Continuing Education Activity
Cervical subluxation is the most unstable form of cervical spine injury. This condition involves varying degrees of vertebral body slippage relative to adjacent vertebrae, often caused by ligamentous injury and jumped facets, increasing the risk of spinal cord injury. Facet dislocation occurs when the articular surfaces are not in contact, while subluxation entails reduced contact between these surfaces. Osteoligamentous destruction following bilateral facet dislocations encompasses a higher risk of neurological injury. Motor vehicular crashes and falls, which cause acceleration-deceleration injuries or direct cervical impact, are the most common causes of cervical subluxations. Provisions for early anatomical stabilization, preserving spinal cord function, implementing staged rehabilitation, promptly instituting patient care bundles to prevent secondary complications, and prioritizing patient survival, recovery, and eventual thriving are essential.
This activity for healthcare professionals is designed to enhance learners' proficiency in evaluating and managing traumatic cervical spine subluxations. Participants gain a deeper insight into the condition's signs and symptoms, appropriate diagnostic techniques, potential complications, and evidence-based treatment options. Learners become prepared to collaborate within an interprofessional team caring for patients with cervical subluxation.
Objectives:
Identify the signs and symptoms indicative of cervical subluxation.
Create a clinically appropriate diagnostic plan for a patient with suspected cervical subluxation.
Develop a personalized management strategy for an individual diagnosed with cervical subluxation.
Collaborate with all interprofessional team members, including orthopedic surgeons, neurologists, and physical therapists, to provide efficient, comprehensive, and coordinated care for patients with cervical subluxation.
Introduction
Cervical Subluxation Overview
Spinal cord injury (SCI) accounts for multispectral neurological deficit patterns and severely compromises the dichotomous utilization of health resources, especially in low- and middle-income nations. Nearly 80% of patients with this condition are males, with almost 60% aged 16 to 30. Moreover, as many as 60% of these individuals remain unemployed following such incidents.[1]
Subluxation comprises a significant proportion of traumatic cervical spinal injuries. This condition entails varying degrees of vertebral body slippage relative to adjacent vertebrae, often arising from ligamentous injury and jumped facets, increasing SCI risk. Facet dislocation occurs when the articular surfaces totally lose contact, while subluxation involves reduced contact between these surfaces.[2] Osteoligamentous damage resulting from bilateral facet dislocations often incurs a higher risk of neurological injury.[3] Allen et al coined the term "distractive flexion injuries" for facet subluxation and dislocation in 1982.
Cervical Spine Anatomy
The cervical spine comprises 7 vertebrae, each with distinct characteristics and functions. The 1st cervical vertebra, also known as the atlas or C1, lacks a vertebral body but features anterior and posterior arches with lateral masses. C1 articulates with the skull's occipital condyles, facilitating head flexion and extension.
The 2nd cervical vertebra, also known as the axis or C2, is distinguished by a prominent dens (odontoid process) projecting superiorly from the body. The dens articulates and forms a pivot joint with the atlas, enabling rotational head movement. Vertebrae C3 to C7 possess more typical vertebral bodies with spinous and transverse processes. These vertebrae provide support, stability, and flexibility to the cervical spine, allowing for various neck movements. Intervertebral disks lie between each cervical vertebral pair, consisting of a fibrous external layer (annulus fibrosus) and a gel-like inner core (nucleus pulposus). These disks provide spine cushioning, shock absorption, and flexibility.
The cervical spine has been subdivided anatomically and functionally into the following:
- The region from the occiput (C0) joint to C2, which is mostly responsible for rotational head movements
- The subaxial cervical spine region (C3-C7), which predominantly shows flexion and extension movements
The spinal cord extends from the brainstem downward, encased within the protective spinal canal formed by the vertebral bodies. The spinal cord transmits sensory and motor signals between the brain and body. The cervical spinal nerves, comprising 8 pairs labeled C1 to C8, emerge from the spinal cord's cervical region and are crucial in upper body sensory and motor functions. Each nerve exits the spinal cord through the intervertebral foramina between adjacent cervical vertebrae. Sensory fibers transmit touch, pressure, position, temperature, and pain information from the skin, muscles, joints, and other upper body regions back to the spinal cord and brain. Conversely, the motor fibers relay brain and spinal cord signals to the upper body's skeletal muscles.
Specific cervical spinal nerves have distinct roles based on their origin and distribution. For instance, the C1 nerve, known as the suboccipital nerve, innervates the suboccipital muscles at the skull base, contributing to head movement and posture. Additionally, C2 to C4 nerves contribute to the cervical plexus, giving rise to important nerves like the greater occipital (C2) and phrenic nerve (C3-C5). Spinal nerves C5 to T1 are crucial brachial plexus components that innervate upper body muscles and provide upper limb sensory function.
Vertebral arteries travel through the C1 to C6 transverse foramina and supply blood to the brain, particularly the posterior circulation, and are vulnerable to injury in cervical trauma. Various ligaments stabilize the cervical spine, including the anterior longitudinal (ALL), posterior longitudinal, interspinous, and supraspinous ligaments, ligamentum flavum, and transverse ligament of the atlas. The main cervical spine stabilizers are the tectorial, cruciate, apical, and alar ligaments. The posterior ligamentous complex, disks, and apophyseal joints prevent anteroposterior translation exceeding 3 mm.
Facet joints—synovial joints between adjacent vertebrae's articular processes—facilitate smooth movement and stability of the spine. However, these joints are susceptible to damage following an SCI.
Etiology
The most common etiologies of cervical subluxation are motor vehicular crashes and falls.[4][5] Acceleration-deceleration injuries and direct impact on the neck account for such subluxations.[6] Medical conditions that increase susceptibility to cervical subluxation include the following:
- Rheumatoid arthritis
- Down syndrome [7]
- Mucopolysaccharidoses, particularly Morquio disease [8]
- Grisel syndrome
- Cervical surgical procedures and radiation [9]
- Dystonia [10]
- Marfan syndrome [11]
Cervical subluxation has been observed in up to 50% of patients with a destructive form of rheumatoid arthritis. Connective tissue abnormalities associated with conditions like Down and Marfan syndromes increase ligamentous laxity, making the spinal region injury-prone in affected individuals.
Epidemiology
The overall prevalence of cervical spinal injury (CSI) among all trauma patients is 3.7%, occurring in 2.8% of alert individuals and 7.7% among unevaluable patients. Nearly 42% of CSIs are deemed unstable.[12] New SCI cases reported annually reach 15 to 40 per million population, with more than 50% involving the cervical spine. Half of the patients present with either unilateral or bilateral subluxations.[13][14] Facet dislocation is observed more frequently than subluxation, with 50% of such injuries occurring between the C5 and C7 regions. The number of new CSI cases reported yearly in North America is about 150,000, predominantly following motor vehicle accidents.
A study from major Australian tertiary hospitals comprising 226 patients between 2003 and 2013 reported that cervical subluxation's median age of involvement was 40 years, with 56.2% of the cohorts sustaining unilateral or bilateral facet dislocations. The male-to-female ratio in traumatic cervical spinal cord injury was 4.0:1, with almost 90% of affected individuals being manual laborers.[15] High-velocity motor-vehicle collisions were predominant in younger cohorts. In contrast, low-velocity falls contributed more to similar injuries in older adults. The region most frequently involved was C6 to C7, comprising 38.5% of cases. Tetraplegia was present in 87% of cervical subluxations. Concomitant facet fracture was observed in almost 60%. Almost 81.3% presented with an ASIA grade A or B neurological status (see Physical Examination), with C6 to C7 and C5 to C6 levels involved in almost 70% of the cases.
Pathophysiology
The interplay of various dynamic cervical movements can lead to diverse injury patterns following cervical subluxations. The principal mechanics behind the bilateral jumped facets include hyperflexion injury, axial loading, and anterior shear.[16] The Allen and Ferguson classification system has categorized the principal loading forces as follows:
- Hyperflexion injury: Unilateral or bilateral locked facets with associated interspinous ligament injury and teardrop fracture
- Hyperextension injury: Facets and lamina fractures with posterior subluxation following ALL disruption
- Axial loading: Leads to burst fracture and damage to all ligaments [17]
Acute atlantoaxial rotatory subluxation is more common in children than adults owing to ligamentous laxity, weak neck muscles, the atlantoaxial joint's horizontal configuration, and greater head size relative to the torso.
History and Physical
History
The management of cervical subluxation begins with the primary survey, assessing the patient's airway, breathing, and circulation since most cases arise from acute trauma. Unconscious individuals without respiration and a cardiac tone must be immediately resuscitated according to the Advanced Trauma Life Support (ATLS) guidelines. The patient's neck should be immobilized with a rigid cervical collar to prevent further neurological deterioration from inadvertent neck movements during evaluation and stabilization.[18] Once the patient is stabilized, the secondary survey must be thoroughly conducted to rule out polytrauma, severe hemorrhage, and other potentially life- or limb-threatening injuries.
Individuals with cervical subluxation typically present with a history of neck trauma, often after motor vehicle crashes, falls, sports collisions, or direct neck blows. The patient may report experiencing a sudden onset of neck pain, stiffness, or discomfort following the traumatic event. Associated symptoms may include numbness, tingling, or weakness in the arms or hands, depending on the subluxation's severity and location.
Patients may also describe specific injury mechanisms, such as neck hyperextension or hyperflexion, which can predispose to vertebral misalignment. Loss of consciousness or altered mental status at the time of the injury may be elicited, which could indicate traumatic brain injury. Some people may have a history of previous neck injuries or underlying conditions predisposing to cervical instability, such as degenerative disk disease, osteoarthritis, or congenital cervical spine anomalies. Other medical information that may impact treatment decisions include allergic history, current medications, and history of immunodeficiency, diabetes mellitus, clotting problems, and neurologic, cardiac, and respiratory conditions.
Physical Examination
Many patients with cervical subluxation have associated injuries, warranting a complete physical examination. Cardiorespiratory status must be monitored continuously to determine the need for resuscitation. Extremity examination may reveal musculoskeletal injuries requiring immobilization. Wounds may be noted on the head, neck, and limbs, which may need immediate sterilization, bleeding control, or dressing for definitive surgical treatment.
The neurological assessment should be completed and documented per the American Spinal Injury Association (ASIA) grading.[19] The grading scheme is as follows:
- ASIA A: Complete motor and sensory function loss
- ASIA B: Incomplete injury with preserved sensory function but total paralysis
- ASIA C: Incomplete injury with preserved motor function below the injury level; less than 50% of muscles have Medical Research Council (MRC) grade 3
- ASIA D: Incomplete injury with preserved motor function below the injury level; at least 50% of muscles have MRC grade 3
- ASIA E: Normal motor and sensory function
Clinicians can assess the pattern and level of motor weakness to localize the lesion swiftly. Patients may present with quadriparesis, quadriplegia, or central cord syndrome. Weakness at the C5 level may manifest as difficulty in shoulder shrugging, while weakness at C6 may affect elbow flexion. A C7 injury may impact elbow extension. Evaluating the degree of areflexia, typically occurring at the level of injury, can provide further insight. Abnormal single-breath counts may indicate phrenic nerve involvement at the C3 to C5 level. Concurrent Horner syndrome may suggest injury at the C7 to T1 level. The salient clinical features in cervical subluxations include neck pain, arm rhizopathy, and myelopathy.[20]
Torticollis with neck spasm is characteristic of atlantoaxial rotatory subluxation. A cock-robin head posture develops, accompanied by sternocleidomastoid spasticity ipsilateral to the side of chin rotation. Plagiocephaly may be observed late on the side of the head tilt.
Evaluation
Initial management and resuscitation should be instituted according to the ATLS protocol. Detailed neurological documentation must be performed based on the International Standards for Neurological Classification of Spinal Cord Injury or the ASIA scoring system.
After hemodynamically stabilizing the patient, the injury level, pattern, grade, and associated ligamentous and vascular injuries are evaluated through a radiological imaging series. Canadian cervical spine or National Emergency X-Radiography Utilization Study rules guide the imaging choices. However, full spinal precautions and the log roll transfer method must be used during imaging procedures. Indications for radiographic evaluation include the following:
- Neck pain
- Neck tenderness
- Patient lacking alertness or is under the influence of alcohol or drugs
- New neurological deficits
- Distracting injuries [21]
The roles of different imaging modalities in evaluating cervical subluxation are explained below.
Plain Radiography
Plain spinal x-rays help diagnose and localize the injury. Radiography also helps rule out vertebral body and spinous process fractures. This modality may be the only imaging tool available in rural areas.
Radiographs should include lateral (flexion, neutral, and extension), anteroposterior, and open-mouth odontoid projection views. Anteroposterior and open-mouth views may show the asymmetric distance between the lateral mass and dens, whereas the lateral facet may appear wedged-shaped in lateral views. The “bow-tie” or “batwing” sign is characteristic of a unilateral jumped facet joint.[22] More than 50% overlap between the facet joints’ articulating surfaces is considered unstable.
The dynamic x-ray is critical in ruling out subtle instability in low-grade subluxations. The clinician should carefully examine subtle subluxation radiological findings, including spinous process divergence or “fanning,” anterior disk space narrowing, apophyseal joint displacement, and loss of parallelism at the apophyseal joint surfaces during flexion. Instability is present if more than 3.5 mm of horizontal displacement or above 11° of kyphotic deformity is observed at an involved level during dynamic imaging. However, the acquisition of dynamic studies may be limited due to muscular spasms and concurrent neck pain. This modality may also risk further neurological deterioration.
Radiological variables predicting cervical subluxation include the following:
- A space available for a cord of less than 13 mm
- An atlantodens interval of more than 5 mm in children, having higher odontoid and atlas ring cartilage content and ligamentous laxity, and 3 mm in adults
- A violation of Steel’s rule of thirds: one-third cord, one-third odontoid, and one-third space (safe zone)
- The powers ratio is determined by a line from the basion (B) to the atlas’ posterior arch (C) and a second line from the opisthion (O) to the atlas’ anterior arch (A). A value less than 0.7 suggests a posterior subluxation. In contrast, a value greater than 1 indicates an anterior subluxation.
- The Wiesel and Rothman method entails drawing a line connecting the atlas' anterior and posterior arches. Perpendicular lines are then drawn from this line, one to the basion and the other to the anterior arch’s posterior margin. The distance (x) between these 2 lines exceeds 1 mm during dynamic imaging in subluxation.
Computed Tomography
Spine computed tomography (CT) provides bony anatomic details. This modality aids in diagnosing unilateral or locked facets, concurrent foramen transversarium injury (risking vertebral artery injury), and confirming lateral mass and lamina integrity for posterior screw fixation length validation.
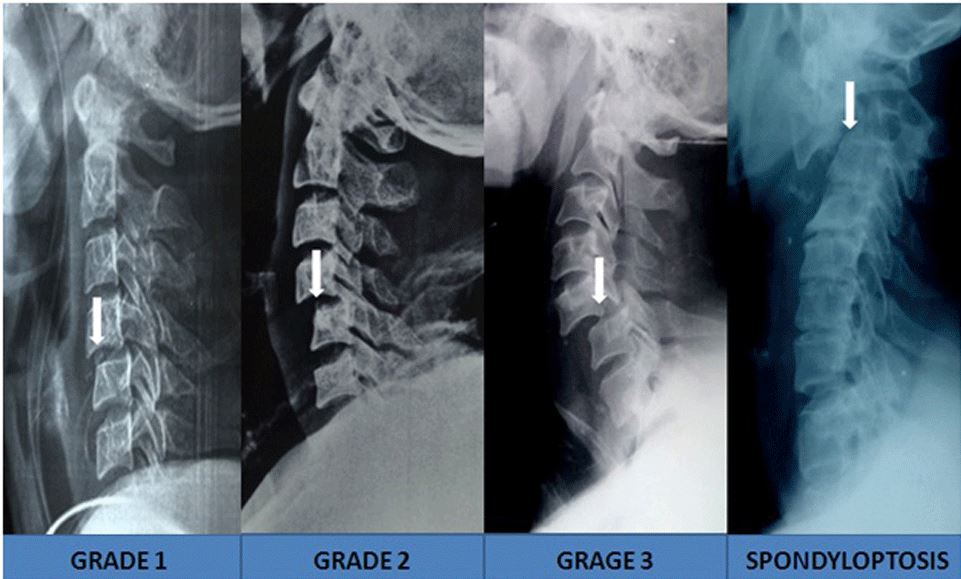
The Meyerding scoring system applies for grading cervical subluxation (see Image. Meyerding Subluxation Grading Applied to the Cervical Spine):
- Grade I: Translation up to 25%
- Grade II: Translation up to 50%
- Grade III: Translation up to 75%
- Grade IV: Translation up to 100%
- Grade V: Complete ptosis of one vertebral body over another [23]
The CT scan may show a reverse hamburger bun sign highly indicative of a facet dislocation.[24] Dynamic CT may also be applied to determine C1’s lateral inclination angle and classify chronic atlantoaxial rotatory (AAR) subluxation. The grading system is as follows:
- Grade 1: C1’s lateral inclination angle is 0°.
- Grade 2: The angle is less than 20°.
- Grade 3: The angle is greater than 20°.
Magnetic Resonance Imaging
Spine magnetic resonance imaging (MRI) is the gold standard for determining the spinal cord injury type—whether compression, transection, or central cord syndrome—and assessing ligamentous integrity. Tractography helps assess nerve tract integrity and predict neurological recovery. A traumatic syrinx may develop in a few patients with initially missed low-grade subluxations. MRI also helps determine whether the anterior or posterior surgical approach is better during reduction or bony fragment and extruded disk decompression procedures.
Vertebral Artery Angiography
Vertebral artery angiography is of prime importance, especially with fractures extending to the foramen transversarium and high-grade subluxation at the C2 to C6 levels. However, concurrent vertebral artery dissection or occlusion may sometimes occur when performing this procedure.
Treatment / Management
Traumatic cervical subluxations are categorized based on severity as follows:
- Facet subluxation
- Unilateral facet dislocation or facet fracture and dislocation
- Bilateral facet dislocations
Nondisplaced facet fractures or minimal diastasis of less than 1 mm may be managed with an orthosis alone. However, facet displacement and concurrent ligamentous injury warrant surgical fixation.[25] Spine immobilization until stabilization is mandatory. Reduction, realignment, and rigid stabilization are the management cornerstones.[26]
Reduction should be performed as early as feasible within a safe environment, preferably within 4 hours of injury, to facilitate neurological improvement. Baseline neurologic status should be recorded. Skull traction using Gardner Well tongs is applied just below the superior temporal line. An initial 2.5 to 5 kg traction weight is used. Incremental weights of 2 to 5 kg per level above the dislocation are added every 5 to 10 minutes, guided by periodic x-ray assessments and serial neurological evaluations. Incremental traction is applied under flexion to achieve reduction after facets start to unhinge.
Rotating the head 40° toward the dislocation is recommended in unilateral facet dislocation. The outcome of traction can result in 3 scenarios:
- A new neurological deficit occurs. Traction weight must be immediately reduced until the condition resolves. Urgent MRI and open reduction are necessary.
- Reduction is not achievable despite using maximum traction weights. Traction weight must be reduced to 1 to 2 kg per vertebral level above the diseased level. MRI and open reduction must be performed urgently.
- The reduction is successful. A 7.5 to 10 kg traction must be maintained, and a hard collar should be applied. MRI and surgical management planning should be undertaken afterward.
Cord traction from heavy weights must be avoided. Early reduction of locked facets and spinal canal decompression are crucial. Closed reduction is contraindicated among uncooperative patients and when imaging shows cord compression from disk or bony fragments. However, closed reduction under sedation without prereduction MRI may be safe for awake and alert patients. Attempting closed reduction under anesthesia is successful in about 95% of locked-facet cases.[27] Nonoperative management of reduced facet dislocation with traction and hard collar immobilization alone has high rates of instability.
The surgical approach options include the following:
- Standalone anterior approach
- Standalone posterior approach
- Simultaneous anterior and posterior approaches
- Staged anterior, posterior, and anterior approaches
The approach depends on several radiological variables, including the following:
- Degree of injury instability, ie, whether unilateral or bilateral, and if osteoligamentous damage is severe
- Concurrent presence of traumatic disk herniation
- The dislocation’s reducibility
The surgical plan depends on patient characteristics, ASIA neurological status, Meyerding grading, and team expertise. The anterior approach addresses herniated discs, while the posterior approach restores the posterior tension band. If traction achieves good reduction, patients may undergo an anterior approach with diskectomy or median corpectomy, followed by in-situ bony graft fusion or allograft spacer use with plate and screw fixation. If reduction fails and preoperative MR images reveal traumatic disk involvement, an anterior approach with a diskectomy, open reduction using a Casper distractor, and anterior-only fusion are recommended. In some cases, traction applied during neck flexion or when using the “level rule” may fail due to rigid locking.[28] Posterior reduction of jumped facets followed by 360° global fixations is justified in neurologically intact patients.
In people with financial barriers, simple graft placement may be considered, particularly for those with ASIA A and B status, using interspinous wiring for anatomical fixation to aid early rehabilitation. However, for patients with ASIA C and D status, the posterior approach is initially necessary to unlock jumped facets, followed by anatomical fixation with lateral mass and translaminar screw and rod fixation. This technique may be reinforced with fixation from the anterior approach. In neurologically stable patients with significant disk prolapse, diskectomy or corpectomy is performed first, followed by posterior facet unlocking and instrumentation. Anterior bony graft placement with plate and screw fixation is performed afterward (360° approach).[29]
Surgical timing is another important aspect. Failed closed reduction and progressing neurological deficits mandate urgent surgery. The Surgical Timing in Acute Spinal Cord Injury Study recommends early reduction and decompression, preferably within 24 hours, to facilitate neurological improvement. Facets should be reduced only after anterior cervical diskectomy if concurrent disk herniations are present. Reduction can be safely achieved after adequate diskectomy either by distracting Casper pins placed divergently within the vertebral bodies or using leverage from a blunt instrument within the superior endplate of the caudal vertebra to push the rostral vertebra backward. Intraoperative external cranial traction may also facilitate the process.
Following adequate reduction, fixation via conventional plates, locking plate systems, cages, or bone grafts is performed. Anterior cervical diskectomy and fusion alone does not address the loss of the tension band effect owing to posterior ligamentous complex injury, which risks postoperative kyphosis. Such adverse events are also observed following endplate fractures.
The posterior approach allows for direct visualization and reduction of locked facets using either traction-leverage maneuver or facetectomy. This technique also facilitates adequate spinal decompression and posterior fixation utilizing lateral mass, facetal, translaminar, or pedicle screws. The posterior approach enables the repair of the tension band effect. However, this method risks further neurological deterioration during concurrent traumatic disk herniations. The posterior approach is also more likely to produce wound-related complications, fail to restore cervical lordosis (including endplate fractures), and increase morbidity during positioning (particularly for unstable patients and those with polytrauma). A high incidence of delayed instability resulting in kyphotic deformity has also been reported.
The combined approaches—anterior-posterior, posterior-anterior, and anterior-posterior-anterior—are indicated in the following scenarios:
- Anterior-approach reduction failure
- Injuries requiring robust fixation and fusion
- Cases of osteoporotic bones, ankylosing spondylitis, and concurrent fractures involving endplate and facets, which necessitate spinal stability enhancement
Debates persist regarding MRI indications and timing and surgical approach preferences, with injury mechanism, pathoanatomy, and team experience being pivotal determinants. The definitive indication for an anterior or posterior approach is the site of compression. In facetal subluxation or dislocation, where the anterior spinal ligament may remain intact, the posterior approach is theoretically favored due to disrupted posterior columns and the feasibility of facet unlocking. In contrast, the anterior approach’s advantages include reduced blood loss and operating time, though it involves longer patient positioning times and higher resubluxation risk when repositioning patients lying prone.
Anterior fixation has a minimal learning curve compared to lateral mass screw fixation, which carries a 1.8% per-screw risk of radiculopathy (through the lag effect) and risks of lateral mass fractures (6%) and vertebral artery injury (6%) from screw malpositioning. Pseudarthrosis occurs more frequently with lateral mass fixation, as bone chips are only placed in the interfacet region with a small surface area. However, despite lateral mass fixation's biomechanical soundness in multiple planes of cervical motion, anterior fixation provides comparable stability.
The following is the clinical algorithm for managing atlantoaxial subluxation:
- Less than 1 week post-injury: Soft cervical collar, pain management, and stretching physiotherapy program
- More than 1 week but less than 1 month post-injury: Traction therapy, muscle relaxants, pain management, and hard cervical collar immobilization for 4 to 6 weeks
- Longer than 1 month post-injury: Traction to obtain reduction, followed by halo vest immobilization in the most physiological position of the head and neck for 6 weeks
- More than 3 months post-injury and cases with concurrent neurological signs, treatment refractoriness, recurrence, or nonoperative management failure: Posterior atlantoaxial fusion
The recommended approaches using the Arbeitsgemeinschaft für Osteosynthesefragen (AO) Spine scale system (see Staging below) are as follows:
- A0: Typically conservative treatment
- A1: Generally conservative; anterior monosegmental fusion is warranted if kyphosis exceeds 15°
- A2: Usually conservative; anterior bisegmental fusion is required if kyphosis is greater than 15°
- A3: Anterior monosegmental or bisegmental fusion
- A4: Anterior bisegmental fusion
- B1: Posterior bisegmental fusion
- B2: Approach and fusion length depend on the A component
- B3: Anterior monosegmental fusion; posterior long-segment fixation is warranted in ankylosing spondylitis
- C1: Approach and fusion length depend on the A component
- F1: Conservative treatment
- F2, F3, and F4: The approach depends on the B and C components
Asymptomatic vertebral artery injury does not typically hinder operative management of subluxations. Aspirin is recommended during the postoperative period. However, consensus has not been reached for managing symptomatic vertebral artery injuries associated with traumatic cervical spine subluxations.
Differential Diagnosis
Pseudosubluxation is considered a potential diagnosis when evaluating cervical spine abnormalities. The condition is associated with an absent cervical pedicle. The Swischuk line is utilized to determine the presence of pseudosubluxation. A line is drawn from the anterior cortex of C1's posterior arch to its counterpart in C3. A Swischuk line passing 2 mm or more behind the anterior cortex of C2's posterior arch suggests a pathological anterior displacement.
Staging
C1-C2 rotatory dislocation, defined initially by Fielding and Hawkins, is classified into 4 types:
- Type 1: Unilateral facet subluxation with intact transverse ligament. This condition is the most common subtype, with the dens acting as a pivot.
- Type 2: Unilateral facet subluxation with atlantodental interval 3 to 5 mm owing to transverse ligament injury. The facet acts as a pivot.
- Type 3: Bilateral anterior facet displacement exceeding 5 mm
- Type 4: Posterior atlas displacement with dens deficiency
Cervical subluxation is the most unstable form of cervical spine injury. Cervical spine subluxation types include the following:
- Anterior atlantoaxial subluxation
- Atlantoaxial impaction or vertical subluxation
- Subaxial subluxation [30][31]
Allen et al termed facet subluxation and dislocation "distractive flexion injuries" in 1982, describing the following radiological stages:
- Stage 1: Flexion sprain
- Stage 2: Unilateral facet dislocation
- Stage 3: Unilateral facet dislocation with up to 50% translation
- Stage 4: Bilateral facet dislocation with up to 100% translation
The ABC classification system for cervical spine injuries includes the following classes:
- A: Compression injuries
- B: Burst injuries
- C: Distraction injuries
Vaccaro et al proposed the Subaxial Cervical Spine Injury Classification System (SLIC) in 2007. This system is based on the following:
- Morphology: Type and severity of the injury, classified into compression, distraction, rotation/translation, and other injuries
- Discoligamentous complex integrity: Assesses ligament and disk integrity, with values assigned based on severity
- Neurologic status: Determines the severity of neurological deficits, graded from normal to complete motor and sensory loss
- Injury modifiers: Additional factors such as patient age, systemic disease, and associated injuries that may influence treatment decisions [32]
In 2016, AO merged SLIC with the ABC classification system. Group C encompassed translational injuries, and subgroup F specifically addressed facetal injuries. This subgroup also accounted for case-specific modifiers, including posterior ligamentous complex injury and disk herniation.
The AO spine subaxial cervical spine injury classification system categorizes injuries based on several factors:
- Injury morphology, which includes compression (A), posterior tension band (B), and translational injuries (C), each with 4 subtypes
- Facet injury, also divided into 4 subtypes
- The patient's neurological status
- Case-specific modifiers, such as central disk involvement, metabolic bone diseases, and vertebral artery injury
The AO spine classification system is crucial for managing traumatic subluxations because it assesses the status of the facet joints, which are pivotal for spinal stability. Damage to these joints justifies comprehensive spine fixation in neurologically intact patients.[33]
Prognosis
Cervical subluxation and its associated complications negatively impact patients’ functionality and quality of life.[34] When adjusted for age, patients with facet dislocation are 7.25 times more likely to have SCI than those with subluxated facets. In a study focusing on fracture/dislocation cohorts, tetraplegia occurred in 93.5% of cases, with ASIA C neurological status being the most common presentation.
Approximately 44% of these patients have at least 1 combined injury, the most common being lung contusion. Furthermore, 21.3% have at least 1 complication during their hospital stay, the most common being pulmonary infection. Hospital-acquired pneumonia and pressure ulcers risk disability and mortality, most often in patients with ASIA A, B, and C.[35] Most patients with poor neurological status are dependent on their care providers, even for carrying out activities of daily living. Moreover, the risk of repeated admissions can be as high as 30% owing to varied complications in these cohorts.[36]
Delayed or missed diagnosis has an incidence of 5% to 20% in cervical subluxation. The condition is also 5 times more likely to be neglected than the thoracolumbar spine. Concurrent disk herniation and disruption have been observed in up to 25% of cases.[37] MRI revealing a 1% increase in spinal cord compression increases SCI risk by almost 3.5%. Translation, Cobb angle, facet apposition, and cord compression are radiological variables prognosticating the clinical outcome.
Open surgical fixation is required in around 26% of patients with cervical subluxation, with a 3.7/100,000 person-years surgery rate. No statistically significant difference exists between anterior and posterior approaches relating to neurological improvement. The anterior approach, however, has less postoperative pain and wound-related morbidities and a higher fusion rate. Lateral mass screw fixation does not address kyphotic deformity. Compared with nonoperative management, cervical fusion for acute atlantoaxial rotatory subluxation was associated with increased length of stay and hospital resource utilization but had low mortality. Single-stage combined surgery has high stress imposed upon the patient, as it requires a prolonged operative time.
A 62% decrease in mortality rate (5.3% to 2.2%) has been observed from 1993 to 2014 among patients with cervical subluxation. The overall 90-day mortality in a study was 7.1%.
Complications
The early complications of cervical subluxation are as follows:
- Neurological, including quadriplegia, quadriparesis, central cord syndrome, and cruciate paralysis
- Phrenic nerve injury (C3-C5 level)
- Vertebral artery injury (C2-C6 level)
- Spinal cord injury, including compression, transection, and contusion
- Secondary complications relating to spinal cord injuries, such as pneumonia, pressure ulcers, deep vein thrombosis, urinary tract infections, muscle atrophy, and spasticity. About 84% of patients with C1 to C4 injuries and 60% of individuals with C5 to C8 injuries experience respiratory complications.
Individuals with SCI have an age-standardized mortality rate nearly 3 times higher than the general population. Late complications of cervical subluxation include delayed instability or subluxation, progressive kyphotic deformity, and traumatic syrinx.
High morbidity and mortality have been associated with prolonged external immobilization. Patients incur an increased risk of pneumonia, osteomyelitis, sepsis, deep vein thrombosis, acute kidney injury, aspiration pneumonitis, and acute respiratory distress syndrome. Ligamentous disruption has high failure rates from external immobilization alone.
Early surgical complications include surgical site hematoma, cerebrospinal fluid leak, recurrent laryngeal nerve damage, vertebral artery injury (especially in lateral mass fixation), graft extrusion, cord edema (reperfusion injury), and cord herniation. Late complications include surgical site infection, tracheoesophageal fistula, implant failure, pseudoarthrosis, adjacent segment disease, kyphotic deformity, and nonunion.
Continuum multispectral burden patterns, including physical, economic, social, and emotional, are imposed upon the care providers. A significant challenge for individuals, families, and society arises from high treatment and rehabilitation costs and lost productivity.
Postoperative and Rehabilitation Care
Rehabilitation requires the following:
- Timely anatomic stabilization to ensure structural integrity
- Focusing on preserving spinal cord function
- Early mobilization and implementation of staged rehabilitative programs
- Swift initiation of comprehensive patient care strategies to prevent secondary complications
- Aiming for patient survival, recovery, and optimal function restoration
Rehabilitative strategies for cervical subluxation injuries encompass various interventions, including physical and occupational therapy, to enhance strength, range of motion, and functional independence. These approaches may also involve using assistive devices for support, pain management techniques, and neuromuscular reeducation to optimize movement patterns and decrease the risk of further injury. Education, home exercise programs, and functional training are integral components, personalized to each patient's needs and implemented in collaboration with an interprofessional rehabilitation team.
Deterrence and Patient Education
Primary prevention involves interventions aimed at preventing cervical subluxation. Preventive measures include educational campaigns to raise awareness about the risks of activities that may lead to such injuries, such as unsafe driving and improper sports techniques. Implementing safety measures, such as using protective gear during high-risk activities and ensuring proper workplace ergonomics, can also help reduce cervical subluxation's likelihood. Additionally, promoting overall spinal health through regular exercise, maintaining proper posture, and avoiding behaviors that may strain the neck can contribute to primary prevention efforts.
Secondary prevention revolves around 3 key aspects:
- Early reduction, spinal decompression, and anatomic fixation
- Early institution of graded physiotherapy to maximize neurological recovery
- Prevention of secondary complications
Additionally, caregivers should support patients with severe deficits in their daily activities. The management plan should be tailored to address the needs of both the patient and the caregiver as a unit.
Pearls and Other Issues
Cervical subluxation management demands meticulous attention to detail and a comprehensive understanding of the injury's complexity. One key aspect is carefully assessing neurological status and injury morphology using classification systems like the SLIC and ABC. These classifications guide treatment decisions, particularly in determining the need for surgical intervention and the choice of approach. The timing of surgical treatment is also critical, balancing the urgency to stabilize the spine with considerations of patient stability and optimization. Single-stage combined surgeries, while efficiently addressing multiple aspects of the injury, can impose significant stress on the patient due to prolonged operative times. Thus, careful preoperative planning, multidisciplinary collaboration, and consideration of patient factors are essential to optimize outcomes and minimize complications during cervical subluxation management.
Enhancing Healthcare Team Outcomes
Diagnosing and managing cervical subluxation require an interprofessional healthcare team's holistic efforts. This team includes clinicians, orthopedic and neurologic specialists, nurses, and physical therapists. Many patients with this injury are first seen in the emergency department. Emergency medicine physicians are responsible for initially evaluating and stabilizing patients with cervical subluxation. Orthopedic specialists provide expertise in surgical interventions and postoperative care. Neurologic specialists focus on neurological assessment and managing associated complications.
Nurses may conduct assessments, provide ongoing monitoring, aid in surgical procedures, and administer pain relief medications. Physical therapists are crucial in both nonsurgical and postsurgical cases. Open communication channels between the team members are crucial while implementing a coordinated team effort. The interprofessional approach is the best way to optimize patient results.