Continuing Education Activity
Cardiopulmonary bypass (CPB) is a critical technology in cardiac surgery, allowing for the temporary replacement of the heart and lung functions during intricate surgical procedures. The CPB circuit, or heart-lung machine, diverts venous blood from the patient, oxygenates and filters it, and then returns it to the arterial system, ensuring continuous perfusion of vital organs while the heart is stopped. This process involves various components, including venous and arterial cannulas, oxygenators, heat exchangers, and pumps, and requires meticulous coordination and precise control to maintain patient stability and prevent complications.
By participating in this course, clinicians enhance their competence in managing CPB procedures by comprehensively understanding its mechanics and components. They gain skills in operating and troubleshooting CPB equipment, optimizing patient safety, and improving outcomes through effective interprofessional communication and coordination. The course also covers preoperative planning, intraoperative management, and postoperative care strategies, enabling clinicians to deliver high-quality, patient-centered care in cardiac surgery settings.
Objectives:
Identify appropriate candidates for cardiopulmonary bypass based on surgical indications and patient characteristics.
Differentiate between venous and arterial cannulation techniques for cardiopulmonary bypass initiation.
Assess cardiopulmonary bypass circuit function and patient response during bypass, including monitoring vital signs and blood gases.
Collaborate and communicate effectively with the interprofessional healthcare team, including anesthesia providers and surgical team members, to optimize perioperative care and patient outcomes.
Introduction
Cardiopulmonary bypass (CPB) is a crucial technology in modern cardiac surgery that answered one of the toughest questions in the history of medicine: Can we operate on human hearts without causing mortality to the patient? Early heart surgeries were limited to conditions deemed safe for operation, such as minor tears of the pericardium, heart, and vessels, or extracardiac congenital conditions like coarctation of the aorta and patent ductus arteriosus. The revolutionary breakthrough in cardiac surgery included the development of CPB—a procedure that stops the heart, allowing surgeons to create a bloodless field and providing a motionless environment for intricate procedures while continuing to maintain essential blood flow and oxygenation to the body's organs.[1][2][3][4]
The CPB circuit includes a pump to circulate blood and an oxygenator to exchange oxygen and carbon dioxide, replicating the physiological processes of the heart and lungs. Since its inception in the mid-twentieth century, CPB has enabled complex heart surgeries, including coronary artery bypass grafting, valve replacements, and congenital heart defect corrections. Continuous advancements in CPB technology have enhanced safety, reduced complications, and improved patient outcomes. However, the procedure carries risks, such as inflammatory responses, coagulopathies, and potential organ dysfunction, necessitating careful management and coordination among the surgical team, perfusionists, anesthesiologists, and nursing staff. Understanding the principles, techniques, and advancements in CPB is essential for all healthcare professionals involved in cardiac surgery, as it directly impacts the success of surgical interventions and patient recovery.
Anatomy and Physiology
CPB is multifaceted in cardiac surgery, involving several critical functions to support the patient's cardiovascular system during surgical procedures. First, CPB facilitates emptying the heart by draining blood through venous cannulas, allowing the surgical team to operate on a bloodless field. The blood is then oxygenated outside the body using pump oxygenators, temporarily taking over the lung's role in oxygenation.[5] Additionally, CPB includes mechanisms to adjust the blood's chemical composition and electrolyte levels via a reservoir container and regulates its temperature using a heat exchanger machine.
Furthermore, CPB returns the oxygenated blood to the patient's circulation through arterial cannulas, ensuring continuous perfusion of vital organs. Additionally, it collects and salvages blood lost during surgery using cardiotomy suckers, thereby minimizing the need for blood transfusions. CPB systems often incorporate cardiac vents to prevent heart enlargement during surgery by maintaining optimal cardiac pressures. CPB can deliver cardioplegia—a specialized solution that induces temporary cardiac arrest to protect myocardial tissue during delicate procedures. CPB setups include adjuncts and standby pathways within a closed circuit driven by pumps and interconnected by tubing to enhance safety, ensuring the patient's stability and viability throughout the surgical intervention.
Understanding CPB's anatomy and physiology involves recognizing its impact on the body's inflammatory response. Research indicates that CPB triggers a systemic inflammatory response syndrome due to several factors. Blood coming into contact with the artificial surfaces of the CPB circuit initiates a cascade of events involving complement activation, leukocyte activation, and endothelial cell dysfunction. Surgical trauma, endotoxemia (due to gut-derived toxins entering the bloodstream during surgery), blood loss, and ischemia-reperfusion injury further exacerbate this response. These processes collectively lead to the release of pro-inflammatory cytokines, reactive oxygen species, and nitric oxide, contributing to oxidative stress.[6] Elevated oxidative stress during CPB is associated with increased postoperative morbidity and mortality rates.
Clinicians must know these physiological responses to mitigate potential complications. Strategies to minimize inflammatory responses and blood loss include using biocompatible CPB circuits, administering anti-inflammatory agents, optimizing surgical techniques for reducing trauma, and maintaining meticulous hemostasis. Understanding the intricate balance between achieving effective cardiac surgery and managing CPB-induced physiological responses is crucial for improving patient outcomes in cardiac surgery.
Indications
CPB is indicated in cardiac surgery when procedures require temporary cessation of the heart's function and bypassing of the heart and lungs to facilitate surgical repair. The primary indications for CPB include:
- Coronary artery bypass graft
- CPB is commonly used during coronary artery bypass graft surgery to bypass blocked coronary arteries with grafts (usually veins or arteries from elsewhere in the body) to restore blood flow to the heart muscle.
- Valve replacement or repair
- CPB is necessary for repairing or replacing heart valves affected by stenosis or regurgitation.
- Congenital heart defects
- Children and adults born with congenital heart defects, such as septal defects or complex structural abnormalities, may require CPB for corrective surgeries.
- Aortic aneurysm repair
- Surgical repair of aneurysms involving the aorta often involves CPB to maintain blood flow while repairing the weakened artery wall.
- Cardiac tumor removal
- CPB may be used during surgical removal procedures in benign or malignant tumors affecting the heart.
- Heart transplantation
- CPB supports the circulation during heart transplant surgeries, allowing for the removal of the diseased heart and its replacement with a healthy donor heart.
The decision to use CPB depends on the specific surgical procedure and the patient's overall health status. By using CPB, surgeons can work on the heart while maintaining adequate oxygenation and circulation throughout the body, reducing the risk of complications during complex cardiac surgeries.
Contraindications
There are no absolute contraindications for CPB; however, surgeons may postpone surgery considering associated complications or pathophysiology in specific scenarios. These situations include acute kidney impairment, acute cerebral stroke, chest infection, or severe asthma exacerbations.[5][7][8][9] Delaying surgery when possible is preferred to optimize outcomes and minimize risks.
Equipment
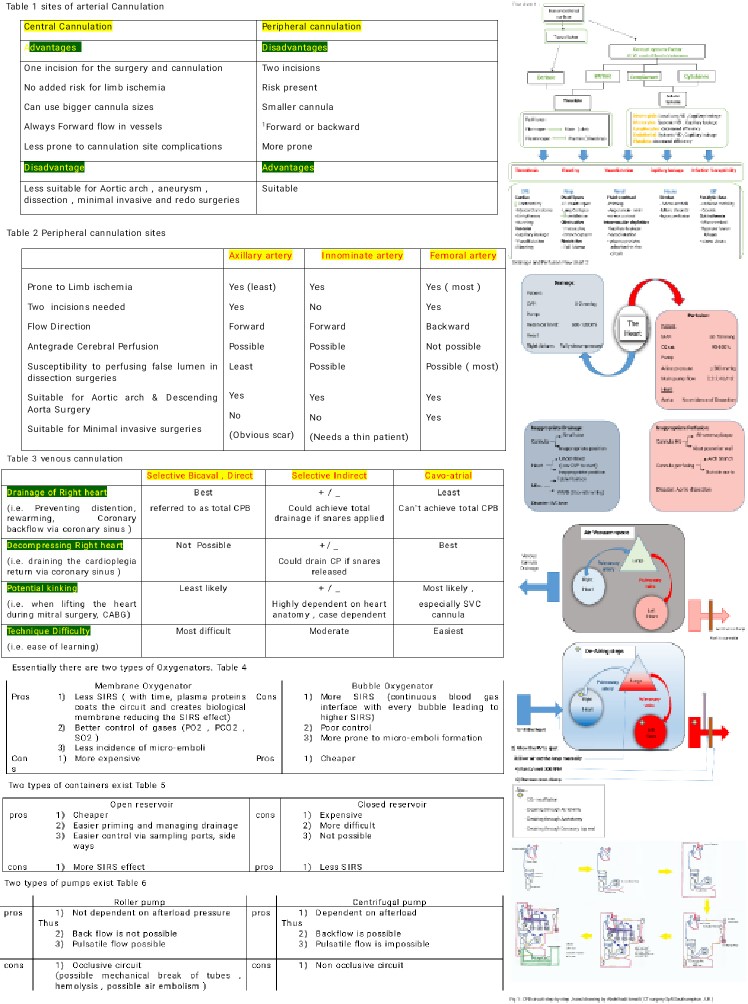
The components of the CBP machine include the following:
Venous Cannulas
Venous cannulas divert deoxygenated blood from the body into the CPB circuit. They are typically placed in the right atrium, superior vena cava, or inferior vena cava. The design of venous cannulas ensures efficient drainage and minimizes the risk of air embolism. They come in various sizes and shapes to accommodate different patient anatomies and surgical requirements.
Arterial Cannulas
Arterial cannulas return oxygenated blood from the CPB circuit to the patient’s arterial system. They are usually inserted into the ascending aorta but can also be placed in peripheral arteries like the femoral artery. The design of arterial cannulas focuses on minimizing blood flow resistance and reducing the risk of vessel injury or dissection. The aortic cannula must be safe to insert smoothly (atraumatic tip and surface), with no high-pressure gradient jet at the tip that could dislodge atheromatous plaques, and of a suitable size to allow sufficient flow. Various designs of arterial cannulas are available. Nothing is termed the best cannula; each cannula enjoys specific features that suit a particular situation. All cannulas are used in practice, and it is up to the surgeon to assess the situation and decide which to use. The following briefly describes some of the features and their values.
- Right-angled
- Prevents perforating the posterior wall of the aorta
- Can selectively perfuse an arch branch
- Straight
- Prevents selective arch vessel perfusion
- Can penetrate the posterior wall of the aorta
- Beveled tip
- Easier insertion
- Higher pressure gradient delivered at the tip
- Diffusion tip
- Less pressure gradient allows better perfusion of arch branches
- Slightly more complex
- Wire reinforced
- Allows higher flow for a smaller cannula
- More immune to iatrogenic dissection
- Flanges
- Hemostatic
- Acts as anchor points for the purse strings
Heat Exchanger
Heat exchangers in CPB circuits regulate the temperature of the blood. They allow for the controlled cooling and warming of blood, crucial for protecting organs and tissues during surgery. The exchanger typically consists of a series of metal plates or tubes through which blood and a temperature-controlled fluid (usually water) flow, allowing heat transfer between the 2.
Oxygenators
- Membrane oxygenators
- These devices use a semipermeable membrane to facilitate gas exchange. Blood flows on 1 side of the membrane, while a gas mixture flows on the other. Oxygen diffuses into the blood, and carbon dioxide diffuses out. Membrane oxygenators are preferred for their efficiency and lower risk of blood trauma.
- Bubble oxygenators
- In these devices, blood is oxygenated by direct contact with oxygen bubbles. While effective, membrane oxygenators have largely replaced bubble oxygenators due to higher risks of blood trauma, embolism, and inflammatory responses.
Reservoir Container
- Open reservoirs
- These containers collect blood from the patient and allow it to mix with air before entering the CPB circuit. They offer easy access for adding medications or fluids but pose a higher risk of air embolism and contamination.
- Closed reservoirs
- These containers prevent blood from coming into contact with air, reducing the risk of air embolism and contamination. Closed systems are generally safer and more efficient at maintaining blood volume and pressure.
Pumps
- Roller pumps
- These pumps use rollers to compress a section of tubing, propelling blood forward. They are simple and reliable but can cause blood trauma and are associated with risks of tubing rupture and air embolism.
- Centrifugal pumps
- These use a rotating impeller to create a centrifugal force that moves blood through the circuit. They are gentler on blood cells, reducing hemolysis and trauma, and provide a more consistent flow without the risk of tubing rupture.
Tubing
All tubes are made of polyvinyl chloride, which is nonallergic, nonmutagenic, nontoxic, nonimmunogenic, pliable, flexible, and transparent. The venous tube is 1/2 inch (12 mm), the arterial tube is 3/8 inch (8 mm), and the vents and suckers are 1/4 inch (6 mm).
Cardiotomy Suckers
Cardiotomy suckers are used to remove blood from the surgical field and return it to the CPB circuit. They help maintain a clear operative field and reduce blood loss. Blood collected by cardiotomy suckers is filtered to remove air and debris before being reinfused into the patient.
Vents
Vents are used to decompress the heart and prevent air embolism during CPB. They are typically placed in the left ventricle, left atrium, or pulmonary artery. Vents ensure that air does not accumulate in the heart chambers, which could lead to serious complications. They also help manage heart volume and pressure during surgery.
Adjunct Equipment
This includes the level detector, arterial line pressure meter, arterial line bubble trap and filter, cardioplegia line pressure meter, gas line filter, gas flow meter, and 1-way valves on cardiac vents (see Image. Cardiopulmonary Bypass Figures and Tables).
Personnel
A highly skilled, multidisciplinary team is needed to successfully implement CPB and patient safety. The following personnel are typically involved in the process:
- Cardiac surgeon
- Oversees the entire surgical process, including the setup and initiation of CPB
- Ensures correct cannulation for CPB
- Manages surgical interventions while the heart is on bypass
- Anesthesiologist
- Administers anesthesia and monitors the patient's vital signs
- Manages the patient's hemodynamics and fluid balance
- Coordinates with the perfusionist and surgeon to ensure optimal conditions for CPB
- Perfusionist
- Sets up and manages the CPB circuit, including oxygenators, pumps, and cannulas
- Monitors and adjusts blood flow, oxygenation, and other parameters
- Ensures proper anticoagulation and manages any complications related to CPB
- Surgical nurses
- Scrub nurse
- Prepares and hands surgical instruments to the surgeon
- Circulating nurse
- Manages the overall environment of the operating room, supplies necessary equipment, and ensures sterility
- Cardiovascular technician
- Helps in the setup and testing of CPB machinery
- Assists the perfusionist with equipment management and troubleshooting
- Intensive care unit staff
- Monitors and manages the patient's recovery postsurgery
- Ensures proper functioning of life support systems and manages complications
- Pharmacist
- Prepares and provides medications required during and after the procedure
- Advises the medical team on drug interactions and optimal pharmacological management
- Biomedical engineer
- Ensures that all CPB equipment is functioning correctly
- Performs regular maintenance and repairs as needed
- Respiratory therapist
- Assists with ventilation settings and management before, during, and after CPB
- Monitors blood gases and adjusts ventilator settings accordingly
- Echocardiographer
- Conducts intraoperative echocardiograms to guide the surgeon
- Assists in the assessment of cardiac function before, during, and after CPB
- Clinical pathologist
- Ensures timely analysis of blood samples for coagulation, oxygenation, and other parameters
- Advises the medical team on laboratory findings and their implications for patient care
- Sterile processing technicians
- Sterilize and prepare surgical instruments and equipment
- Ensure timely availability of sterile supplies during the procedure
Preparation
Preoperative Assessment
Before starting CPB, a thorough preoperative assessment is crucial to identify potential risks and ensure patient safety. This includes:
- History and physical examination
- Evaluating the patient's cardiovascular and pulmonary status, comorbid conditions, and previous surgical history
- Diagnostic tests
- Performing echocardiography, coronary angiography, and other relevant imaging studies to assess the heart's anatomy and function
- Laboratory tests
- Checking complete blood count, coagulation profile, electrolytes, renal, and liver function tests
Anesthesia Induction
- General anesthesia
- The patient is administered general anesthesia, ensuring they are fully unconscious and immobile during the procedure.
- Monitoring
- Invasive and noninvasive monitoring devices are placed, including arterial lines, central venous lines, pulmonary artery catheters, and transesophageal echocardiography.
Patient Positioning
- The patient is positioned supine on the operating table, ensuring optimal access to the surgical site and cannulation points.
- Proper padding and support are provided to prevent pressure injuries and ensure patient comfort.
Surgical Site Preparation
- The surgical site is sterilized using appropriate antiseptic solutions.
- Sterile drapes are placed around the surgical field to maintain a sterile environment.
Heparinization
- CPB is a nonendothelial circuit. Blood that is not well anticoagulated is prone to massive clotting. Accordingly, before going on bypass, a specific dose of intravenous heparin is given (300 units/kg or 3 g/kg). The sufficient level of anticoagulation is judged by checking the activated clotting time (ACT) in the operating room. The following ACT values indicate if there is adequate heparinization:
- >300 s is safe for cannulation
- >400 s is safe for going 'on bypass' (ie, starting CPB)
- >480 s is safe for initiating deep hypothermic circulatory arrest
- If the ACT only increases marginally after full heparinization, heparin resistance may be suspected, commonly due to antithrombin III (AT3) deficiency. After consulting the surgeon, if a total dose of 600 units/kg of heparin does not achieve an ACT greater than 480 seconds, recombinant AT3 concentrate should be considered. Alternatively, fresh frozen plasma, which contains AT3, may be administered. The ACT is checked every 30 minutes during the operation, and if it falls below 480 seconds, an additional 500 units of heparin are administered.
Arterial Cannulation
Arterial cannulas are placed to return oxygenated blood from the CPB circuit to the patient. They can be placed centrally or peripherally. The choice between central and peripheral cannulation and the specific peripheral site depends on the patient's anatomy, the type of surgery, and the surgeon's expertise. Each approach has advantages and limitations that must be carefully considered to optimize patient outcomes. They are described below:
- Central cannulation
- Pros:
- Direct access to the heart
- Involves cannulating the ascending aorta and right atrium or vena cava, providing direct access to the heart and great vessels
- Optimal flow rates
- Allows for high flow rates and efficient CPB management
- Reduced risk of limb ischemia
- Since cannulation is performed directly on the heart, peripheral limbs are not at risk of ischemia.
- Easier management of cardiac venting
- Facilitates better control of cardiac decompression and venting
- Cons:
- Increased surgical invasiveness
- Requires a sternotomy or thoracotomy, which are more invasive and carry higher risks of complications and longer recovery times
- Risk of aortic dissection
- Manipulating ascending aorta carries a risk of aortic dissection or injury
- Limited in reoperations
- Can be challenging in patients with previous cardiac surgeries due to adhesions and scar tissue
- Central cannulation is the most commonly used site in practice; however, it is less favored in certain circumstances, such as:
- Aortic arch surgery
- In the past, surgeons cannulated the ascending aorta first to achieve a hypothermic circulatory arrest. They removed the cannula and reinserted it into the carotid artery to provide antegrade cerebral perfusion. The same cannula can cannulate the axillary artery, reducing manipulation and time.
- Aortic aneurysm surgery
- Sometimes, the aorta is dilated or aneurysmal, and there is a risk of rupture during a sternotomy; thus, using peripheral cannulation first on bypass before opening the chest could be a safer option.
- Aortic dissections
- The whole aorta could sometimes be obscured by the false lumen.
- Peripheral Cannulation
- Pros:
- Less invasive
- Can be performed without a sternotomy, reducing surgical trauma and recovery time
- Suitable for minimally invasive procedures
- Ideal for minimally invasive cardiac surgeries and procedures requiring rapid cannulation and initiation of CPB
- Alternative in operations
- Can be advantageous in patients with previous sternotomies or complex chest anatomy
- Cons:
- Risk of limb ischemia
- Cannulation of peripheral arteries, especially the femoral artery, can lead to limb ischemia and require additional monitoring and management.
- Suboptimal flow rates
- Peripheral cannulation may not achieve the same flow rates as central cannulation, potentially affecting the efficiency of CPB.
- Cannulation site complications
- There is an increased risk of local complications, such as infection, bleeding, and vessel injury at the cannulation site.
- Peripheral cannulation sites
- Axillary artery
- Pros:
- Reduced risk of limb ischemia
- The axillary artery provides a reliable site with a lower risk of limb ischemia compared to femoral cannulation.
- Adequate flow rates
- Provides sufficient flow rates for CPB and is suitable for extended periods
- Less atherosclerosis
- Less prone to atherosclerotic disease, reducing the risk of embolic events
- Cons:
- Technical difficulty
- Can be technically challenging and requires careful surgical dissection
- Risk of brachial plexus injury
- Proximity to the brachial plexus increases the risk of nerve injury during cannulation
- Innominate artery
- Pros:
- Central flow rates
- Provides flow rates comparable to central cannulation, supporting effective CPB
- Reduced risk of limb ischemia
- Avoids limb ischemia associated with femoral artery cannulation
- Cons:
- Technical complexity
- Technically demanding and requires precise surgical technique
- Risk of stroke
- Manipulation of the innominate artery can increase the risk of cerebrovascular events.
- Femoral artery
- Pros:
- Ease of access
- Easily accessible, especially in emergency situations or minimally invasive procedures
- Rapid cannulation
- Allows for quick establishment of CPB, which is beneficial in urgent cases
- Cons:
- High risk of limb ischemia
- Necessitates continuous monitoring and potential use of distal perfusion catheters
- Atherosclerosis
- More likely to be affected by atherosclerosis, increasing the risk of embolic complications
- Lower flow rates
- May not achieve the same flow rates as central or other peripheral sites, potentially affecting CPB efficiency
Venous Cannulation
Venous cannulas, which can be 1- or 2-stage, are inserted to drain deoxygenated blood from the patient into the CPB circuit.
- 1-stage venous cannulation
- A single cannula is inserted into the right atrium, providing drainage from the superior vena cava (SVC) and inferior vena cava (IVC).
- Advantages:
- Simplicity: easier and quicker to insert
- Less invasive: requires fewer incisions and less manipulation of the heart and great vessels
- Reduced bleeding risk: fewer entry points minimize the risk of bleeding complications
- Disadvantages:
- Limited flow: may not provide optimal venous drainage, particularly in larger patients or during procedures requiring full cardiac decompression
- Inadequate for complex surgeries: not suitable for procedures requiring complete isolation of the heart, such as certain valve repairs or congenital heart defect corrections
- 1-stage is used in selective indirect bicaval cannulation.
- 1-stage right-angled is used in selective direct bicaval cannulation (avoids back wall abutting and block)
- 2-stage venous cannulation
- Involves 2 separate cannulas, 1 placed in the SVC and 1 in the IVC, or a 2-stage cannula that provides separate drainage ports for the SVC and IVC
- Advantages:
- Optimal drainage: provides superior venous drainage and decompression of the heart
- Versatility: suitable for complex cardiac procedures where complete cardiac isolation is necessary
- Enhanced control: allows for precise management of venous return and better visualization of the surgical field
- Disadvantages:
- Complexity: more technically demanding and time-consuming to insert
- Increased invasiveness: requires additional incisions and manipulation of the heart and great vessels, increasing the risk of complications
- 2-stage is used in cavoatrial venous cannulation
There are 3 types of venous cannulation that can be performed:
- Cavoatrial cannulation
- Involves a cannula inserted at the junction of the IVC and the right atrium
- Advantages:
- Simpler technique: easier to perform and requires less precise placement compared to bicaval cannulation
- Adequate drainage: provides effective drainage for many standard cardiac procedures
- Disadvantages:
- Limited control: less control over individual vena cava drainage, which may not be suitable for more complex surgeries requiring complete isolation of the SVC and IVC
- Direct selective bicaval cannulation
- Involves placing separate cannulas directly into the SVC and IVC
- Advantages:
- Complete isolation: provides complete isolation of the right atrium, which is essential for procedures such as tricuspid valve repair and certain congenital heart defect corrections
- Optimal drainage: ensures maximum venous return and cardiac decompression
- Disadvantages:
- Technical complexity: more challenging and time-consuming to perform
- Increased risk: higher risk of bleeding and vessel injury due to multiple cannulation sites
- Indirect selective bicaval cannulation
- Utilizes a 2-stage cannula that has separate drainage ports for the SVC and IVC, inserted through a single incision
- Advantages:
- Simplified procedure: easier and quicker to perform compared to direct bicaval cannulation
- Adequate drainage: provides effective drainage and partial isolation of the heart
- Disadvantages:
- Less complete isolation: does not offer complete isolation of the right atrium like direct bicaval cannulation
- Potential for incomplete drainage: may not be suitable for all complex cardiac procedures requiring complete separation of venous return
Technique or Treatment
After the preparation is finished and the cannulas have been placed, CPB begins. During CPB, a heart-lung machine temporarily takes over the patient's blood circulation and oxygenation. The process begins with inserting venous cannulas into the right side of the heart to draw blood passively into a reservoir, using gravity based on the height difference between the patient and the reservoir. The blood is then pumped through an oxygenator, where it is oxygenated and transformed into blood suitable for systemic circulation. The oxygenated blood is split into 2 streams: 1 stream is returned to the patient via an aortic cannula inserted into the distal ascending aorta, while the other stream, mixed with a cardioplegia solution, is delivered to the aortic root via a cardioplegia pump. This separation ensures that the heart receives only the cardioplegia solution, causing arrest, while the rest of the body receives oxygenated blood.
Cross-clamping the aorta is crucial for intracardiac repair as it induces ischemia in the heart. Cardioplegia, a myocardial protection method, involves perfusing the heart with a solution to cause electromechanical arrest, thereby reducing myocardial oxygen consumption. The cardioplegia cannula is inserted proximally, while the aortic cannula is placed distal to the clamp. Cardioplegia is delivered via a separate pump, either antegrade into the aortic root, retrograde into the coronary sinus, or both. A transesophageal echocardiogram can guide the placement of the balloon-tipped retrograde cannula into the coronary sinus. Retrograde cardioplegia alone is insufficient for right ventricle protection. However, it may be necessary in addition to antegrade or ostial cardioplegia when aortic insufficiency is present. With aortic insufficiency, antegrade cardioplegia may leak through the incompetent valve, leading to inadequate cardiac protection due to insufficient solution delivery and myocardial stretch of the left ventricle. In such cases, retrograde cardioplegia may also be used. Ostial cardioplegia is administered in cases of severe aortic regurgitation.[10]
CPB also includes mechanisms to adjust the blood's chemical composition and temperature via a heat exchanger, ensuring the patient's metabolic needs are met. Throughout the procedure, cardiotomy suckers collect and salvage any blood lost during surgery, minimizing the need for transfusions. Cardiac vents maintain optimal cardiac pressures and prevent heart enlargement. Once the surgical procedure is complete, the aortic cross-clamp is applied to isolate the heart from the rest of the circulation, enabling the surgeon to work on a bloodless field. The CPB machine's careful coordination of these functions ensures continuous perfusion of vital organs and protection of myocardial tissue during the surgery, maintaining patient stability and viability throughout the procedure.
The following is an example of how CPB is conducted in the operating room:
Going "On Bypass"
The surgeon performs arterial and venous cannulation and then connects the arterial and venous cannulas to the pump. Connecting the arterial cannula first is beneficial for several reasons, with one being that it allows the patient to transfuse volume into circulation if they become hemodynamically compromised. Venous cannulation can lead to atrial irritation and supraventricular arrhythmias, such as atrial fibrillation, which may be poorly tolerated in certain heart conditions like left ventricular hypertrophy or aortic stenosis. An atriotomy for the venous cannula will also lead to blood loss that could compromise the patient. With the arterial cannula ready and connected, the surgeon can quickly correct this by instructing the perfusionist to transfuse the volume.
Once the connections are satisfactory, the surgeon asks the anesthetist and the perfusionist if they are ready to go on bypass. If all is well, they give the go-ahead order to go "on bypass." As both sides of the circuit are in continuity, the surgeon must "divide the lines." Before doing so, the surgeon must confirm 2 things with the perfusionist:
- The pump is off.
- If not, the pump will push against a closed clamp, potentially causing machine breakage.
- The venous line is clamped.
- If not, the fluid in the venous line will siphon back into the reservoir.
Before connecting the lines to the cannulas, the surgeon instructs the perfusionist to:
- Push some fluid in the arterial cannula to de-air the connection completely (ie, "come around").
- Pull back some fluid in the venous cannula, reduce tube length, and ensure it sits properly.
After the surgeon connects the arterial line tube to the aortic cannula, they confirm:
- Good swing
- Ensuring the cannula is in continuity with the bloodstream (ie, inside the aorta)
- Good pressure
- Ensuring the cannula is not in an inappropriate site (eg, back wall, dissection lumen)
An example of a typical dialogue during this part of CPB is:
- Surgeon: ACT ok?
- Anesthetist: ACT satisfactory.
- Surgeon: Cannulating (The anesthetist could instruct the surgeon to wait if pressure is high.)
- Anesthetist: Go ahead.
- Surgeon: Dividing the lines.
- Perfusionist: Off and clamped.
- Surgeon: Connecting arterial line (A-line), come around, please, stop; the A-line is connected.
- Perfusionist: Good swing and pressure.
- Surgeon: Cannulating atrium, return losses, please.
- Perfusionist: Transfusing.
- Surgeon: Take back, please; connected, ready to go on bypass
- Perfusionist/anesthetist: All good.
- Surgeon: On bypass, please.
Confirming Satisfactory Bypass
Confirming satisfactory CPB involves several key steps to ensure the patient is stable and that the bypass circuit functions correctly. By meticulously checking these parameters and maintaining clear communication among the surgical team, perfusionist, and anesthesiologist, satisfactory CPB can be confirmed, ensuring the safety and stability of the patient throughout the surgical procedure. These steps include:
- Adequate venous drainage
- Ensure the venous cannula is properly positioned and draining blood into the reservoir. This is typically confirmed by observing a steady blood flow into the venous reservoir without signs of air or excessive resistance.
- Arterial line pressure
- Verify that the arterial line pressure is within the normal range. This indicates that blood is adequately pumped from the oxygenator to the patient's arterial system. Proper arterial cannula placement prevents complications like dissection or inadequate perfusion.
- Oxygenation and blood gases
- Regularly check blood gas measurements and oxygenation levels to confirm that the oxygenator effectively oxygenates the blood and removes carbon dioxide. The blood gas values should be within the expected physiological range.
- Hemodynamic stability
- Monitor the patient's vital signs (including blood pressure, heart rate, and central venous pressure) to ensure they remain stable. Hemodynamic parameters should indicate adequate perfusion of vital organs.
- Flow rates
- Assess the pump's flow rates to ensure they match the calculated patient's size and condition requirements. The flow rate should be sufficient to maintain systemic perfusion without causing hemodilution or other issues.
- Temperature management
- Check the temperature of the blood returning to the patient to ensure the heat exchanger appropriately regulates it. The temperature should be maintained within a safe range to avoid hypo- or hyperthermia.
- Visual inspection
- Perform a visual inspection of the entire CPB circuit to ensure no leaks, air bubbles, or malfunctions are present. Ensure all connections are secure and that the circuit is operating smoothly.
- Communication with surgical and anesthesia teams
- Constant communication with the surgical and anesthesia teams is crucial to ensure that all members know the CPB status and any potential issues. The surgeon should confirm good arterial line swing and pressure, indicating proper placement and function.
- Cardioplegia delivery
- Ensure that the cardioplegia solution is being delivered appropriately to achieve myocardial protection. Verify that the heart is adequately arrested and protected during the procedure.
Weaning Off Bypass
Weaning off CPB is a step-by-step reversal of the bypass process, ensuring the patient's heart and lungs gradually resume normal functions. Here's how the weaning process typically unfolds:
Step 1: Restarting the Heart and Lungs
The first step in weaning off bypass involves resuming the heart's electrical and mechanical activity and allowing blood to flow to the lungs. This enables both organs to function partially while the pump is still running. The heart is restarted by rewarming, de-airing, and placing epicardial pacing (discussed in a separate chapter). Lung reperfusion occurs simply by re-ventilating the lungs.
- Rewarming
- Rewarming is essential to reestablish the metabolism of cardiac myocytes. Due to the physical properties of body fluids, this process takes longer (0.3-0.5 °C/min) than the cooling process (0.5-1.5 °C/min). Rewarming is achieved systemically via the heat exchanger and using a "bear hugger" to warm the lower extremities. Rewarming must not happen too quickly to avoid creating microbubbles (Boyle law) and not overheating to prevent the denaturation of plasma proteins.
- De-airing
- De-airing is a critical step in the weaning process that aims to expel all air from the heart and great vessels before allowing the heart to control circulation independently. Residual air in the heart and aorta can embolize any organ and cause severe damage. Air embolizing of the coronary or carotid arteries is of particular concern, as these are the first branches of the aorta. The right coronary artery is especially vulnerable to air embolism due to its higher anterior position. If air embolizes down the right coronary artery, it can cause right ventricular distension.
- The CPB pump manages air particles through maneuvers such as escalating pump flow and increasing pressure to expel air down the system. In severe cases, more drastic measures may be required, such as going back on bypass or conducting antegrade/retrograde cerebral perfusion. Ensuring satisfactory de-airing before dismantling the circuit is essential.
- When the heart is fully decompressed, the distance from the venous cannula to the cross-clamp, including the right heart, pulmonary arteries, lung parenchyma, pulmonary veins, and left heart, should be free of blood but will contain some air. This air is exaggerated by surgical breaches (eg, CABG) since they allow ambient air into the space. Sources of air entering this space during cardiac surgery include surgical (atriotomy, aortotomy, cannulation site), anesthetic (central venous catheter line), CPB pump (exhaustion of reservoir level, unsecured stock ports, cavitation), and natural dead space.
- Lung reperfusion
- The lungs are reventilated to resume their function, allowing blood to flow through the lungs.
Step 2: Confirming Heart and Lung Function
The surgeon must confirm the function of the heart and lungs by examining specific parameters, such as arterial blood gas and cardiac output. These parameters ensure that both organs function properly before fully weaning off CPB. The following is a summary of the parameters.
- “No” x 2
- No conditions include graft failure, valve leakage, dissection, and no residual air.
- "Satisfactory" x2
- These are satisfactory pacing and ventilation.
- "Physiological" x2
- These are the physiological temperature (35-37 °C) and physiological gases (arterial blood gases, potassium [K+], PO2).
Step 3: Gradual Weaning from the Pump
If the heart and lung functions are satisfactory, the surgeon instructs the perfusionist to slow down the pump until it is completely off gradually. The perfusionist starts by gradually clamping the venous line, limiting the amount of blood returning from the patient. This causes more blood to flow into the patient than returns, effectively filling the heart. This process continues until a satisfactory contraction is achieved, reaching the highest point of the Frank-Starling curve. At this point, the perfusionist begins to slow down the main head pump's flow as instructed by the surgeon. This limits the blood flowing back to the heart until the venous line is fully clamped and the main head pump is entirely switched off. The arterial and venous lines are clamped, and the lungs and heart functions are monitored for a few more minutes to ensure stability.
Step 4: Dismantling the Circuit
At the end of the operation, heparin is reversed by administering protamine (1 mg/100 units of heparin given). Protamine, derived from salmon sperm, reverses heparin anticoagulation by forming 1:1 complexes with the negatively charged heparin molecules. Protamine administration can be associated with adverse effects such as hypotension, pulmonary vasoconstriction, bronchoconstriction, reduced cardiac output, and anaphylaxis. The risk of hypotension is particularly dependent on the rate of administration.
The surgeon dismantles the CPB circuit only if the heart and lung functions are confirmed to be normal. This is done stepwise in the following order. Venous cannula out (but leave the purse string intact), root vent out, then aortic cannula out (after giving protamine and satisfactory filling). Throughout the procedure, the surgeon keeps an eye on the heart parameters, bearing in mind the situation might necessitate returning to the bypass at any time; certain precautions are taken to enable that. Fill the venous line with crystalloid to reprime it (siphon venous line). The perfusionist checks the heparinization, occlusion, and reservoir levels. The surgeon leaves the atrial purse strings ready to reuse if needed.
Complications
CPB is a crucial technology in cardiac surgery but is also associated with various complications that can affect patient outcomes. One significant complication is systemic inflammatory response syndrome, triggered by blood contact with the nonendothelial surfaces of the CPB circuit. This response releases inflammatory mediators, causing fever, leukocytosis, and capillary leak syndrome. Pharmacological strategies with antioxidant properties show promising potential in mitigating these issues, particularly in reducing complications, such as vasoplegic syndrome during CPB.[6]
Another critical issue is coagulopathy, often characterized by platelet dysfunction and consumption of clotting factors that can lead to bleeding complications. Additionally, CPB is associated with neurological complications such as stroke, which can result from emboli, hypoperfusion, or inflammatory responses affecting cerebral blood flow. Other complications include acute kidney injury due to altered renal perfusion, electrolyte imbalances, and the potential for transfusion-related complications like hemolysis or infection. Vigilant management and advanced techniques aim to mitigate these risks and improve patient outcomes in cardiac surgery.
Clinical Significance
CPB holds profound clinical significance in modern cardiac surgery, enabling intricate procedures that are otherwise impossible. CPB allows surgeons to perform precise repairs and interventions with minimal intraoperative bleeding by creating a bloodless and motionless environment for the heart. This technology ensures continuous oxygenation and circulation of blood throughout the body, sustaining vital organ function during surgery. CPB plays a crucial role in treating complex cardiac conditions such as congenital heart defects, coronary artery disease, and valvular heart disease, thereby improving patient outcomes and extending lives. However, it also presents challenges, including potential complications—many of which can be life-threatening. Because of the risks, CPB requires vigilant monitoring and management for optimal patient safety and recovery. To reduce the risk of complications from CPB, many surgeons also perform off-pump heart surgery.[11][12][13][14]
Enhancing Healthcare Team Outcomes
Effective CBP management involves a multifaceted strategy that includes advanced skills, strategic planning, interprofessional communication, and seamless care coordination. Physicians and surgeons must be adept at CPB techniques and equipment, making real-time decisions and managing complications. Advanced practitioners and nurses are essential for preoperative patient assessments, intraoperative monitoring, and postoperative care. They ensure patient stability and support the surgical team with their expertise in pharmacologic management and CPB machinery. Pharmacists optimize medication management, particularly the dosing of anticoagulants and reversal agents, and monitor for adverse reactions. Perfusionists, crucial for operating the heart-lung machine, must meticulously manage the blood flow and oxygenation. Clear and effective communication among these professionals ensures that critical information, such as patient status and procedural steps, is shared promptly to enhance patient safety and outcomes.
Care coordination is essential for the success of CPB and involves preoperative planning, intraoperative management, and postoperative care. Preoperatively, thorough patient assessments and team discussions help identify potential risks and develop individualized care plans. During surgery, constant communication ensures every team member knows the procedure's progress and any necessary adjustments. Postoperatively, coordinated care involves monitoring and managing patient recovery, swiftly addressing complications, and rehabilitation planning. This collaborative approach improves team performance and enhances patient-centered care by ensuring that each patient receives the most appropriate and effective treatment, optimizing outcomes, and ensuring patient safety.