Continuing Education Activity
Duloxetine is a medication used to manage major depressive disorder (MDD), generalized anxiety disorder (GAD), fibromyalgia, diabetic peripheral neuropathy, and chronic musculoskeletal pain. Off-label uses for duloxetine include chemotherapy-induced peripheral neuropathy and stress urinary incontinence. It is in the Serotonin and norepinephrine reuptake inhibitors (SNRIs) class of medications. This activity describes the indications, mechanism of action, and contraindications for duloxetine as a valuable agent in treating multiple health conditions. This activity will highlight the mechanism of action, adverse event profile, and other key factors (e.g., off-label uses, dosing, pharmacodynamics, pharmacokinetics, monitoring, relevant drug-drug interactions) pertinent for members of the interprofessional team in the treatment of patients with major depressive disorder (MDD), generalized anxiety disorder (GAD), fibromyalgia, diabetic peripheral neuropathy, chronic musculoskeletal pain, and related conditions.
Objectives:
- Identify the indications for the use of duloxetine.
- Describe the most common potential adverse events associated with duloxetine therapy.
- Explain the importance of monitoring for patients on duloxetine therapy and summarize key patient counseling points.
- Explain how the successful initiation and maintenance of effective therapy with duloxetine requires a well-coordinated interprofessional team approach.
Indications
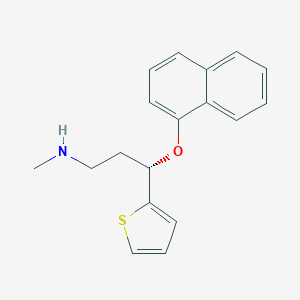
Duloxetine hydrochloride is a serotonin and norepinephrine reuptake inhibitor (SNRI), first patented in 1990 and marketed in the United States in 2004. It is FDA-approved for use in the treatment of major depressive disorder, generalized anxiety disorder, fibromyalgia, chronic musculoskeletal pain, and diabetic peripheral neuropathy. Off-label (non-FDA approved) use for duloxetine includes chemotherapy-induced peripheral neuropathy and stress urinary incontinence in both men and women.[1]
In addition to its general SNRI properties, duloxetine also increases dopamine levels, specifically in the prefrontal cortex. Due to the involvement of the prefrontal cortex in depression, the actions of duloxetine in this region also contribute to its efficacy in the treatment of depression. However, the mechanism of action does not involve the inhibition of dopamine transporters.[2]
Mechanism of Action
Duloxetine inhibits serotonin and norepinephrine reuptake, thus combining two therapeutic mechanisms in one agent to treat depression and anxiety. As well, duloxetine enhances dopamine levels within the prefrontal cortex. The mechanism of action behind the increase in dopamine levels involves the inhibition of norepinephrine transporters. These transporters have a significant affinity for dopamine, resulting in the transporter’s ability to act on both dopamine and norepinephrine. Therefore, inhibition of norepinephrine transporters can lead to an increase in dopamine. This increase in dopamine specifically occurs in the prefrontal cortex, where dopamine transporters are scarce, and reuptake relies more heavily on norepinephrine transporters.[3]
Duloxetine works to treat various neuropathic and chronic pain states by increasing the activity of noradrenergic and serotonergic neurons in the descending spinal pathway on the dorsal horn. These descending neurons inhibit the activity of dorsal horn neurons, suppressing excessive input from reaching the brain. The hypothesis is that a deficiency in these inhibitory signals results in excess input reaching the brain, which gets perceived as pain.[4]
Of note, duloxetine has no significant activity for muscarinic, cholinergic, alpha2-adrenergic, or H1 histaminergic receptors.
Administration
Duloxetine is most commonly administered in a capsule form due to good absorption via the oral route, and administration can be with or without food. Duloxetine should not be crushed or chewed. However, studies have shown that duloxetine may remain stable up to 2 hours after being opened and sprinkled on apple juice or apple sauce.
Management of fibromyalgia: 30 mg once daily can be given for one week, then the dose may be increased to 60 mg once daily. A titration approach may also be utilized starting with 20 mg daily, then increasing the dose by 20 mg every week, up to 60 mg, as tolerated. Maximum dose: 60 mg/day.[5]
Treatment of generalized anxiety disorder (GAD): 60mg can be administered initially, however depending on patient tolerance, 30 mg may be given once daily for one week, then the dose may be increased to 60mg once daily. Though studies have shown no additional benefit to doses above 60 mg/day, some experts have reported benefits when increasing doses over 60 mg/day.
Treatment of unipolar major depressive disorder (MDD): 40 to 60 mg/day can be given in a single or two divided doses. It may be necessary to start at 30mg/day for one week, and then the dose may be increased to 60 mg/day. Maintenance: 60 mg/day. Though studies have shown no additional benefit to doses above 60 mg/day, some experts have reported benefits when increasing doses over 60 mg/day.
Management of pain associated with diabetic peripheral neuropathy: 60 mg can be administered initially; however, lower starting doses may be appropriate depending on patient tolerance. Maximum dose: 60 mg/day.
Management of chronic musculoskeletal pain:
Low back pain: 30 mg can be given once daily for one week and increased up to 60 mg once daily as tolerated as an adjunct therapy. Maximum dose: 60 mg/day.
Knee pain: 30 mg can be given once daily for one week and increased up to 60 mg once daily as tolerated as an adjunct therapy.[6]
Adverse Effects
Duloxetine has a very low anticholinergic side effect profile; adverse effects of the cardiovascular, gastrointestinal, central nervous system, such as headaches and drowsiness, and fatigue, are more common.[1][6]
Serious adverse effects of duloxetine include:
- Suicidality
- Serotonin syndrome
- Hepatoxicity
- Mania
- Syncope
- Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
- Hyponatremia
Common adverse effects of duloxetine include:
- Headache
- Drowsiness
- Fatigue
- Nausea
- Xerostomia
- Abdominal pain
- Weight loss
- Weakness
- Insomnia
- Dizziness
- Chane in libido
- Diaphoresis
- Constipation
- Decreased appetite
- Tremor
- Diarrhea
- Erectile dysfunction[1][6]
Contraindications
Duloxetine is contraindicated in patients with concurrent or recent (within two weeks) therapy with monoamine oxidase (MAO) inhibitors, uncontrolled angle-closure glaucoma, or hypersensitivity to duloxetine. Duloxetine should also be avoided in patients with liver failure or severe renal dysfunction. Clinicians should also avoid using duloxetine in patients receiving treatment with linezolid or intravenous methylene blue due to an increased risk of serotonin syndrome.[1]
Precautions and Warning in Special Population
Pregnant Patients
Duloxetine is FDA pregnancy category C, which means risk to fetal development cannot be ruled out. In animal reproductive studies, duloxetine demonstrated adverse effects on embryo/fetal development. Therefore, the clinician should only prescribe duloxetine if the potential benefits justify the potential risk to the fetus.
Breastfeeding Women
Duloxetine is excreted in breast milk and may produce effects in the nursing infant. Some studies show the relative infant dose (RID) of duloxetine to be 2.3%. RID is the dose received via breast milk relative to the mother’s dose. A RID below 10% is acceptable when breastfeeding. Some sources recommend breastfeeding only if the RID is less than 5% if the mother is on psychotropic medication. Regardless, an infant breastfed by a mother receiving duloxetine requires monitoring for behavior changes, sleep disturbance, feeding changes, growth, and neurodevelopment.[7]
Elderly
SSRIs and SNRIs have correlations with several cases of clinically significant hyponatremia in elderly adults. Caution is necessary when prescribing duloxetine in the geriatric population. However, dosage adjustment based on the age of the patient is not required.[8]
Monitoring
Clinicians should check blood pressure and vitals before initiating therapy and routinely after that. Monitor for changes in suicidal ideation, especially when starting treatment, altering the dose, and after discontinuation of therapy. Monitor for worsening depression, behavioral changes such as mania, and withdrawal symptoms from abrupt discontinuation. Patients should be monitored for abnormal bleeding as duloxetine may impair platelet aggregation. Caution should be exercised when using anticoagulants or antiplatelet medications along with duloxetine therapy. Laboratory workup should include monitoring serum creatinine, blood urea nitrogen(BUN), transaminase levels, blood glucose levels, and HgbA1c in diabetic patients. Sodium levels require follow-up when prescribing duloxetine in the geriatric population.[1]
Toxicity
Fatal outcomes have occurred with overdoses at as low as 1000 mg. Signs and symptoms of overdose include serotonin syndrome, seizures, coma, somnolence, syncope, tachycardia, autonomic instability, diarrhea, and vomiting. Signs of serotonin syndrome include agitation, restlessness, disorientation, diaphoresis, hyperthermia, tachycardia, nausea, vomiting, tremor, muscle rigidity, hyperreflexia, myoclonus, dilated pupils, dry mucous membranes, and increased bowel sounds. Clonus and hyperreflexia are particularly common in serotonin syndrome.
There is no antidote to duloxetine overdose. If the patient is presenting with serotonin syndrome, cyproheptadine and cooling measures may be considered. Patients with abnormal vital signs need monitoring, and severe cases may warrant ICU-level of care.[9][10]
Enhancing Healthcare Team Outcomes
Antidepressants including duloxetine may increase the risk of suicidal thinking and behavior in children, adolescents, and young adults who have a major depressive disorder and other psychiatric disorders. Close observation and routine follow-up by the healthcare team is essential in ensuring medication compliance and patient safety.
When a patient is started on duloxetine therapy, all the interprofessional team members, including clinicians, mid-level practitioners, specialists, nurses, social workers, and pharmacists, should be involved in patient care. The pharmacist should perform a thorough medication reconciliation to preclude any drug interactions and verify that dosing is appropriate. A psychiatric health specialist nurse will assist with patient counseling regarding administration and monitor the patient on follow-up visits. If there are any warning symptoms or concerns, the pharmacist and nurse should inform the prescriber promptly. Any social workers or other mental health counselors also need to be included in the sharing of information. This type of interprofessional team approach can ensure optimal patient outcomes with minimal adverse events.