Continuing Education Activity
Carotid sinus hypersensitivity is an exaggerated response to pressure applied to the carotid sinus located in the carotid bifurcation, resulting in bradycardia, vasodilation, and hypotension. This response is manifested clinically as syncope or presyncope and can cause fatal consequences. Losing consciousness in some situations is dangerous (i.e., driving). This activity reviews the etiology, approach to diagnosing carotid sinus hypersensitivity, complications, management, and patient education. The activity also highlights the role of the interprofessional team in approaching this condition, assessing the response to treatment versus its adverse effect, and the education to prevent major complications.
Objectives:
Review the etiology of carotid sinus hypersensitivity.
Summarize the evaluation of carotid sinus hypersensitivity.
Outline the management options available for carotid sinus hypersensitivity.
Discuss an interprofessional team required to care for patients with carotid sinus hypersensitivity that will result in the best outcomes.
Introduction
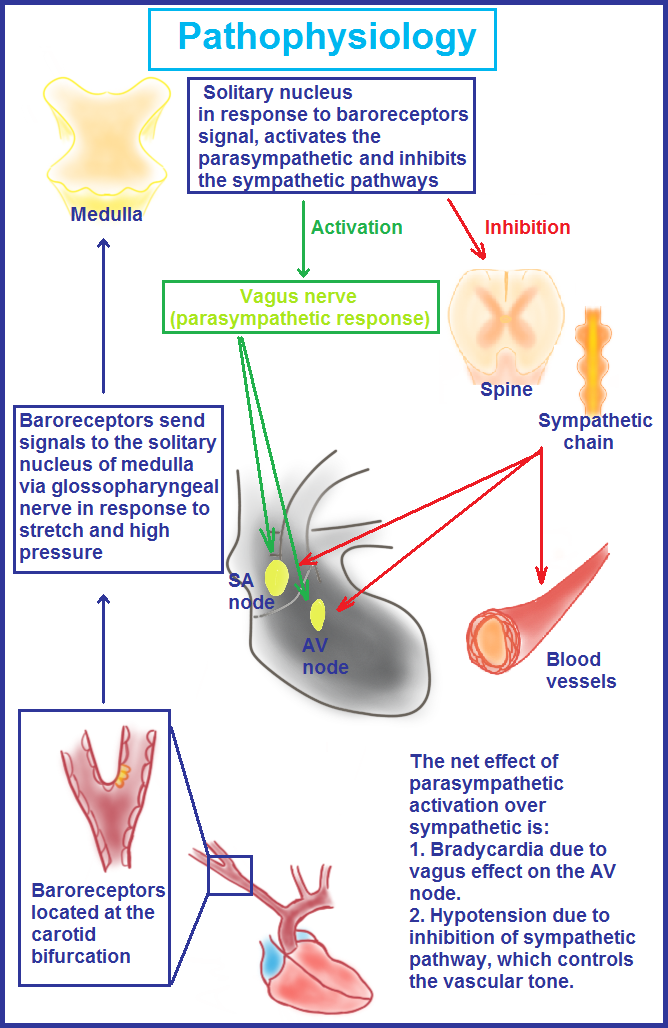
Carotid sinus hypersensitivity (CSH) is a condition that commonly manifests as syncope. Hypersensitive receptors in the carotid sinus cause an exaggerated response when stimulated, leading to CSH. The place where the internal and external carotid arteries meet to make the common carotid artery is called the carotid sinus (dilated area in the carotid bifurcation); this is a kind of neurovascular structure, which contains baroreceptors ("baro" is the Greek word for pressure or stretch) (see Graphic. Pathophysiology of Carotid Hypersensitivity Syndrome).
The baroreceptors at the carotid sinus shoot neural signals through the glossopharyngeal nerve to the solitary nucleus in the medulla. Increased pressure or stretch sensed via baroreceptors activates the parasympathetic nervous system, with the net effect of vasodilation, bradycardia, and hypotension. Hypotension further eliminates the inhibitory effect of baroreceptors.
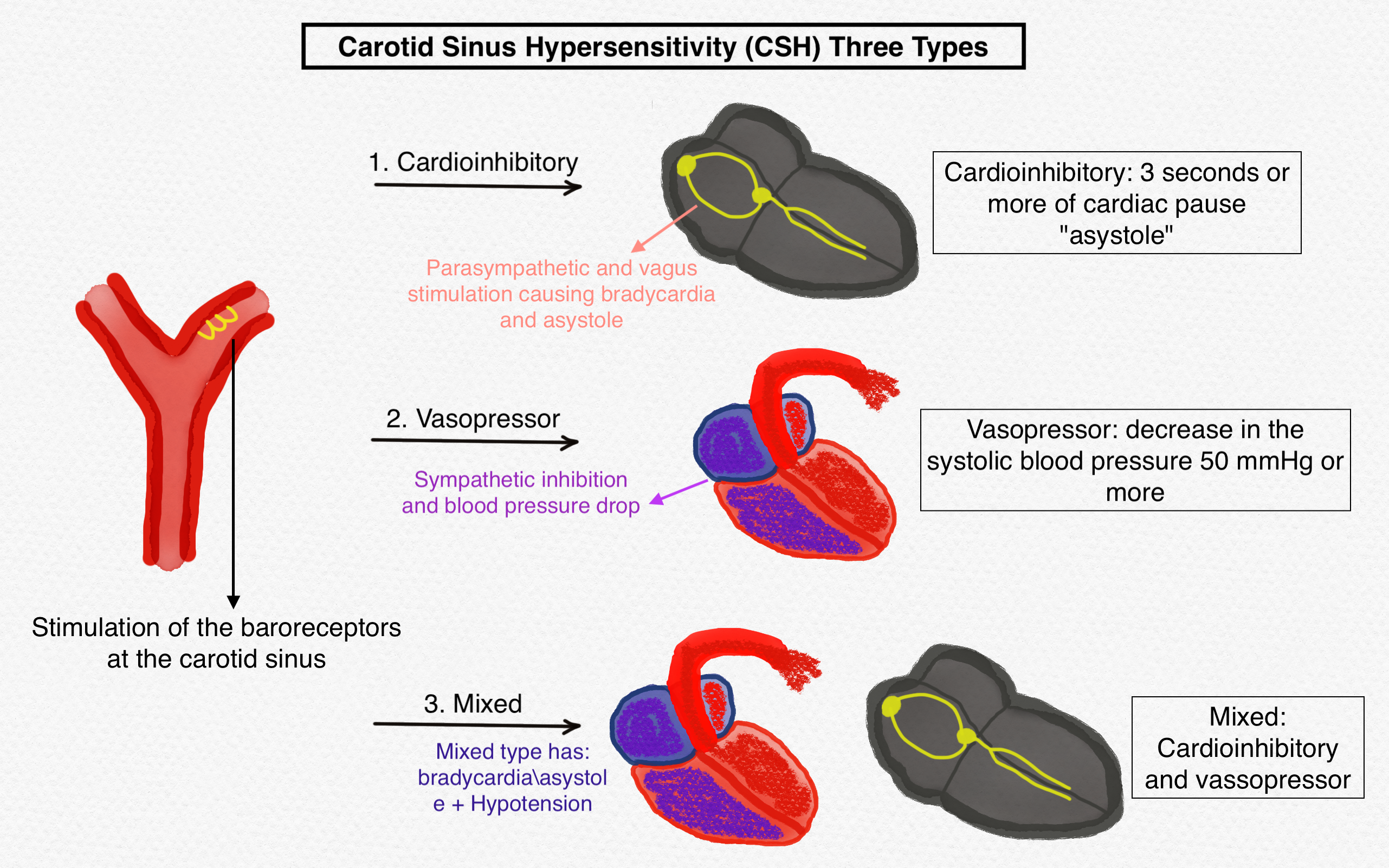
However, the objective definition of CSH includes the evolution of 3 seconds or more of cardiac pause "asystole" (cardioinhibitory) or a decrease in the systolic blood pressure 50 mmHg "hypotension" or more (vasopressor) if the massage results in hypotension and bradycardia then it is called mixed (cardioinhibitory and vasopressor), while a carotid sinus massage is made regardless of symptoms occurrence (ie, might fulfill the criteria but be asymptomatic).
There are three subtypes of CSH: cardioinhibitory, vasodepressor, and a mixed type (cardioinhibitory and vasopressor) (see Graphic. The Three Types of Carotid Sinus Hypersensitivity).[1][2][3]
Etiology
The exact cause of CSH is not well understood. However, it is known that CSH incidence increases with aging, as CSH is very unlikely before the age of 50. Furthermore, it is more common in men than in women, especially those with chronic medical conditions (hypertension, coronary artery disease, diabetes, and valvular pathologies). Besides, there is an association between neurodegenerative disorders and CSH, as the prevalence of CSH is increased in patients with Parkinson's disease, Alzheimer's dementia, and dementia with Lewy bodies. It is hypothesized that there is a degenerative pathology in the medullary autonomic nuclei, which senses baroreceptors' signals, resulting in exaggerated response, manifested as hypotension and bradycardia.[4]
Epidemiology
In the United States, carotid sinus hypersensitivity (CSH) is 35 to 40 cases per year per million. The incidence increases with age as CSH is found in the elderly population. It is virtually unknown in the younger population. CSH predominates in males more than females (the ratio is 4 to 1).[5]
The prevalence of CSH increases with age, as it was 2.4% in the sixth decade and 9.1% in the seventh, reaching 40% in people over 80 years.[6]
The worldwide prevalence of CSH is near 30% of unexplained syncope in elderly people and 14% of nursing home residents. It is worth saying that there is an overlap between CSH and vasovagal syncope, orthostatic hypotension, and other causes of syncope. This makes a margin of error in estimating the incidence rate of each condition by its own presentation as syncope (i.e., multiple etiologies beyond syncope).
The subtypes of CSH occurrence rates are 70% cardioinhibitory, 10% vasopressor, and 20% for mixed type.
Pathophysiology
The role of baroreceptors is to control the equilibrium of blood pressure and heart rate. The autonomic nervous system receives information via baroreceptors distributed in the carotid sinus, aortic arch, and great blood vessels. This control forms an arc consisting of afferent limbs; baroreceptors sense stretch and change of pressure and send signals through the glossopharyngeal nerve (baroreceptors in the carotid sinus) and vagus nerve (baroreceptors in the aortic arch) to the solitary nucleus of the medulla, which sends signals through the efferent limb; consist of sympathetic (activated if there are a decreased blood pressure or wall stretch) and parasympathetic (activated if there is an increased blood pressure or wall stretch) effects causing:
- Hypotension and bradycardia (parasympathetic)
- Hypertension and tachycardia (sympathetic)
The exact mechanism behind CSH is poorly understood and might be at any point in the previous pathways. However, what seems to be clear is that stretching or mechanical pressure over the carotid sinus overshoots signals, resulting in hypotension, bradycardia, or both.[7][8]
Recent data suggests that the theory of decreased arterial compliance due to atherosclerosis of carotids with aging and the decreased afferent reflux resulting in compensatory upregulation of the postsynaptic alpha-2 adrenoreceptor in the brainstem is not true because afferent limb of the carotid sinus reflex was normal in the CSH population, and the study on 18 patients with CSH failed to attenuate baroreflex in patients with CSH after the administration of Yohimbine (alpha-2-receptors antagonist), meaning the alpha-2 receptors upregulation have no role in CSH.[9][6]
Histopathology
It is noted that when CSH is associated with neurodegenerative disorders, there is tau protein hyperphosphorylation and alpha-synuclein accumulation in the medulla on histological examination with special stains and techniques, which might be the reason behind the association between CSH and neurodegenerative disorders.[4][10]
History and Physical
The medical history of CSH patients might show hypertension, diabetes, coronary artery disease, and neurodegenerative disorders (Parkinson's and Alzheimer's). Physical exams might be normal except for the clinical manifestations of the previously mentioned disorders.
Symptomatic CSH mainly presents with the following:
Signs and Symptoms
- Presyncope or syncope
- Unexplained falls
- Visual changes before consciousness loss (ie, darkening visual field).
Physical Examination
- Hypotension
- Pallor
- Bradycardia
- Bruises related to fall injury
It is very important to determine the cause of falls or syncope in the elderly, as it is very likely to miss a critical condition (severe aortic stenosis, arrhythmias) or neurologic conditions (seizure or stroke). Such a miss can lead to critical results, especially if the patient has recurrent episodes of syncope while driving, during sea activities (swimming and diving), parachuting, or running heavy machinery. On the other hand, CSH can be asymptomatic and only happens during a carotid massage. It is worth mentioning that CSH diagnostic criteria during carotid massage might happen without symptoms.
It was mentioned in the medical literature that in rare cases of head and neck tumors, there has been a hyper-response of the carotid sinus to the tumor burden pressing over baroreceptors (the management depends on the primary tumor, stage, age, and prognosis).[11]
Evaluation
Approach syncope by getting the vital signs, assessing for orthostatic hypotension, and getting the history of dehydration induced by coughing, micturition, or exercise, i.e., hypertrophic cardiomyopathy and aortic stenosis. A family history of sudden cardiac death, medical and surgical history (postprandial syncope after gastrointestinal surgery), complete blood count, basic metabolic panel, and fingerstick glucose (hypoglycemia causes unconsciousness) should be obtained. It is also important to have an electrocardiogram (ECG) and, in certain cases, an echocardiogram. Performing a neurologic exam to screen for transient ischemic attack (TIA) or strokes is needed. The tilt table test is also helpful for diagnosing vasovagal syncope and orthostatic hypotension. Performing a brain CT scan or electroencephalogram EEG if the presentation suggests neurologic etiology is also helpful.
Other diagnostic options can be used (ie, Holter monitor and cardiac electrophysiologic study). However, the best method to diagnose CSH is via monitored carotid massage (but again, other causes of syncope must be ruled out, and history helps to choose the proper diagnostic option). Non-accidental falls in the elderly following a sudden loss of consciousness must be approached wisely to avoid misdiagnosing and event recurrence.
Massage Technique: With the patient in the supine position, use the second and third fingers over the carotid sinus, which is located anterior to the sternocleidomastoid muscle at the level of the upper border of the thyroid cartilage. First, massage the right carotid sinus as there are a bunch of receptors, and there is a greater response than the left. Massage for 5 to 10 seconds with a circular motion. If there is no response, switch to the left carotid sinus unless it is contraindicated. If there is asystole for 3 seconds or more and/or a drop in systolic blood pressure of 50 mmHg or more, the test is considered positive regardless of symptoms evolution. If the test is not diagnostic, one may repeat the test with the patient in the upright position or using a tilt table (prepared emergency equipment and skillful staff must be at the scene of the carotid massage).[12][13]
Contraindications to carotid sinus massage:
- Absolute contraindications are stroke, transient ischemic attack (TIA), and myocardial infarction in the previous three months.
- Relative contraindications include arrhythmia (ventricular tachycardia or ventricular fibrillation) and bruit over the carotid artery; in case of bruit presence, an echo-doppler should be done, if showing stenosis of 70% or more, then it is a contraindication for carotid massage (it is acceptable to do a carotid massage with a stenosis level of 50 to 69%).[13][14]
Treatment / Management
General approach: Educating the patient about CSH and what might trigger an event (explain the events, cardioinhibitory or vasopressor); ie, avoid tight collar dressing, chiropractic activities around the neck, or manipulation around the carotid sinus besides the control of associated medical conditions (for example hypertension, diabetes, etc).
Asymptomatic patients who fulfill the criteria for CSH diagnosis without developing an event need no further evaluation (this finding is when approaching syncope diagnosis for a reason other than CSH).
Asymptomatic patients who develop an event during monitored carotid massage (supervised) and otherwise asymptomatic need no further treatment except for avoiding triggers and controlling other medical issues.
Symptomatic patient's treatment depends on the CSH subtype:
- The Vasopressor subtype maintaining a proper status of hydration and salt intake up to 6 gm/day if not contraindicated (hypertension and congestive heart failure) is enough to control most of the cases; if still symptomatic, adding fludrocortisone (mineralocorticoid) or midodrine (The alpha-adrenergic agonist) if not contraindicated as hypertension is usually existed in CSH population, adjusting the medication dosage and timing is important in avoiding hypertension and CSH events.[15][16]
- The cardioinhibitory subtype, the use of a dual-chamber pacemaker, is the cornerstone of the management. The reason beyond using a dual-chamber pacer is that, in some cases, there is a complete block at the AV node, and a dual-chamber pacemaker can overcome this by stimulating both the atria and the ventricles. It is also wise to use a pacemaker in the mixed subtype. However, in this case, an event development is still possible because of the vasopressor component in the mixed type. Still, the incidence of events is decreased with pacemaker placement, especially if the vasopressor is managed properly.[17][18]
- There is an association between sick sinus syndrome (SSS) and CSH, and they coexist in 26% of cases. Pacemaker placement is beneficial for both cases.[19]
- Surgical or radiologic denervation of the carotid sinus was previously used to treat CSH. However, these procedures are no longer used because of their complications.
Differential Diagnosis
CSH can manifest as a syncopal attack that makes it a challenging task to approach it properly, especially when the historical carotid stimulation is not clear in the presentation (in case of sudden neck movement or a rush in blood pressure ie the patients will not always mention a carotid stimulation). Here are the most common conditions that mimic CSH:
- Vasovagal syncope (preceded by prodromal symptoms and usually evoked via pain or the scene of blood).
- Situational syncope (evoked via cough, defecation, and micturition ("a sudden increase in intraabdominal pressure").
- Orthostatic hypotension (change in blood pressure between standing and laying down).
- Cardiogenic syncope.
- Arrhythmias (Electrocardiogram and Holter monitor help in diagnosing).
- Myocardial infarction (ECG and cardiac enzymes).
- Massive pulmonary embolism.
- Severe Aortic stenosis.
- Seizures.
- Hypertrophic cardiomyopathy.
- Transient ischemic stroke.
- Loss of consciousness due to metabolic and toxic conditions (ie, hypoglycemia).
- Medication adverse effect.
Hence, a proper wide approach that does not ignore critical conditions should occur in the diagnosis process. Each syncope case must be scanned and examined well, with the proper diagnostic plan and management. Anyway, some of the syncopal cases remain undiagnosed.[20]
Prognosis
The mortality rate of CSH patients is the same as the general population; CSH in itself is not considered dangerous. However, syncope-related injuries are what matters for these patients; nonaccidental falls or loss of consciousness on serious occasions can result in multiple fractures or intracranial bleeding, especially since many elderly patients are on anticoagulants or/and antiplatelet medication, which can result in fatal consequences.[21][22]
Complications
The major complication is non-accidental falls, which might be serious due to the CSH elderly population (taking anticoagulants, osteoporosis, poor candidates for surgical intervention, or high risk for postsurgical complications). Another issue to consider is while performing carotid massage for diagnosis, ignoring good carotid evaluation (excluding bruits and carotid artery stenosis) may evoke a stroke.[23]
Deterrence and Patient Education
Educating the patient about the nature of the disease and its consequences is essential in the management plan; it is helpful to avoid wearing tight collar clothing and minimize pressure application near the sinus node (e.g., while shaving).
It is also mandatory to avoid actions that require full consciousness (driving, running heavy machinery, and performing sea activities, ie, diving or swimming). Driving depends on each state's laws, and physicians must report on these laws. However, the patient can retain these activities if proper treatment is achieved (pacemaker placement which can eliminate the cardioinhibitory CSH subtype; in this case, the patient can drive after one week of the pacemaker placement), for the vasodepressor subtype stabilizing the blood pressure might help in returning to the previous activities.[24]
Enhancing Healthcare Team Outcomes
CSH is a cause of syncope in the elderly. Physicians must approach syncope wisely. Ruling out life-threatening conditions first is a priority; after that, a monitored carotid massage is allowed (if not contraindicated), and management of CSH is directed toward education about the condition and its consequences in the first place, not ignoring the patients' activities requiring a full consciousness, treating the symptomatic patient helps continue daily life activities ie, driving (after a symptom-free period post-management concerning each state's law and the case conditions). The interdisciplinary collaboration between the healthcare team to approach patients presenting with syncope and the highly skilled hands are needed at healthcare facilities to give suitable care because determining the etiology behind syncope helps decrease morbidity and mortality rates.