Continuing Education Activity
Breast augmentation is a surgical procedure where the breast size is enhanced. Augmentation can be from the placement of an implant, or less commonly, thru fat transfer. Breast augmentation is one of the most commonly performed plastic surgery procedures in the United States. The FDA put a restriction on silicone filled implants for cosmetic enhancement starting in 1992. However, most reconstructive patients continued to receive silicone implants after mastectomy. This ban was due to concern over the risks of silicone implants which has now been resolved. This activity describes the indications, contraindications, and complications of breast augmentation and highlights the role of the interprofessional team in the pre and postoperative management of these patients.
Objectives:
- Identify the different techniques of breast augmentation.
- Describe the indications for breast augmentation.
- Review the complications of breast augmentation.
- Outline the importance of improving care coordination among interprofessional team members to improve outcomes for patients undergoing breast augmentation.
Introduction
Breast augmentation is a surgical procedure where the breast size is enhanced. Augmentation can be from the placement of an implant, or less commonly, through fat transfer. Breast augmentation is one of the most commonly performed plastic surgery procedures in the United States. The FDA put a restriction on silicone-filled implants for cosmetic enhancement starting in 1992. However, most reconstructive patients continued to receive silicone implants post-mastectomy. This ban was put in place following concern over the risks of silicone implants. Extensive research and clinical trials did not confirm those fears of silicone. After many studies had failed to show silicone linked to diseases, the FDA, in 2006, again allowed silicone-filled implants to be used by any patient without requiring them to be enrolled in a clinical study. In 2017, the majority of patients undergoing breast augmentation received cohesive gel silicone implants. The FDA also recommends MRI screening every 2 years in patients with silicone implants to detect subclinical implant leaks. However, patients and their physicians do not always adhere to this recommendation, and MRI scans can also have false-positive readings. The gel in current implants is more cohesive than previous implants and even shaped, or form-stable implants have been increasing in use. These may have lower complication rates, but further evaluation is ongoing. Recently, implant makers have been introducing different levels of cohesive gel in their products. The higher or more cohesive the gel, the more firm or "gummy" the implant will be. This may lead to lower rupture rates of implants. But eventually, all implants will likely eventually rupture or break.[1][2][3]
Anatomy and Physiology
The female breast is located on the anterior chest wall inferior to the clavicle with the sternum medially and the edge of the latissimus dorsi muscle laterally. The inferior border is the inframammary fold (IMF) also referred to as the inframammary ligament. This fold is a dermal structure formed by the fusion of the superficial and mammary fascia. The pectoralis major and minor muscles form the posterior or bottom boundary of the breast with the breast parenchyma superior. The blood supply is from the subdermal plexus of vessels with major contributions from the internal mammary artery, the external mammary artery, and the intercostal perforators. The major nerve supply is via the intercostal plexus with most contributions from the third through fifth intercostal nerves.
Indications
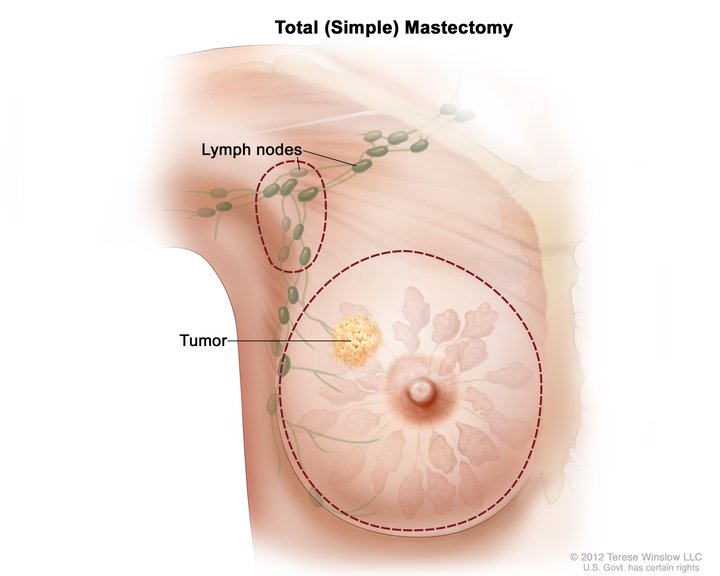
Patients get implants for reconstruction after mastectomy as well as developmental disorders, or for elective reasons for enhanced self-image. Hypomastia may be from normal development or involution, especially after pregnancy. Patients from all different personality types and spectrums may seek this procedure to help with their self-image or esteem. When surveyed after surgery, the vast majority of women would undergo the operation again.[4]
Contraindications
Most patients do not have contraindications to breast augmentation. But these include active infection of the breast, active cancer, pregnancy, history of autoimmune disease, current radiation treatment, unstable medical conditions, or known sensitivity to silicone. Patient psychological instability or patients with unrealistic expectations also should not have this surgery.[5][6]
Equipment
Basic operating room equipment is usually all that is required to perform a breast augmentation. Some surgeons prefer a lighted retractor to visualize inside the breast pocket created for the implant while some prefer using a headlight instead. If the umbilical or axillary approaches are used, then an endoscope or other specialized equipment may be needed. Some surgeons also recommend using a special implant sleeve to insert the implant. This may make the implant insertion easier and is part of the no-touch technique where minimal touching of the implant is allowed. This may decrease the risk of implant trauma and bacterial contamination.
Personnel
In most cases, the operating team will consist of the surgeon, an assistant who is scrubbed in surgery, an anesthesiologist, and a circulating nurse in the operating room.
Preparation
Patients are prepared for surgery as in any other surgical procedure.
Technique or Treatment
There are 2 main types of breast implants: saline-filled or silicone-filled, but both have an outer silicone shell. Saline-filled implants are filled with sterile saline. These implants are usually inserted empty and then a small port is used by the surgeon to add the desired amount of sterile saline to inflate the implant. The port is then removed, and the implant has a self-sealing tab for the port insertion site. Saline implants give the surgeon a large degree of variability to fill to different amounts as the implants will usually have a 25 to 50 mL range specified by the manufacturer. Some saline implants are filled by the surgeon during surgery while some manufacturers prefill other saline implants, but these prefilled saline implants are not commonly used in the United States.
The outer shell of the implant may be smooth or textured. Texturing is used in shaped implants and some round implants as well. The texturing helps prevent rotation in shaped implants and has been shown in some studies to lower the incidence of capsular contracture when the implant is placed in the subglandular pocket. Texturing does not seem to offer this decreased incidence of contracture when placed in the submuscular pocket. Saline implants are currently approved by the FDA for use in patients 18 years and older for breast augmentation and any age patient for breast reconstruction. Silicone-filled implants have an outer shell that is comprised of solid silicone. They are then filled inside with a viscous silicone gel. Silicone gel implants, as is also the case with saline implants, may have a smooth surface or a textured surface on the outer shell. Silicone gel implants are FDA approved to increase or enhance breast size in any patient over the age of 22. Many surgeons will still use the gel-filled implants "off-label" in patients under the age of 22 if they are indicated for the patient. Patients with small amounts of soft tissue coverage in their breasts will see the most benefit from a silicone implant as opposed to a saline implant that gives the silicone's softer or more natural feel. Also, in thin patients, silicone implants will show less rippling of the implant edges when compared to saline implants.
The implants can be placed above or beneath the pectoralis muscle. This is also referred to as subglandular and submuscular respectively. There are advantages and disadvantages to each approach. Patient anatomy, as well as surgeon preference, play a role in the decision. There is not one placement method that is uniformly accepted as the best location, and this should be determined by collaboration between the patient and the surgeon. Common access incisions include the inframammary crease, transaxillary, and the peri-areolar locations. General anesthesia is most common for this procedure, but it can also be done under sedation or even local anesthesia in select cases. Breast augmentation is considered an outpatient operation generally takes 45 to 90 minutes to perform. Recovery is usually rapid with a return to light work and activity within a week. Return to full activity may take up to 6 weeks.
Complications
The risk of complications is low; however, there are known potential problems, and no implant is considered a lifetime device.[7][8][9] Implants can rupture at any time or last a lifetime after placement. However, many surgeons will estimate a 15 to 20-year lifespan for the implants. Presently there is no established uniform recommendation to replace implants at a set time interval. Some surgeons will recommend routine replacement at 10 to 15 years after initial placement and others will recommend waiting until the implants break or deflate before replacing. Early postoperative complications include:
- Infection
- Scarring
- Asymmetry
- Hematoma
- Seroma
- Breast pain
- Poor cosmetic outcome
- Nipple/breast sensation changes
Later complications include:
- Implant malposition or displacement
- Implant deflation or leak
- Capsular contracture which is tightening of the tissue capsule around the implant
Surgeons do not know the specific cause of contracture, but many suspect a sub-clinical or low-grade infection that can lead to inflammation and a capsule biofilm that may initiate the contracture. The most commonly isolated microorganisms from studies on breast implant capsular contracture are Staphylococcus epidermidis and Propionibacterium acnes [10]. Capsular contracture is graded on a scale of 1 to 4, and if severe, it may require surgical correction or even implant removal. It is important for patients undergoing this procedure to understand that many women receiving breast implants may need more breast surgery at some point in their life. Recently, there have been reports that there is a slim possibility of women with breast implants being more likely to be diagnosed with anaplastic large cell lymphoma (ALCL). The exact relationship between implants and ALCL has not been determined yet, but it may be more common with a certain type of texturing on the implant.
Clinical Significance
Breast augmentation remains a highly popular procedure. The American Society of Plastic Surgeons (ASPS), reports that approximately 290,000 procedures were performed in the United States in 2016. The vast majority of patients have improved self-esteem and express satisfaction with their decision to have the operation. Given the number of women who have breast implants, doctors who treat these women for other conditions should have an awareness of the procedure and implants in general.
Enhancing Healthcare Team Outcomes
Although breast augmentation surgery has a low risk of acute complications, it is imperative to make all attempts to minimize any risks. Over the years, many litigations have resulted primarily due to the lack of informed consent. The pre-operative visit conducted by a nurse can help ensure that all post-operative care instructions are understood and followed. Patients should be instructed to discontinue smoking and make a positive change in lifestyle so that the results of the surgery will last a long time. Patients who follow their given post-operative instructions will likely have a lower rate of complications. Also, pharmacists can play a role in the care of a breast augmentation patient by ensuring that patients have no allergies to their prescribed medicines and by instructing patients on their proper use. This may help decrease the rate of infections or assist patients in their postoperative pain control. Interprofessional care provided to the patient may also help to identify any potential problems earlier. Patients should not be offered unrealistic expectations but also told about the potential for an iatrogenic complication. Earlier awareness of a complication can lead to quicker treatment and a better eventual outcome.[11] (level III)
Outcomes
Of all the cosmetic procedures, breast augmentation results in outstanding results. The majority of patients not only are pleased with the outcome but develop more self-esteem and confidence. The rate of complications after breast augmentation is low and varies depending on surgeon experience. Surveys intact that about 70-80% of patients are satisfied and feel that the outcome was perfect. [2][12](Level V)