexes the foot at the ankle, and inverts the foot. Several conditions can affect the EHL, including foot drop from nerve injury, tendonitis, tendon rupture, and anterior compartment syndrome.
Structure and Function
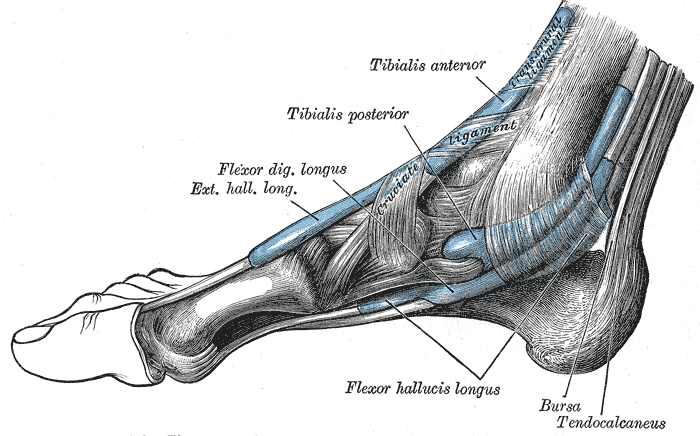
The EHL arises from the middle half of the anterior fibular surface and the adjacent interosseous membrane, then inserts at the base of the hallux's distal phalanx at the dorsal central aspect. (see Image. Extensor Hallucis Longus). The muscle lies between the tibialis anterior and EDL in the anterior leg compartment, coursing inferiorly and medially to its insertion point. The anterior tibial artery and vein and deep peroneal nerve run between the EHL and tibialis anterior. The EHL's muscle fibers course inferiorly and medially, ending in a tendon that passes under the inferior extensor retinaculum. This tendon prevents the muscle from bowstringing or subluxation.[2]
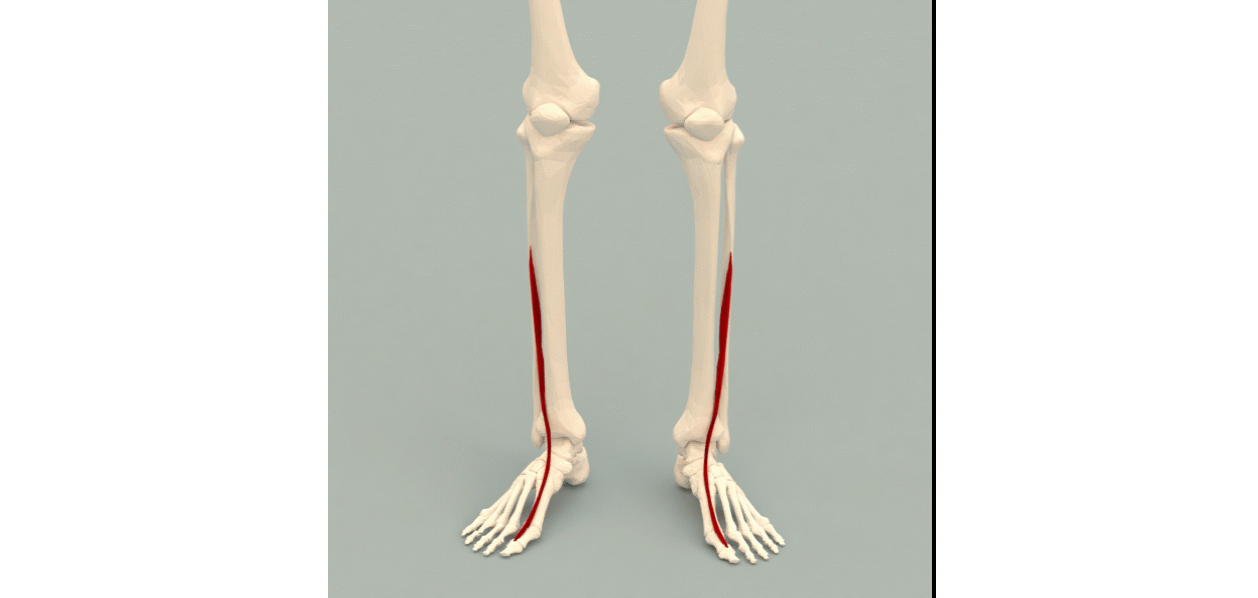
The EHL's principal function is to extend the hallux and dorsiflex the foot at the ankle. With its origin at the fibula—the lateral bone of the anterior leg—and insertion at the distal phalanx of the hallux, muscle contraction lifts the foot and big toe toward the shin (see Image. Extrinsic Foot Muscles). This movement is critical to gait because it allows foot clearance off the ground during the swing phase. Injuries to the deep peroneal nerve, the nerve that innervates the EHL, can result in foot drop. The condition manifests with weakened dorsiflexion and a characteristic high-stepping gait.[3]
The EHL's insertion on the distal phalanx of the hallux also allows it to invert the foot weakly. Injuries to this muscle may slightly weaken foot inversion. However, the condition may not be apparent as the tibialis anterior can compensate for the change.
Embryology
The embryo's limb buds begin to form about 5 weeks after fertilization. At this point, the mesoderm migrates into the limb bud and forms posterior and anterior condensations that eventually become the lower limb's muscular and skeletal components. The posterior condensation will develop into the extensor and abductor muscles of the lower limb. The anterior condensation will form the lower limb's flexor and adductor muscles.[4][5][6]
Regulators of embryonic lower limb muscle development include retinoic acid, the sonic hedgehog (SHH) gene, homeobox (HOX) genes, the apical ectodermal ridge (AER), and the zone of polarizing activity (ZPA). Retinoic acid is a global organizing gradient that initiates the production of transcription factors dictating regional differentiation and limb polarization. The AER produces fibroblast growth factor (FGF), promoting limb bud growth by stimulating mitosis. The FGF type involved in hindlimb development is FGF10, which is stimulated by T-box transcription factor 4.
The ZPA produces SHH, promoting the orientation of the limb bud along the anterior-posterior axis. SHH activates specific HOX genes— HOXD9, HOXD10, HOXD11, HOXD12, and HOXD13—important in limb polarization and regional specification. These genes control patterning and, consequently, the morphology of the developing limb in the human embryo. Errors in HOX gene expression can lead to limb malformations.[7]
Blood Supply and Lymphatics
The muscular branches of the anterior tibial artery supply blood to the EHL. The anterior tibial artery arises from the popliteal artery, which can be traced back to the superficial femoral artery, common femoral artery, and external iliac artery. The superficial femoral artery becomes the popliteal artery as it passes through the adductor hiatus into the popliteal fossa. The popliteal artery then divides toward the distal end of the popliteal fossa into the anterior and posterior tibial arteries. The anterior tibial artery passes from the posterior popliteal fossa to the anterior leg through the interosseous membrane between the tibia and fibula. The anterior tibial artery continues distally to the anterior leg compartment to supply the muscles in this area, including the EHL, before terminating as the dorsalis pedis artery on the foot dorsum.
The lower limb's lymphatic vessels divide into the superficial and deep vessels. The superficial vessels further subdivide into the medial group, which follows the greater saphenous vein, and the lateral group, which follows the small saphenous vein. The deep lymph vessels include the anterior and posterior tibial and peroneal lymph vessels. These vessels follow the course of their corresponding arteries and veins. The lymph vessels of the lower limb drain into the popliteal lymph nodes. From there, the lymph vessels ascend to the superficial inguinal, deep inguinal, external iliac, and lumbar or aortic lymph nodes.
Nerves
The deep peroneal nerve innervates the EHL. The deep peroneal nerve is a terminal branch of the common peroneal nerve, which originates from the sciatic nerve. The sciatic nerve branches into the tibial and common peroneal nerves at the popliteal fossa's apex. The tibial nerve continues its downward course posterior to the tibia, supplying the deep muscles of the posterior leg compartment. The tibial nerve terminates by dividing into 2 sensory branches, the medial and lateral plantar nerves. The common peroneal artery follows the medial border of the biceps femoris, running inferolaterally and continuing over the head of the gastrocnemius.
The common peroneal nerve wraps around the fibular neck, passing between the fibularis longus attachments to supply the lateral leg compartment. The common peroneal nerve then divides into the superficial and deep peroneal nerves. The superficial peroneal nerve supplies the lateral leg compartment. The deep peroneal nerve supplies the anterior leg compartment, including the EHL. Nerve roots from L4 to S1 contribute to the deep peroneal nerve. Injuries to this nerve can produce a foot drop and a characteristic high-step gait.
Physiologic Variants
EHL anatomic variations arise from differences in the muscle's insertion patterns. These physiologic variants are clinically significant because the EHL can be used in tendon transfer surgeries to correct conditions such as hallux varus, talipes equinovarus, and cavus foot-associated clawed hallux.[8]
The 3 most common insertion patterns for the EHL are the following:[9]
- Pattern 1 (65%): the muscle has a single tendinous insertion dorsal to the base of the big toe's distal phalanx
- Pattern 2 (26.7%): the muscle terminates in 2 tendons
- Pattern 3 (8.3%): the muscle terminates in 3 tendinous slips
Knowledge of these EHL variants is crucial in preventing iatrogenic injuries during tendon transfer surgery.
Surgical Considerations
Tendon Transfer Surgery
Trauma can damage the EHL tendon. The patient may present with a dropped hallux, loss of dorsiflexion, and abnormal gait. Surgical repair entails transferring the EDL and extensor hallucis brevis tendons to the damaged EHL tendon. The EHL tendon itself can also be used in tendon transfer surgery to correct conditions like hallux varus and talipes equinovarus.[10]
Anterior Compartment Syndrome
The anterior leg compartment is the site most frequently affected by acute compartment syndrome. Anterior compartment syndrome affects the anterior leg region.[11] Elevated pressure in this area compromises tissue perfusion and may produce irreversible muscle and nerve damage. The most common causes of anterior compartment syndrome are trauma, tight casts or dressings, IV infusion extravasation, burns, post-ischemic swelling, bleeding disorders, and arterial injury.[12]
Prompt recognition of compartment syndrome is vital to preventing limb loss and disability. Patients with anterior compartment syndrome often have pain out of proportion to the clinical findings. Other signs of this condition include pain on palpation of the muscles involved, pain on passive muscle stretching, and firmness of the anterior compartment. Pain on passive muscle stretching is the most sensitive finding before the onset of ischemia.[13] Compartment syndrome primarily affects the venous system; thus, arterial pulses are usually intact. Weak dorsiflexion is another pertinent finding in anterior compartment syndrome.
Compartmental pressure determination aids in the definitive diagnosis of anterior compartment syndrome. A resting compartment pressure greater than 30 mm Hg confirms the diagnosis. Acute compartment syndrome is time-sensitive. Complete recovery can be expected if the condition is treated within 6 hours of ischemia onset. Necrosis and limb loss are likely if compartment syndrome is not managed within that period. Subcutaneous fasciotomy is the definitive management of this condition.[14]
Clinical Significance
Physical Examination of the EHL
Physical examination of the anterior leg compartment should assess the range of motion and motor strength of the ankle and big toe. Motor weakness may indicate damage to the nerve or muscles of the anterior leg compartment. Waak ankle dorsiflexion and big toe extension are consistent with EHL neuromuscular pathology.
EHL Tendon Injuries
Most documented cases of EHL tendon injuries are due to lacerations. However, an atraumatic EHL tendon tear has been reported in a patient without prior medical problems.[15] Such a condition may occur in the setting of diabetes mellitus, osteophytic growth, local steroid injections, and obesity.[17]
EHL tendonitis may occur when the tendon becomes overstressed, resulting in inflammation and pain. Factors that commonly cause tendonitis in the lower limb extensor muscles include excessive calf muscle tightness, overexertion during exercise, and falling off the foot arch.[16] Mild extensor tendonitis may be treated with stretching and nonsteroidal anti-inflammatory drugs. A walking boot may be combined with stretching and anti-inflammatory drug therapy to relieve severe EHL tendonitis.