Continuing Education Activity
Toxoplasmosis is a parasitic infection in humans and animals. Infection in healthy immunocompetent adults is asymptomatic in about 50% of the cases. However, it can also cause a self-limited mild, nonspecific illness presenting with signs and symptoms such as fever, malaise, maculopapular rash, headache, fatigue, and tender lymphadenopathy. In immunocompromised individuals and neonates, it causes a severe infection with devastating sequelae. This activity reviews the identification, evaluation, and management of congenital toxoplasmosis and explains the role of the interprofessional team in managing and improving care for patients with this condition.
Objectives:
Identify the risk factors for acquiring congenital toxoplasmosis and understand its pathophysiology.
Evaluate the common physical exam findings associated with congenital toxoplasmosis.
Determine the risks and benefits associated with the antiparasitic regimen and summarize key patient counseling points.
Communicate the importance of improving care coordination amongst interprofessional team members to improve outcomes for patients affected by congenital toxoplasmosis.
Introduction
Toxoplasmosis is a parasitic infection in humans and animals. Infection in healthy immunocompetent adults is asymptomatic in about 50% of the cases. However, it can also cause a self-limited mild, nonspecific illness presenting with signs and symptoms such as fever, malaise, maculopapular rash, headache, fatigue, and tender lymphadenopathy. In immunocompromised individuals and neonates, it causes a severe infection with devastating sequelae. Congenital toxoplasmosis, as a result of vertical transmission from infected mothers, is a significant cause of morbidity and mortality in fetuses, neonates, and children as they progress into adulthood. Since asymptomatic infection is more common, a high index of suspicion is necessary, and diagnosis can be made readily by serologic testing.
Etiology
Congenital toxoplasmosis results from a protozoan, an obligate ubiquitous intracellular parasite, Toxoplasma gondii (T. gondii).
Life cycle
The definitive hosts of T. gondii are cats with a wide range of intermediate hosts. In cats, it can have 2 cycles, intestinal and extraintestinal, whereas, in other hosts, it has only an extraintestinal phase. The life cycle of T. gondii has 3 infectious stages: tachyzoite, bradyzoite, and oocysts or sporozoites. Bradyzoites and tachyzoites are slow and fast multiplying phases in the host's tissues, mainly the brain and muscle. Oocysts form from the sexual cycle of the organism in the cat’s intestine. Cats typically get infected by consuming infected animals containing bradyzoites or contaminated soil or water containing oocysts. The parasite replicates in the gut of the cat to produce oocysts.
In this acute phase of intestinal infection, the cat sheds millions of oocysts in their feces for about 1 to 2 weeks. These oocysts sporulate under ideal humid environmental conditions and contaminate the soil, grass, and garden vegetables. It usually takes 2 to 3 days in temperate climates and longer in colder climates. Thus, if the cat litter gets disposed of within 1 to 2 days, the risk of infection is decreased. Intermediate hosts such as humans, sheep, cattle, pigs, birds, and mice acquire the infection in this phase. These oocysts differentiate into tachyzoites, which are characteristic of acute infection. The transformation into oocysts (sexual cycle) occurs only in cats. Over time, they get deposited in the tissues as cysts (bradyzoites) in the intermediate hosts. Bradyzoites are responsible for latent infection and persist in the brain, myocardium, skeletal muscle, and other organs for life.
Transmission
Pregnant women develop toxoplasmosis via 2 routes:
- Primary maternal infection due to the ingestion of undercooked meat or oocyst-contaminated food or water
- Reactivation of latent infection in severely immunocompromised states such as co-infection with human immunodeficiency virus
The organisms are transmitted transplacentally to the growing fetus. The incubation period is 4 to 21 days in acquired infections. The exact timing of when the transmission occurs is not well documented. The severity of the clinical manifestations in the fetus and the newborn depends on the gestational age at which the infection occurs, parasitic load, the virulence of the infective strain, and the maternal immune status.[1]
Epidemiology
The number of men, women, and children in the United States carrying the toxoplasma parasite exceeds 40 million, but most are asymptomatic. Worldwide, more than 60% of some populations are infected with toxoplasma. Seroprevalence is variable between different regions, being more prevalent in tropical areas. Toxoplasmosis is considered to be the most common parasitic infection in humans. Seropositivity increases with age in all geographical areas. The infection rates are often higher in regions with hot, humid climates and lower altitudes because oocysts grow faster and survive better in such an environment. The incidence of congenital toxoplasmosis depends upon the acquisition time of toxoplasma infection in pregnant women and their prior infection state at the time of exposure. Congenital cytomegalovirus (CMV) is the only transplacentally acquired infection more common than congenital toxoplasmosis. In the United States, congenital toxoplasma infection rates among live-born newborns are from 1 in 3000 to 1 in 10,000.[2]
History and Physical
Congenital toxoplasmosis has wide-ranging clinical manifestations from being completely asymptomatic at birth to severe neurological and ocular disease. The majority of the infants (about 75%) with congenital toxoplasmosis have no apparent clinical manifestations at birth. Identification usually takes place during routine newborn and maternal screening done in certain countries. They demonstrate neurological (cerebral calcifications) or ophthalmologic (retinal scars) abnormalities. In a limited percentage of patients, it can lead to spontaneous abortion, premature or stillbirth.
Term newborns usually present with a milder form of the disease with symptoms such as hepatosplenomegaly and lymphadenopathy. In comparison, preterm newborns exhibit severe symptoms. The classic triad of chorioretinitis, hydrocephalus, and cerebral calcifications presents in a limited number of infected newborns. The symptoms are generally severe and clinically apparent when the mother acquires the infection in the first trimester and receives no treatment. Some severely affected may die in utero or a few days after birth. The signs and symptoms of severe disease include:
- Neurological manifestations (eg, micro- or macrocephaly, seizures, nystagmus, hydrocephalus, cerebral calcifications, meningoencephalitis) [3]
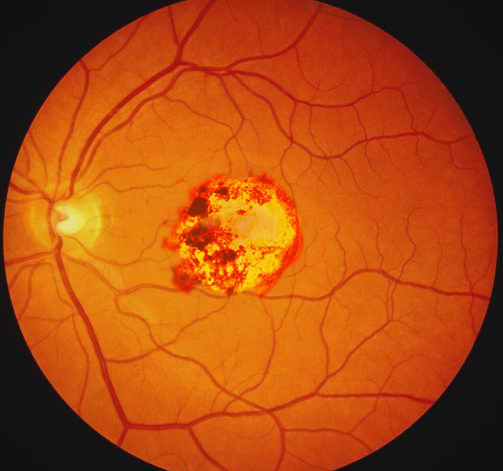
- Ophthalmologic manifestations (eg, chorioretinitis, microphthalmia, retinochoroiditis, strabismus)
- Small for gestational age
- Hepatosplenomegaly
- Generalized lymphadenopathy
- Jaundice
- Thrombocytopenia, anemia, petechiae
- Maculopapular rash
Infants with mild or subclinical infection are at risk for late sequelae such as:
- Recurring chorioretinitis resulting in vision loss
- Motor delays
- Learning disorders
- Intellectual disability
- Hearing loss
- Endocrine abnormalities due to disruption of the hypothalamus and pituitary gland
At present, newborn screening for congenital toxoplasmosis is performed only in Massachusetts and New Hampshire.[4]
Evaluation
Testing for congenital toxoplasmosis in the fetus should take place when the mother has confirmed infection or there are suggestive sonographic findings such as intracranial calcifications or cerebral ventricular dilation. Positive polymerase chain reaction (PCR) for T. gondii DNA in the amniotic fluid confirms the diagnosis in the fetus.
Congenital toxoplasmosis should be suspected in the newborns in the following situations:
- Primary maternal infection with T. gondii during pregnancy
- Immunocompromised mothers with prior T. gondii infection
- Newborns with clinical features indicative of congenital toxoplasmosis
- Newborns with positive newborn screening for toxoplasma
The diagnosis results from a combination of clinical and laboratory findings.
Serological tests
toxoplasma-specific antibodies (immunoglobulin [Ig]G, IgM, and IgA) require testing in all cases of suspected infection. The half-life of toxoplasma IgM and IgA antibodies is 5 and 10 days. When there is a concern for false positives due to maternal contamination of fetal blood during labor, repeat serological testing should be done 10 days after birth. T. gondii DNA by PCR is also possible in cerebral spinal fluid (CSF), urine, or peripheral blood.[5]
The diagnostic criteria for confirmed infection are one of the following:
- Presence of toxoplasma-specific IgM or IgA antibodies 10 days after birth
- Persistent or increasing IgG titer without treatment in infants at or beyond 1 year of age
- Positive PCR for T. gondii DNA or positive toxoplasma IgM or Ig A antibodies in the CSF
Positive IgG is indicative of prior or current maternal infection. In the presence of other suggestive features but negative IgM and IgA antibodies, toxoplasma IgG testing requires repetition every 4 to 6 weeks until complete disappearance. Negative IgM and IgA antibodies do not exclude the infection. If the mother is affected later in her pregnancy, there is a delay in the production of antibodies in the newborn. When an infection is suspected, the antibodies should be repeated every 2 to 4 weeks until at least 3 months of age.
Because the interpretation of these serologic tests is complex, they should be sent to the National Reference Laboratory for Toxoplasmosis (Palo Alto, CA) or the Toxoplasmosis Center (Chicago, IL) for confirmation.
Imaging
The main findings on cranial sonography or computed tomography of the head include diffuse intracranial periventricular calcifications, brain atrophy, or hydrocephalus.
Other tests
CSF will be abnormal, with high protein levels (>1 gm/dl) and mild elevation of white blood cells with monocyte predominance. A complete blood count may demonstrate anemia or thrombocytopenia. Hepatic and renal function tests can be done as a baseline to look for other signs of systemic involvement.
Treatment / Management
Despite being over a hundred years since the discovery of T. gondii, researchers have not been able to establish a standardized regimen for the treatment of congenital toxoplasmosis. There are numerous opinions regarding the drug regimens and the duration of the treatment.[6]
Most medications work against the actively dividing tachyzoites and do not work against encysted bradyzoites. The most commonly used treatment regimen in confirmed and probable cases of congenital toxoplasmosis is a combination of pyrimethamine, a sulphonamide (sulphadiazine or sulphadoxine), and folinic acid for 1 year.[7] Higher doses and longer duration (2 years) are recommended when the presentation is severe, with over three intracerebral calcifications and/or more than one ocular sign or severe abnormalities at birth. Newer drugs known to have activity against T. gondii are azithromycin and atovaquone. However, more research is needed to determine its efficacy. If diagnosed prenatally, the mother should be treated immediately before the delivery. Spiramycin is recommended for mothers with acute toxoplasma infection to prevent transplacental transmission.[8]
Asymptomatic infants with positive serology or newborn screening receive treatment for 3 months. Some experts recommend adding steroids to this regimen when the CSF protein is high or severe chorioretinitis affects vision. Steroid therapy continues until the protein in the CSF disappears or the chorioretinitis resolves. The infants must be followed with frequent neurodevelopmental, ophthalmologic, and hearing assessments to evaluate the therapy response and identify any late sequelae.
The long duration of treatment is associated with adverse medication effects such as severe bone marrow suppression resulting in neutropenia, worsening kidney function, and allergic reactions. These infants should have frequent blood count monitoring and periodic liver and renal function tests.[9]
Differential Diagnosis
Congenital toxoplasmosis requires differentiation from other congenital infections caused by:
- CMV
- Rubella
- Lymphocytic choriomeningitis virus
- Varicella
- Herpes simplex virus
Prognosis
Prenatal treatment of toxoplasmosis reduces the risk of severe presentation and late neurological sequelae. The prognosis of untreated toxoplasmosis is very poor, resulting in vision deficits, neurological deficits, and severe developmental delays.[10] The prognosis in treated patients remains an area of significant research. Some studies have demonstrated that early treatment substantially improves the ocular lesions. However, they need close ophthalmologic monitoring through early adulthood.[11] Higher gestational age correlates with better outcomes.
Complications
Complications of untreated congenital toxoplasmosis include:
- Loss of vision
- Deafness
- Intellectual disability
- Severe developmental delays
Pearls and Other Issues
Prevention
Pregnant women should be educated to prevent toxoplasmosis; counseling points include:
- Wear gloves or wash hands when handling litter boxes, and to not adopt or pet stray cats
- Avoid eating undercooked meat during pregnancy
- Peel and wash fruits and vegetables before consumption
- Avoid contact with soil or wear gloves when gardening
- Avoid drinking unfiltered water
Enhancing Healthcare Team Outcomes
The identification and management of congenital toxoplasmosis continue to be challenging. Early treatment is the cornerstone of improved morbidity. This condition is best managed by an interprofessional group of medical professionals that includes a neonatologist, neurologist, Infectious disease specialist, ophthalmologist, developmental pediatrician, primary care pediatrician, and care coordinator.
The key is prevention, and this requires an interprofessional approach. The pregnant female requires education on washing hands after touching meat products and not consuming undercooked or raw meat. Also, all fruits and vegetables require thorough washing. The female should avoid contact with cat litter and fecal material. Educational reinforcement should come from the nurses, pharmacists, obstetricians, and primary caregivers at every clinic visit. Only through such an approach can the morbidity of congenital toxoplasmosis be reduced.
Given the lack of a solid pharmaceutical approach to treatment, the pharmacist should monitor the regimen closely, checking dosing and agent selection, performing medication reconciliation, and informing the team should they encounter any issues. Nurses will be best positioned to monitor for adverse events or evaluate the effectiveness of treatment. Only through an interprofessional team approach, including physicians, specialists, specialty-trained nurses, and pharmacists, all collaborating across disciplines, can patients achieve optimal patient results.