Continuing Education Activity
Bladder stones are solid calculi that are primarily found in the urinary bladder. While often calcified, they may also be composed of non-calcific material. The incidence of bladder stones in Western countries is relatively low, but due to dietary differences, it is higher in developing countries. This activity outlines the evaluation and management of bladder stones and highlights the role of the interprofessional team in improving care for patients with this condition.
Objectives:
- Describe the causes of bladder stones.
- Explain how to evaluate for bladder stones.
- Identify the treatment options for bladder stones.
- Explain the importance of improving care coordination among the interprofessional team to enhance the delivery of care for patients with bladder stones.
Introduction
Bladder stones are solid calculi that are primarily found in the urinary bladder. While often calcified, they may also be composed of non-calcific material.[1][2][3][4][5] The incidence of bladder stones in Western countries is relatively low as they tend to be found more often in developing countries due primarily to dietary factors. The areas most affected are countries in the Middle East and North Africa as well as Thailand, Indonesia, and Myanmar. Bladder stones usually occur due to urinary stasis as in benign prostatic hyperplasia or neurogenic bladder but can also form in healthy individuals without anatomic defects, foreign bodies, strictures, or infections. The presence of upper urinary tract calculi does not necessarily predispose to the formation of bladder stones. Bladder stones result in specific symptoms and are a significant source of discomfort.
Etiology
Urinary stasis, such as benign prostatic hyperplasia (BPH) or neurogenic bladder disorder, is the primary cause of bladder calculi. Most such stones are newly formed in the bladder, although some may come from the kidneys either as a stone or a sloughed papilla. Stones originating from the kidney that are small enough to pass through the ureters can easily traverse the urethra unless there is significant bladder dysfunction or outlet obstruction. Stones that remain in the bladder will develop layers of additional stone material that may or may not be identical to the original core material.[6][7][8][9]
Any foreign body left in the bladder that is not spontaneously expelled will eventually form layers of stone material and develop into calculus. One example would be a surgical staple or permanent suture. This is why absorbable suture material is recommended whenever urinary surgery is performed.
A retained double pigtail stent will also form stone material if left in the urinary tract long enough. Another example would be a fragment from a Foley catheter balloon that "fell out" but had a balloon rupture with a retained fragment left in the bladder. For these reasons, it is important to inspect any Foley catheter that has been pulled out, or that has "fallen out" to make sure that there are no missing fragments that might develop into a stone. If this cannot be done or it appears there might be a missing balloon fragment, cystoscopy should be performed.
Foley catheters are associated with more bladder stones than intermittent catheterization. In one study of patients with spinal cord injuries, 36% developed bladder calculi over an eight-year period of follow-up. Improved urologic care of these patients reduced the bladder stone formation rate to about 10%.
Radiation therapy, schistosomiasis, bladder augmentation surgery, urethral strictures, and the presence of bladder diverticula are other predisposing factors to bladder stone formation.
Epidemiology
The overall incidence of adult bladder stones appears to be decreasing. This is due to the increased use of BPH medications such as alpha-blockers and 5-alpha reductase inhibitors (5-ARIs) throughout the world.
In general, adult men with BPH and bladder stones are more likely to have a history of nephrolithiasis, gout, lower urinary pH, and lower urinary magnesium levels than similar men with BPH but without bladder calculi. The presence of urinary tract infections and having a significant intravesical prostatic extension (BPH) are the clinical signs that are most closely associated with the development of bladder calculi.[10]
In children, the overall incidence also is decreasing, mostly due to better prenatal and postnatal care as well as a general improvement in neonatal nutritional support. Boys typically have more bladder stones than girls, are not associated with renal stone disease, and are relatively unlikely to return compared to renal stone disease where recurrences in children are relatively common.
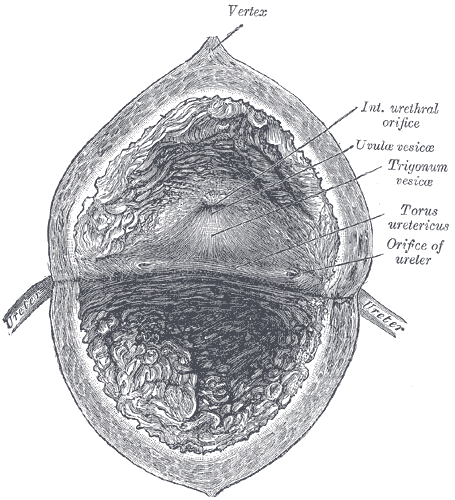
Pathophysiology
In adults, the most common bladder stone composition is uric acid, which accounts for about 50% of cases. Most patients who develop uric acid bladder stones do not have either gout or hyperuricemia. Other chemicals that form bladder stones include calcium oxalate, calcium phosphate, ammonium urate, cystine, and calcium-ammonium-magnesium phosphate (also called triple phosphate or struvite stones and are always associated with infection). Patients prone to chronic bacteriuria and urinary infections, such as those with spinal cord injuries or severely hypotonic bladders, tend to develop struvite (infection) and calcium phosphate stones.[11]
Stones that are primarily calcium oxalate or calcium phosphate typically start as renal calculi, become trapped in the bladder, before developing additional layers of stone material until they are too large to pass and become symptomatic.
There may be an association between bladder calculi and bladder urothelial cancer.[12]
In children, the most common stone types are calcium oxalate, calcium phosphate, and possibly ammonium acid urate. In developing countries, infants and very young children often are only given breast milk and rice, leading to a high urinary ammonia excretion due to the low dietary phosphorus. These children also typically have a high green vegetable intake (high dietary oxalate load) with low dietary citrate.[13]
History and Physical
Bladder stones do not present any particular or specific symptoms, or there may not be any symptoms at all. They are usually associated with various types of incomplete bladder emptying problems, most commonly BPH. There may also be a combination of other urinary symptoms such as terminal hematuria, suprapubic pain, weak stream, dysuria, etc. Terminal gross hematuria with a sudden voiding stoppage is a common sign of a large bladder calculus. Various degrees of pain may be present at the tip of the penis or anywhere in the scrotum, pelvis or perineum. A distended bladder may be palpable in some cases, but the stone typically is not. Since the signs and symptoms of bladder stones are relatively vague, a definitive diagnosis is not typically made without cystoscopy or imaging.
In the past, a definitive diagnosis was sometimes made by the passage of a Van Buren sound. When contact was made with a stone in the bladder, it would produce a "sound" or click along with a transmitted vibration. This is of historical interest only and is not used anymore due to the common availability of modern imaging technology and flexible cystoscopy.
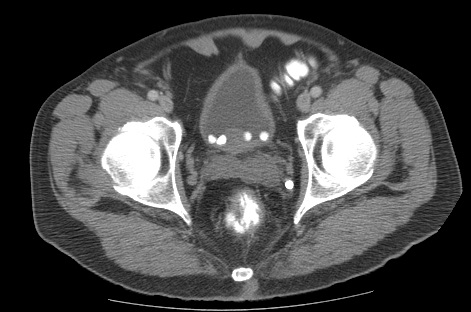
Evaluation
The urinalysis in affected individuals may show blood, nitrites, or leukocytes. It may also demonstrate a low urinary pH and a urinary tract infection (UTI). A plain x-ray or KUB is often the first study ordered, but in adult men, the stone may not be calcified, such as uric acid, so plain x-rays alone may not be sufficient. CT or a bladder ultrasound can be reliably used for imaging for possible bladder stones. Stones will typically show up on ultrasound as hyperechoic areas with shadowing.
Ammonium urate is radiolucent but may develop a calcific coating making it visible on x-rays.
If any bladder filling defect moves when the patient is repositioned, a bladder stone is likely, although it could also be a blood clot, fungal ball, or a papillary urothelial tumor on a long stalk. Since most of these patients will also have associated pelvic pain, hematuria, or voiding difficulties, a cystoscopy is frequently performed, and this will definitively show any bladder calculi.
Treatment / Management
Medical Therapy
Dissolution of bladder stones, particularly uric acid, can sometimes be accomplished with oral alkalinizing agents alone if the higher pH level necessary (usually 6.5 to 7) can be maintained long enough. This is typically done with oral potassium citrate, which can be supplemented with sodium bicarbonate if necessary. For most patients, this will require roughly 60 mEq per day of potassium citrate. Serum potassium levels and urinary pH levels should be checked periodically while on this therapy. The dosage of potassium citrate should be titrated and adjusted to maintain the optimal pH level.[14][15][16]
Patients with a history of nephrolithiasis may benefit from a metabolic evaluation, including a 24-hour urine test for kidney stone production risk factors and directed prophylactic therapy.
Citric acid, glucono delta-lactone, and magnesium carbonate can be used to dissolve struvite (infection) type stones but requires irrigating catheters. Dissolution is relatively slow, so this treatment is infrequently used.[17]
Calcium phosphate is the primary component of the encrustations and debris that typically clogs urinary stents and catheters. It only forms in an alkaline solution and can be dissolved by a mild acid. Periodic bladder instillations of 1/4% acetic acid solution can help dissolve calcium phosphate crystals and prevent bladder stone formation. It can also help maintain patency in Foley catheters, and suprapubic tubes in patients whose urinary drainage tubes tend to become clogged with debris prematurely.
Surgical Therapy
Most stones can be managed with endoscopic surgery. The underlying cause should also be addressed at the same time, if possible.[18]
Cystolitholapaxy can be achieved cystoscopically with most stone types. Various sources of disruptive or ablative therapy can be used, including lasers, pneumatic-powered mechanical contact jackhammer, ultrasound, and direct mechanical crushing with a lithotrite. Electrohydraulic devices are not generally used for bladder stones as the calculi tend to move, and higher rates of mucosal bladder injury are reported. Ultrasound and the lithoclast can usually fragment bladder stones faster than lasers, although all are considered effective.
Extracorporeal shockwave lithotripsy (ESWL) can work for bladder stones, but it requires the treatment head to be above the patient or prone positioning.
Percutaneous suprapubic cystolitholapaxy is the primary means of treatment for pediatric bladder stones, to minimize urethral trauma in children. Larger caliber instruments can be placed suprapubically than transurethrally, particularly in the pediatric age groups. In some cases, a combined procedure with simultaneous suprapubic and cystoscopic approaches are used.
In male adults with outlet obstruction, transurethral resection of the prostate (TURP) is recommended, when indicated, immediately after the stone has been fragmented and removed.
In some cases of extremely large bladder stones or prostates, it may be reasonable to do open suprapubic surgery. This allows for the removal of the intact stone, followed by an open, suprapubic prostatectomy (usually for prostates more than 75 g in size). The main advantage of an open suprapubic cystostomy for bladder stone removal is the reduced overall surgery time (roughly half the time compared to endoscopic means), easy removal of large or multiple stones, ability to remove stones that might be difficult or hard to fragment with endoscopic treatments and the ability to handle stones that are stuck to the bladder lining. The disadvantages of this approach include a longer hospital stay, additional postoperative pain, the need for an abdominal incision and drains, and possible wound complications and prolonged Foley catheterization time.
Differential Diagnosis
The differential diagnosis of bladder stone include the following:
- Fungus ball
- Clot
- Papillary urothelial carcinoma
- Urinary tract infection
- Benign prostatic hyperplasia
Prognosis
The prognosis of bladder stones is generally good if the stones are treated appropriately. Treatment of the stones depends on the cause of the bladder stones. Small bladder stones may pass out easily but the large one can lodge at the bladder neck and stop the flow of urine. Untreated cases can lead to damage to the urinary tract, recurrent stone formation, or infection.
Complications
Bladder stones that are large usually cause complications and these include:
- Pain
- Frequent urination
- Obstruction
- Urinary tract infections
Deterrence and Patient Education
Once a patient has developed bladder stones, the chances of getting recurrent stones are increased. Therefore it is important to identify and treat the underlying cause. Patients must be counseled that drinking plenty of water would protect them from stone formation because increase water intake would dilute all the minerals that precipitate to form stones in the urinary tract. If the prostate is enlarged it should be removed by surgery to prevent stasis of urine in the bladder.
Pearls and Other Issues
A metabolic evaluation (including 24-hour urine testing, basic metabolic panel, and serum uric acid), is indicated in all patients with bladder calculi with uric acid stones, nephrolithiasis, bladder stones without any identifiable outlet obstruction or nidus, recurrent bladder stones, and in individuals with a strong family history of urinary lithiasis.
Enhancing Healthcare Team Outcomes
Bladder stones are relatively uncommon in Western countries but remain an issue for much of the world. Failure to routinely empty the bladder is a major causative factor. Catheters that are not changed for prolonged periods will predispose to bladder calculi. When Foley catheters are removed traumatically, it is important to have the catheter inspected to make sure there are no missing balloon fragments or pieces. All caregivers of the interprofessional team need to be cognizant of the potential risk in such patients of retained balloon fragments inside the bladder, which will otherwise tend to calcify. In such cases, cystoscopy by a urologist assisted by a nurse is necessary to remove any such fragments. More frequent catheter changes and the judicious use of citric acid, glucono-delta-lactone and magnesium carbonate, and 1/4% acetic acid solutions can help reduce the formation of bladder stones, calcium phosphate debris, and catheter encrustations. Pharmacists should assess drug treatments, interactions, and compliance and report concerns to the interprofessional team. Specialty care urologic nurses coordinate care, facilitate communication with the interprofessional team, and work with the team to provide coordinated patient education.
Close communication and coordination of care between urology, primary care, pharmacy, and nursing staff can help reduce the incidence of preventable bladder stones.[19]