Continuing Education Activity
Lower blepharoplasty is one of the most common aesthetic facial surgeries. It aims at improving the appearance of the eyelid and the periorbital region. There are many techniques described for lower blepharoplasty. All of them address the laxity of the lower eyelid and provide the necessary canthal support, if needed, to maintain long-term results. This activity reviews the indications and the different surgical approaches by the interprofessional team for canthal support during lower blepharoplasty.
Objectives:
- Understand the anatomy and aging process of the lower eyelid and their relevance when assessing lower blepharoplasty patients.
- Describe how to assess lower eyelid laxity and lateral canthus dystopia in lower blepharoplasty patients.
- Identify indications and contraindications for performing lateral canthal support in lower blepharoplasty patients.
- Review different surgical techniques described for lateral canthal support and their limitations when performing lower blepharoplasty.
Introduction
Lower blepharoplasty is one of the most common facial plastic surgery. It aims to improve the appearance of the lower eyelids by addressing skin laxity, fat prominence, and adjusting the lower eyelid position. A good understanding of anatomy and careful preoperative counseling of the patient is crucial for success. Lateral canthal support is used to address the lower eyelid laxity either by performing canthopexy or canthoplasty. This activity reviews anatomy of the lower eyelid, preoperative assessment, common lower blepharoplasty techniques, and highlights different methods of lateral canthal support.[1][2]
Anatomy and Physiology
A thorough understanding of the anatomy of the eyelid and the periorbital area is crucial for successful lower blepharoplasty surgery. Surgeons must understand the effect of surgical rearrangement on eyelids' function, shape, and position. Solid anatomical knowledge and understanding of the aging process help surgeons minimize these complications and achieve optimal results.[3]
The skin of the eyelid is the thinnest in the body. There is a clear distinction between the thin eyelid skin, which lacks any subcutaneous fat, and the thicker cheek skin with well defined subcutaneous layer. The lower eyelid is divided into two lamellae. The anterior lamella is formed of skin and orbicularis oculi muscle, whereas the posterior lamella includes trasoligamentous sling, capsulopalpebral fascia, and conjunctiva. The septum is referred to as the middle lamella as it separates the anterior and posterior lamella. The grey line is a central fine line that serves as a guide for identifying the dissection plane between anterior and posterior lamella.[2]
The palpebral fissure is the interval between the eyelid margins. When lids are open, it measures around 30mm in the horizontal plane and 10 mm in the vertical plane. The lower eyelid is situated at or 1 mm above the lower limbus, while the upper eyelid covers 2 mm of the upper limbus. The commissures are the junction points between the upper and lower eyelid, and they create medial and lateral angles representing medial and lateral canthus, respectively.[3]
In most patients, the lateral canthal angle is positioned at 2 mm superior to the medial canthal angle. If a line is drawn between medial and lateral canthi, it will show an upward inclination to the lateral side. This is called positive canthal tilt. A negative canthal tilt is present when the medial canthus is superior to the lateral canthus. This should be carefully examined and highlighted to the patient in the initial preoperative visit. Negative canthal tilt is associated with a high risk of postoperative eyelid malposition. Therefore, lateral canthal support either in the form of canthopexy or canthoplasty is needed for such cases. Another factor that may lead to poor postoperative results has a negative vector. These patients with prominent globe exceeding the maxilla in the midline sagittal plane are also at a higher risk of lower eyelid malposition.[4]
Scleral triangles are the visible parts of the sclera on both sides of the cornea. They are bound by the upper lid margin, lower lid margin, and corneoscleral limbus. The apex of the triangles is the medial and lateral canthal angles. The size of the medial scleral triangle is constant. In contrast, the larger lateral scleral triangle varies with the changes in the lower eyelid position, and it is the primary determinant of eye shape. Patients should be preoperatively counseled about the shape of scleral triangles and how surgery can affect them. The lower eyelid crease is less well-defined compared with the upper eyelid crease. It is mainly formed by the dermal insertion of lower lid retractors. It is situated 5mm from the medial lid margin and slopes slightly towards the lateral side.[5]
Muscle
Orbicularis oculi muscle lies immediately beneath the skin and is the main protractor of the eyelid. It can be subdivided into three parts: pretarsal, preseptal, and orbital part. The pretarsal and preseptal parts cover the tarsus and the spetum, respectively, while the orbital part extends from the eyelid to cheek, temple, and forehead. The capsulopalpebral fascia and inferior tarsal muscles are the main retractors of the lower eyelid. They are analogous to the levator aponeurosis and the Müller's muscle in the upper eyelid.[4]
Tarsus
The tarsal plate is part of the posterior lamella. It forms the tarsoligamnetous sling along with the canthal tendons. This represents the main skeleton of the eyelid. Orbicularis oculi muscle is firmly attached to the anterior surface of the tarsus while the conjunctiva is fixed to its posterior part. It usually becomes lax with aging, which leads to distraction of the eyelid from the globe. The lower eyelid tarsal plate is around 25 mm long, 1 mm thick, with a height of 4 mm. It attaches to the medial and lateral orbital walls by canthal tendons. Both canthi are made up of anterior and posterior reflections. The medial canthus reflections attach to the anterior and posterior lacrimal crest. While the anterior reflection of the lateral canthus inserts in the lateral orbital rim and the posterior reflection inserts on the Whitnall's tubercle 5 mm from the lateral orbital rim.
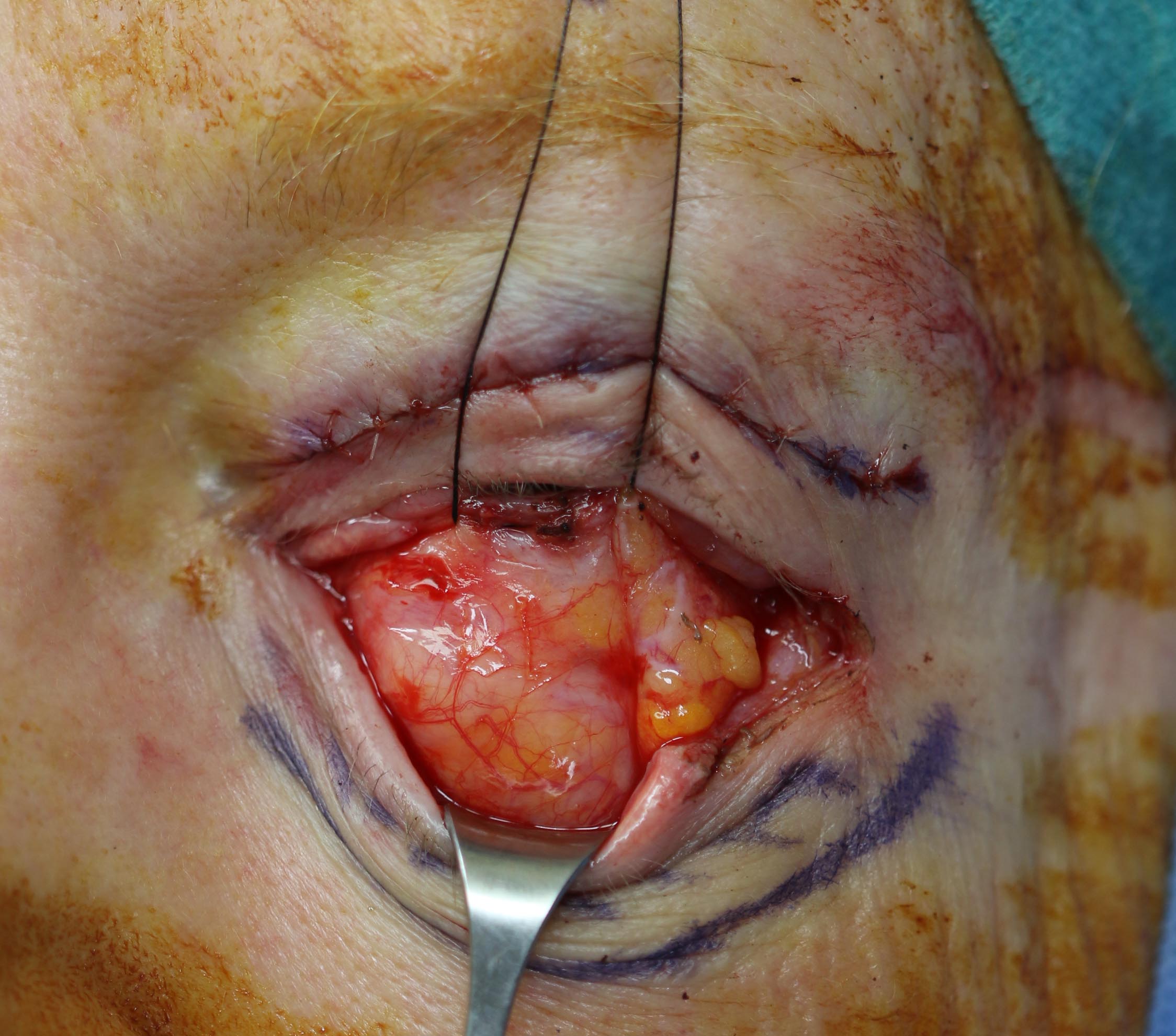
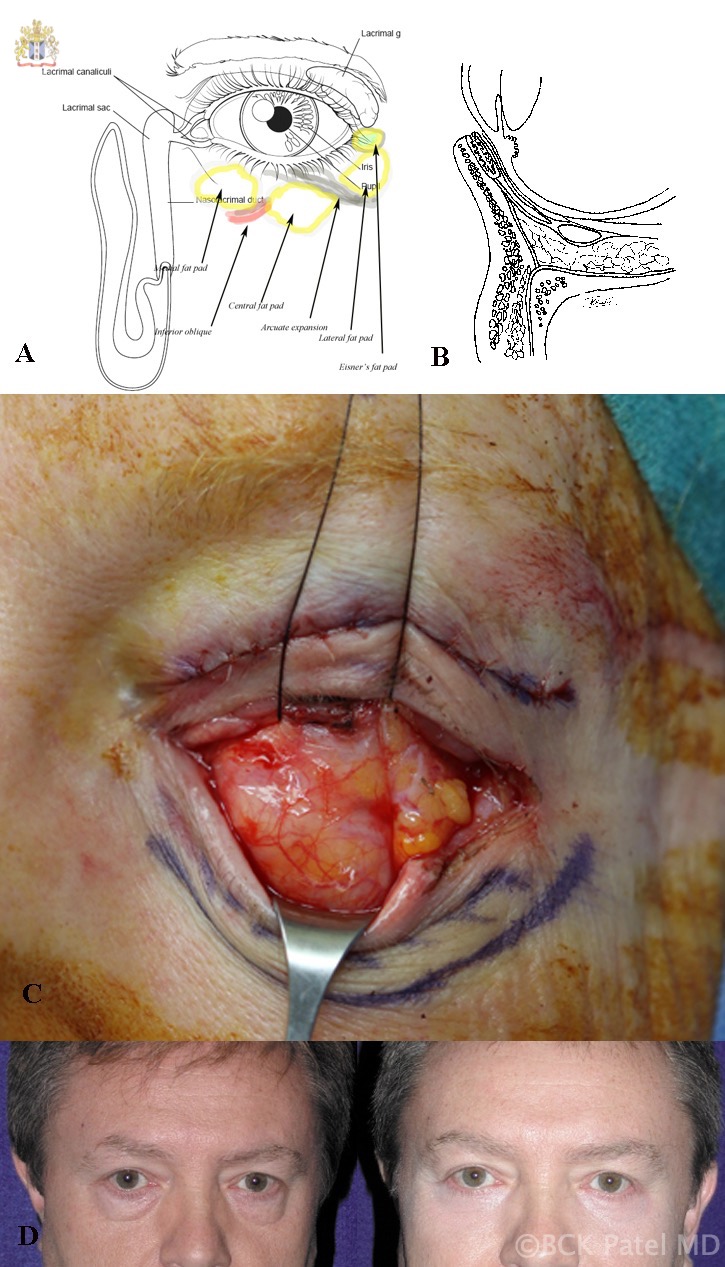
Postseptal Fat Compartment and Midface Fat
There are two post-septal fat compartments in the upper eyelid (central and nasal fat pad) and three compartments in the lower eyelid (nasal, central, and temporal fat pads). In the lower eyelid, the nasal compartment is partially separated from the central compartment by the inferior oblique muscle. Care should be taken not to inadvertently stitch the inferior oblique as this may lead to postoperative painful diplopia, requiring urgent surgical intervention. The central and the temporal fat pad is divided anteriorly by the arcuate expansion.
In addition to the post-septal fat pads, two extra fat compartments exist in the mid-face. Suborbicularis oculi fat (SOOF) lies deep to the orbicularis oculi muscle in the preperiosteal membrane, anterior to the orbital rim. It becomes atrophied and ptotic by age which exposes the infraorbital rim. It is thinner at the anterior nasolacrimal crest and thicker in its temporal part. This layer is encountered during suborbicularis dissection below the level of the inferior orbital rim. The septum separates SOOF from orbital fat, and the orbicularis oculi muscle separates it from the malar fat pad. The ROOF (Retro-orbicularis Oculi Fat pad) is similar to the SOOF. It is present in the upper eyelid deep to the orbicularis oculi muscles and superficial to the orbital fat pad. With the aging process, it becomes atrophied and contributes to eyebrow ptosis, which can be corrected during a brow lift.[6]
Conjunctiva
In the lower eyelid, the inferior conjunctival fornix is 10mm from the lower eyelid margin. This is relatively constant during eye closure as the main movement is from the upper eyelid.
Blood Supply and Lymphatic Drainage
The eyelids have a complex, rich vascular network. It is formed by anastomosis between both external carotid and internal carotid arteries. Branches of the ophthalmic artery(internal carotid artery) connect to the terminal branches of the facial artery, internal maxillary, and superficial temporal arteries (external carotid artery). This forms two arcades in the lower eyelid and three arcades in the upper eyelid.
Most of the blood flow comes from nasal anastomosis, which is the main cause of postoperative hematoma. The lower eyelid arcades are situated 3.8mm from the eyelid margin. Therefore, it is important to place a blepharoplasty incision at least at 4mm from the ciliary margin to preserve these arcades. This maintains a robust blood supply to the lid, and the surgeon can then safely interrupt the blood supply laterally if needed, e.g., in cases that need canthoplasty. Venous drainage occurs through an anastomosis between superficial facial veins (mainly the facial vein) and deep orbital veins (mainly superior ophthalmic veins). The orbital veins have no valves. Any infection in the "triangle of death" (apex is the mid-forehead, passing across the two medial canthi, and the base is the mid nasal dorsum) can easily spread to the cavernous sinus. The lymphatic drainage of the lower eyelid follows different lymphatic channels according to its site. Medial lymphatics drain the lower eyelid, medial canthus, and conjunctiva and go to the submandibular glands. The lateral lymphatics drain the lateral canthus and upper eyelid to the superficial parotid lymph nodes.[4]
Nerve Supply
The sensory supply of the inferior eyelid is mainly through the maxillary division of the trigeminal nerve (V2), while the upper eyelid's sensory innervation is through the ophthalmic division (V1). The maxillary division becomes the infraorbital nerve in the posterior orbit which then emerges through the infraorbital canal, while the ophthalmic division divides into supratrochlear and supraorbital nerves. These three nerves are the target for anesthetic neve block. Orbicularis oculi receive motor innervation through various branches of the facial nerve, including frontal, zygomatic, and buccal branches. The majority of the nerve supply comes from the medial side of the orbicularis.[4]
Aging Process
With aging, the skin of the lower eyelid loses its elasticity which leads to folding and redundancy (dermatochalasis). Loss of integrity of the orbital septum causes herniation of fat compartments in the lower eyelid. Laxity of the lateral canthal tendon affects the lower eyelid position and the shape of the palpebral fissure. Patients with a prominent globe may exhibit a round palpebral fissure with increased lateral scleral triangle and potential scleral show. In contrast, in patients with a shallow globe, both the palpebral fissure and the lateral canthal triangle narrow. Moreover, The tarsoligamentous laxity affects the tone and behavior of the orbicularis oculi muscle. It often atrophies by age which may eventually lead to ectropion and watery eyes. Less commonly, hypertrophy of the orbicularis oculi can be seen, especially in the Asian population, which may predispose to entropion and smile lines.[7]
The aging change of the midface is related to the deflation of the fat compartments of the midface and the sagging effect of gravity. This can vary from mild aging changes confined to the lower eyelid to more significant changes affecting the lower lid, lid-cheek junction, and mid-face area. This can be presented as tear trough deformity, nasojugal groove, deepening of the nasolabial fold, and malar mounds. While early cases can be managed by blepharoplasty alone, more severe cases will need blepharoplasty and midface lift.[6][8]
Indications
Lower blepharoplasty is mainly done for cosmetic purposes. Most cases present with aesthetic problems in the form of dermatochalasis (excess lower eyelid skin) and steatoblephron (prolapsed fat pad). Functional problems are a less common indication when compared with upper blepharoplasty. All lower blepharoplasty cases should be evaluated for the need for canthal support either in the form of canthopexy or canthoplasty.[9]
Contraindications
Absolute Contraindications
Absolute contraindications include patients with unrealistic expectations or body dysmorphic disorders, a pathological eye condition that needs treatment first e.g. acute blepharitis, active myasthenia gravis, undiagnosed dry eye syndrome, and thyroid orbitopathy. Moreover, uncontrolled glaucoma and only one seeing eye are absolute contraindications of lower blepharoplasty.[10]
Relative Contraindications
Relative contraindications include a recent refractive procedure such as laser-assisted in situ keratomileuses (LASIK). Surgery should be delayed at least 6 months to allow time for the cornea to heal. Significant medical comorbidities such as heart failure or respiratory failure are another relative contraindication. However, surgery can still be done under local anesthesia. A high dose of anticoagulation and uncontrolled hypertension put the patient at a higher risk for retrobulbar hematoma and surgery should be postponed until medical optimization.[11][12]
Equipment
Standard blepharoplasty set should include:
- Marking pen
- Tetracaine hydrochloride (0.5%) eye drops
- Local anesthesia such as lignocaine 1% with adrenaline 1:100000
- Measuring gauge
- Corneal shield (optional) and lubricant to protect the cornea
- Blade handle
- Fine toothed tissue forceps (Bishop)
- Small dissecting scissors (Westcott)
- Small retractors (Desmarre retractor), preferably to be insulated
- Insulated bipolar forceps and needle tip cautery (Barraquer or Castroveijo)
- Cotton-tip applicator
- Fine periosteal elevator (Freer or Cottle)
- Fine needle holder
- Sutures (6-0 polyglactin, 6-0 polypropylene, and 4-0 silk for traction)
Chlorhexidine preparation should be avoided around the eyes as it can lead to serious corneal complications.[13]
Personnel
Lower blepharoplasty with canthal support can be done either as a well-equipped surgical theatre or in an office-based setting. It can be done under general anesthesia or local anesthesia with sedation. It should be done by a board-certified plastic surgeon or an oculoplastic surgeon. The operating surgeon must choose his preferred method of anesthesia and which theatre setting he would prefer to give the patient the best outcome. The team should also include a scrub nurse familiar with the used surgical set, a surgical assistant to help with retraction and stitch cutting, and an anesthetist in cases that need general anesthesia.[2]
Preparation
Lower eyelid blepharoplasty patients usually present with certain cosmetic complaints such as wrinkled skin or puffiness in the eyelid. Surgeons should address these complaints by performing a physical examination to assess the patient's motives, expectations, and age-related changes that need to be addressed by surgery. First of all, surgeons should ask about patients' motives for surgery and make sure that it is their own decision and not forced by someone else, e.g., a partner or a friend. It is also crucial to address the patient's expectations. Surgery should be deferred in any patient with unrealistic expectations. Body dysmorphic disorders are another contraindication of surgery. Moreover, patients should be asked about a history of dry eyes. A Schirmer test can be done if needed to quantify the degree of dryness. Visual acuity should be checked preoperatively, and eye movement in all field gazes should be documented. Patients should also be tested for Bell's phenomenon.[2]
Focus examination should include assessing the lower eyelid skin, orbicularis oculi muscle, tarsoligamentous laxity, herniated fat compartments, conjunctiva, eye shape, canthal tilt, eye prominence, and malar area. At the end of the examination, surgeons should decide which patient would benefit from non-surgical rejuvenation, lower blepharoplasty with or without canthal supports, or would need both lower blepharoplasty and mid-facelift. The surgical decision should be discussed with the patient in detail, including the recovery period and possible complications to obtain informed consent.[14]
Skin Assessment
Dermatochalasis, which is excess skin, muscle, and fat, is the most common indication for surgery. Skin wrinkles can be either dynamic or static. Dynamic wrinkles appear only when smiling, and they can be addressed by botulinum toxin injection.[15]
On the other hand, static wrinkles are always present and not related to smile. They need special care with either dermal filler, laser, or chemical peels. Dark eye circles resulting from a shadow of the convexity of the prolapsed fat will improve by blepharoplasty. However, dark circles related to actual skin pigmentation will remain after surgery. This can be addressed postoperatively by intense pulsed light (IPL) skin lightening and hydroquinone treatment.[16]
Co-existing skin lesions such as xanthelasma can only be excised if lying within the area of skin excision. Patients should be informed that any lesions away from the surgical skin excision site cannot be removed during lower blepharoplasty. It is better to be done in another surgical procedure later. Associated eyelid diseases such as blepharitis should be identified and discussed with the patient. In the case of active inflammation, surgery should be postponed till it subsides.[14]
Orbicularis Oculi Muscle
Fullness in the lower lid may be a sign of hypertrophied orbicularis oculi muscle rather than a prolapsed fat pad. This is more common in Asian patients, and it is usually evident as an excessive bunching beneath eyelashes when the patient smiles or squints. Resection of a part of the orbicularis oculi, preserving the pretarsal muscle, may be needed to address this problem.[17]
Tarsoligamentous Laxity
Trasoliganemtous laxity can predispose scleral show, corneal exposure, and in some cases, ectropion. It can be assessed by a snapback test in which the patient's lower lid is pulled downward to determine the lid's elasticity. If the lid does not reposition immediately against the globe once the lid is released, it is a sign of tarsoligamentous laxity. It can also be evaluated by the lid distraction test in which the lower eyelid is gently pulled forward and away from the eye. A distraction of more than 6mm is a sign of significant tarsoligamentous laxity. Canthal support is needed in all cases of tarsoligamentous laxity.
Herniated Fat Compartments
The lower lid has three post-septal fat compartments named nasal, central, and temporal fat compartments. It is important to determine which fat compartment is more prominent and to document it with preoperative photography. Standard photography should be obtained in the form of 5 views with the patient in a seated position and an upright posture with no facial animation. Then, close-up views of the eyes should be done while closed, open at rest, in an upward gaze, and a lateral gaze.[18] The most commonly overlooked fat pad is the nasal pad. Orbital fat can be either excised or redraped over the inferior orbital rim after the release of the orbitomalar ligament to create a space for fat repositioning. Over resection of the orbital fat can lead to hollowness in the lower orbit that is usually difficult to correct.
Conjunctiva
Patients with loose conjunctiva (conjunctivochalasis) should be informed that they are at a higher risk of the common postoperative conjunctival edema and should be counseled about the possible need for plication or resection of the loose conjunctiva if needed.[9]
Eye Shape and Canthal Tilt
Most patients have a positive canthal tilt (lateral canthus is 2 mm superior to the medial canthus), which can be reversed by age. The patient should be asked to describe how they see their eye shape and its relationship to the lateral canthus. A review of an old photo is always helpful. The decision of correction of the canthal tilt should be discussed with the patient preoperatively.
Eye Prominence
Measurement of eye proptosis is important to determine the need for lateral canthal support. A Hertel exophthalmometer can be used. An eye position of 15 to 18 mm from the lateral orbital rim is considered within the normal range. A deep-seated eye is defined as less than 15 mm from the lateral orbital rim. A modified technique of canthopexy is needed in deep-seated eye patients by the placement of the sutures at the level of the inferior pupil deep within the orbit. On the other hand, a prominent eye protrudes more than 18mm from the lateral orbital rim. These patients are at a high risk of lower lid malposition, scleral show, and ectropion postoperatively. In mild cases, placement of the lateral canthus deeper in the lateral orbital wall at the level of the superior pupil may be sufficient. While in severe cases, the excessive elevation of the lateral canthus is not advisable as it may impair eye closure.[19]
Malar Prominence
Patients with prominent eyes and recessed malar prominence (negative vector) are at a higher risk of lower lid malposition. Canthal support is needed in all these patients. On the other hand, patients with prominent malar bone (positive vector) tend to have deep-seated eyes and narrow palpebral fissures postoperatively. These patients are at a higher risk of anterior malposition of the lower eyelid away from the globe. This can be addressed by the deep placement of lateral canthopexy sutures. Midface aging can be seen in the form of tear trough malar festoon or deepening of the nasolabial fold. A commonly seen problem, a tear trough is a midface crease that begins at the medial canthus and travels obliquely above the nasolabial fold. It is an early sign of aging, and it can also be seen earlier in patients with familial tendencies. It can be addressed by redraping the orbital fat over the inferior orbital rim after releasing the orbitomalar ligament.[6]
Technique or Treatment
Transcutaneous Approach
This includes a stairstep incision involving a subciliary incision followed by elevation of skin muscle flap after preserving the pretarsal muscles in place. This is followed by division of the orbitomalar ligament, pre-periosteal dissection, and incision of the orbital septum at the level of arcus marginalis. The herniated fat pad can be either excised or redraped to the malar region. Lateral canthal support is crucial to support the lower eyelid position. Excision of the skin can be done by pinching the excess skin. Care should be taken to limit excision on the medial side of the eye to avoid undue tension, which may lead to ectropion.[20]
Transconjunctival Approach
Transconjunctival lower eyelid blepharoplasty can be either done through a preseptal or transseptal approach. The transseptal approach provides direct access to the post septal fat, which facilitates either excision or repositioning after the release of the orbitomalar ligaments. Stretching the lower eyelid during exposure can aggravate the pre-existing tarsoligamentous laxity. Therefore, routine canthal support should be performed in these cases. Transconjunctival blepharoplasty mainly addresses herniated fat rather than skin laxity. Excess skin can be addressed by either skin pinch excision or postoperative laser treatment. Smoothening the lower eyelid appearance is one of the main limitations of the transconjunctival approach, as removing or tightening the orbicularis is not applicable.[21]
Lateral Canthal Support
The lower eyelid laxity should be carefully evaluated preoperatively. This can be assessed by the previously mentioned snapback and lid distraction tests. Choice of the method of lateral canthal supports depends on the degree of skin laxity and the globe position. Canthopexy is usually sufficient for mild degrees of lateral canthal laxity, while canthoplasty is more suitable for extensive lateral canthal laxity. The decision about which procedure to do is usually made intraoperatively. Canthopexy can be performed if the amount of laxity can be corrected by simply tucking the lower lid edges against the globe. However, canthoplasty is recommended in cases with extensive laxity.[22]
Technical Steps
Canthopexy
- Make a 5mm incision horizontally starting from the lateral canthus. This can be joined with the subciliary incision in cases of transcutaneous blepharoplasty.
- Deepen the incision to expose the lateral canthal tendon and lateral edge of the tarsal plate
- Dissect to expose part of the periosteum of the lateral orbital wall
- Double-armed sutures are passed through the lateral canthal tendon and then secured to the inner aspect of the lateral orbital wall. Double bites of the lateral canthus should be taken and secured to the lateral orbital wall periosteum as deep as possible.
- Suture the orbicularis muscle on top of the deep canthal sutures followed by skin suturing
Canthoplasty
- Make horizontal incision as previously described in canthopexy
- Deepen the incision to expose the lateral canthus and the lateral tarsal strip.
- Divide the lower limb of the lateral canthus tendon from the upper and the common canthal ligament to allow greater mobility.
- Separate the conjunctiva from the lateral tarsal plate to allow easy mobilization of the lateral canthus.
- Excision of the excess skin, orbicularis muscle, and conjunctiva
- Expose the lateral orbital periosteum and secure the sutures in the same manner previously described.
- Suture the orbicularis muscle and the skin.
Choice of the Level of Anchoring Suture
Choice of the level of the anchoring point depends on the eye prominence. The standard position is to secure it at the horizontal pupillary line. In cases of deep-seated eyes, the sutures should be secured deeper in the lateral orbital wall and at the level of the inferior pupil. However, in cases of prominent eyes with a negative vector, the suture should be placed at the level of the superior pupil. If downward retraction of the lower eyelid is still present after canthal support, a release procedure can be performed to elevate the lower lid position. This includes the release of the inferior retinaculum, lower eyelid retractors, and or capsulopalpebral fascia. This then can be supported by the insertion of a spacer such as acellular dermal matrix or ear cartilage.[23]
Choice of Suture Material
Most surgeons prefer to use non-absorbable sutures when doing canthal anchoring, e.g., double-armed 4-0 prolene suture with a small half-circle needle. Each arm of the suture should be secured in the desired position of anchoring. On the other hand, fewer surgeons prefer absorbable sutures such as 4-0 PDS. They argue that canthal anchoring sutures are not needed permanently, and using absorbable sutures prevents the risk of stitch sinus or infection. However, these complications are uncommon. In cases of canthoplasty, the upper and lower eyelid should be carefully and precisely aligned with 6-0 buried vicryl sutures to prevent canthal webbing.[24]
Postoperative Care
The patient should rest in bed with his head up for the first day after surgery. Regular use of cold compresses is highly recommended, especially in the first two days. Sutures are usually removed within one week. Moreover, any strenuous activity and heavy activities should be avoided in the first two weeks after surgery.[9]
Complications
Vision Threatening Complications
- Retrobulbar hematoma requires urgent orbital decompression. The incidence of retrobulbar hematoma is around 0.055% (1:2,000), and the incidence of subsequent blindness is 0.0045% (1 to 22,000).[25][26]
- Rupture globe either from direct trauma during surgery or from the local anesthetic injection.
- Corneal abrasion or ulceration can be treated with topical antibiotic drops.[27]
Lower Lid Malposition
This includes ectropion due to shortening of the anterior lamella, entropion due to shortening of the posterior lamella, and canthal rounding and canthal dystopia.
Over Resection or Under Correction of the Fat Compartments
In case of extensive resection of the fat pads, consider volume replacement such as dermis fat graft or fat transfer. Surgeons should be cautious with fat transfer as overcorrection may persist because of the high chance of survival of any transferred fat to the lower eyelid. In cases of under correction, further surgery is usually needed to address the excess fat.
Adnexal Injury
- Incarceration of the inferior oblique or inferior rectus muscles will lead to postoperative painful diplopia and may require another operation to release the entrapped muscle.[27]
- Dry eye syndrome is more common when combined upper and lower blepharoplasty is done, especially in patients who receive regular hormonal replacement therapy.
- Damage of the ciliary ganglion.[28]
- Early chemosis and edema are related to the inflammatory response after surgery. However, persistent interstitial chemosis may be related to lymphatic disruption and may require revisional surgery.[29]
- Transient lagophthalmos, especially if combined with upper blepharoplasty.[25]
Suture-related Complications
This includes stitch sinus, inclusion cyst, and granuloma.[25]
Unsatisfactory results or recurrence of symptoms are possible complications as well.[30]
Clinical Significance
Lower blepharoplasty with lateral canthal support aims to improve the appearance of the lower eyelid and the surrounding periorbita. Knowing the relevant anatomy, changes with the aging process, proper planning, and patient counseling is essential for a reliable and satisfactory outcome.
Enhancing Healthcare Team Outcomes
Lower blepharoplasty with lateral canthal support provides an excellent long-term outcome that can significantly improve patient self-esteem and confidence. To achieve these positive results, the operation should be performed by a team of experienced staff familiar with the procedure and its possible complications. This should include a facial plastic surgeon or oculoplastic surgeon, anesthetist, surgical assistant, and nursing staff. [Level 5]