Continuing Education Activity
The barium swallow study, also known as a barium esophagogram or esophagram, is a contrast-enhanced radiographic study commonly used to assess structural characteristics of the entire esophagus. It may be used for the diagnosis of a wide range of pathologies including esophageal motility disorders, strictures, and perforations. It may also be used to characterize more distal pathology such as a hiatal hernia or gastric volvulus. This activity reviews the barium swallow study, its indications, and contraindications, and highlights the role of the interprofessional team in evaluating patients with esophageal pathology.
Objectives:
- Identify the anatomical structures evaluated by a barium swallow study.
- Describe the technique for performing a barium swallow study.
- Review the potential risks and benefits of performing a swallow study using barium versus gastrogaffin.
- Explain the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by esophageal pathology undergoing a barium swallow study.
Introduction
The barium swallow study, also known as a barium esophagogram or esophagram, is a contrast-enhanced radiographic study commonly used to assess structural characteristics, and to some extent the functional characteristics of the esophagus. [1] It is important to distinguish this from a "modified barium swallow" study or a "videofluoroscopic swallow study." The videofluoroscopic swallow study examines the mechanics of swallowing and is performed in conjunction with a speech pathologist. [2]
A barium swallow study may be used in the diagnosis of a wide range of pathologies including esophageal motility disorders, strictures, and perforations. [3] [4] It may also be used to characterize more distal pathology such as hiatal hernias, gastroesophageal reflux, or gastric volvulus. A barium swallow study can also be used to obtain some details and evaluation of the swallowing process at the pharyngeal level, although this is often served by a Videofluoroscopic Swallow Study. [5]
The barium esophagogram is noninvasive and readily performed, requiring only radiographic still-image capability and contrast medium. As such, it is a useful exam despite the current wide availability of CT imaging. The use of barium sulfate contrast is considered to result in a more sensitive study when compared to those utilizing water-soluble agents such as Gastrografin/diatrizoate. Barium provides better contrast images.
Anatomy and Physiology
As with all imaging, interpretation of a barium esophagram requires a knowledge of anatomy and function.
The esophagus is a roughly 20 to 25 cm portion of the gastrointestinal (GI) tract that lies between the oral cavity and stomach. Its role is to transport both solid and liquid oral intake distally to the rest of the GI tract in a coordinated fashion. [6]
The origin of the esophagus is at the level of the cricoid cartilage. This is where the inferior pharyngeal constrictor muscle abuts the cricopharyngeus muscle. This area is known as the upper esophageal sphincter (UES). At the distal end, the esophagus terminates at the lower esophageal sphincter (LES), which is an area of muscular thickening that occurs where the esophagus passes through its diaphragmatic hiatus. When normal anatomy of the LES is disrupted, such as with a hiatal hernia, the sphincter is mechanically defective and can lead to common pathologies such as gastroesophageal reflux.
The UES serves to prevent air from entering the GI tract and prevent reflux of distal GI tract contents into the pharynx. It is located around 15 cm from the incisors. It is composed mainly of the inferior pharyngeal constrictor musculature, specifically the cricopharyngeal portion (also sometimes referenced as the cricopharyngeus muscle). This is notable as it is the most common site of iatrogenic perforation during endoscopy.
The LES, similar to the UES, plays a critical role in preventing reflux of gastric contents. It is closed at rest but does undergo periodic relaxations from unclear causes and for unclear reasons. As stated earlier, the incompetence of the LES is related to common pathologies such as gastroesophageal reflux disease (GERD) and Barrett metaplasia. [7] The LES is located around 40 cm from the incisors.
In between the esophageal sphincters is the esophageal body. This serves to propel food to the stomach via peristalsis. Although it is functionally a smooth tube, three anatomic landmarks are clinically important and commonly described in the literature as they cause esophageal narrowing. The first is at the UES at the level of the cricoid cartilage. In the mid-portion, the aortic arch and left mainstem bronchus provide some extrinsic compression. The final narrowing is at the LES, which should denote the esophageal hiatus of the diaphragm.
The histologic structure of the esophagus follows the same general schema seen in other muscular GI tract organs. Its wall is composed of several layers including a squamous epithelial mucosa, a muscular layer, and adventitia as its outermost layer. Note that most intraperitoneal portions of the GI tract have serosa as their outermost layer.
Vascular supply of the esophagus is from the inferior thyroid artery in the cervical portion, by the left gastric and inferior phrenic arteries in the abdomen, and via branches from the bronchial arteries and off the aorta otherwise. Venous drainage is via branches to the azygos and hemiazygos veins except distally, where branches drain to the coronary vein. The coronary vein drains into the portal circulation, which is important as these can become varices in the setting of cirrhosis.
Innervation is via the vagus nerve and adjacent sympathetic trunk.
Indications
Barium swallow studies are used to define the structure and, to a much lesser extent, the function of the esophagus. Pathologies typically seen with barium swallow include esophageal perforations, neoplasms, hiatal hernias, and diverticula. Some motility disorders are also readily diagnosed with barium swallow due to the secondary effects they have on esophageal morphology, though most functional esophageal swallowing pathologies will require a formal modified barium swallow evaluation. This includes achalasia, which is characterized famously by a "bird beak" appearance and a dilated, tortuous, proximal esophagus. [8] Diffuse esophageal spasm is identifiable by a "corkscrew" sign. [9][10]
Effects or changes in chemical esophageal injury can be studied with barium sallow. In the long term after injury, contrast may be used to identify strictures or sometimes more subtle findings such as ulceration in conjunction with endoscopy. It is important not to obtain barium contrast studies in the acute setting of chemical esophageal injury as it can exacerbate the injury. [11]
A further consideration regarding the choice of swallowed contrast agent in the setting of trauma. For the purposes of this section, trauma will be defined as injury resultant from non-iatrogenic causes such as gunshot wound. Guidelines for nontraumatic esophageal perforation investigations often involve the use of Gastrografin/diatrizoate (water-soluble) contrast swallow studies initially, followed by a thinned barium swallow study if the study is negative in the face of significant clinical suspicion. This is because barium extravasation into the mediastinum carries a risk of resultant inflammation and is more difficult to wash out than Gastrografin/diatrizoate during surgical exploration. However, a barium contrast study has better sensitivity than that of Gastrografin/diatrizoate in the detection of perforation. In such clinical situations, timeliness of diagnosis is important, and surgical exploration may be likely on a positive swallow study or even already warranted due to other criteria. This would allow for a washout of extravasated contrast, thus minimizing the risks associated with barium while maximizing sensitivity during an urgent workup. Additionally, aspiration of Gastrografin/diatrizoate is known to cause severe pneumonitis. [12] This is of concern in the setting of concomitant tracheal injury that would allow for Gastrografin/diatrizoate to extravasate into the airway. Barium sulfate is not innocuous when aspirated but causes a less severe pneumonitis.
Contraindications
Barium swallow studies should be used in cases of suspected esophageal perforation only after considering the risk of inflammatory mediastinitis. This is not an absolute contraindication and should be weighed against the benefit of obtaining a timely diagnosis. Patients must be capable of swallowing relatively large amounts of contrast without assistance and be able to protect their airway.
Do not administer barium in cases of suspected acute, chemical esophageal injury as there is little useful information to be gained from a contrast swallow study in such cases.
Preparation
For studies focused on the pharynx and esophagus, minimal preparation is required. However, patients should be able to tolerate swallowing liquids.
Technique or Treatment
The barium swallow exam technique can differ between institutions. Generally, the two components of barium swallow examination involve the evaluation of the hypopharynx/cervical esophagus and the thoracic esophagus using fluoroscopy. The steps are summarized as follows:
- Upright position - Administration of crystals (effervescent sodium bicarbonate granules) and consumption of water for distension.
- Upright position - Place the patient in the left posterior oblique position, have the patient drink a mouthful of thick barium while taking spot images from the cervical esophagus to the gastroesophageal junction. These constitute "double-contrast" images.
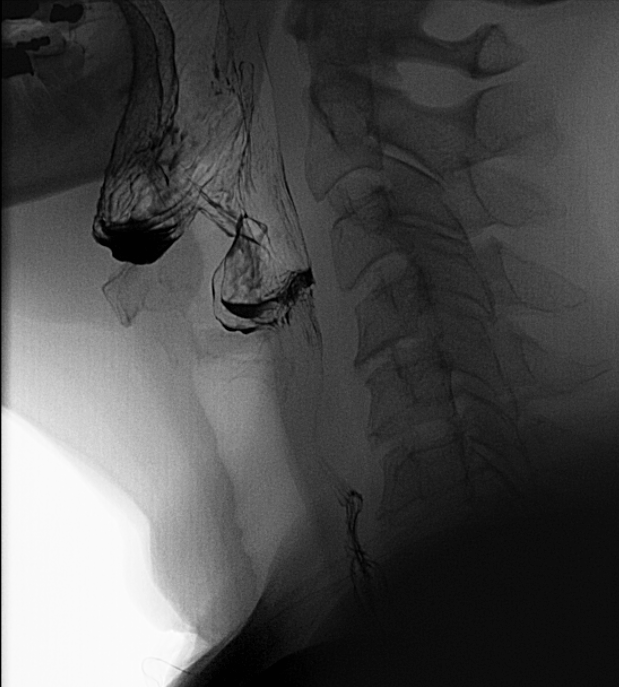
- Upright position - Place the patient in the lateral position, cone down to the hypopharynx and video record(~4 frames/second) while the patient swallows a mouthful of thin barium. Acquire a spot distension images while the patient phonates the sounds "aaaaa" and "eeee."
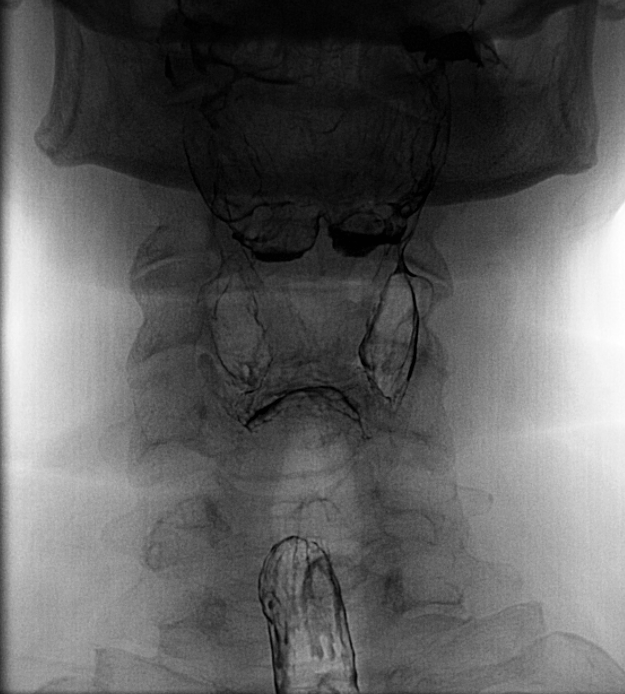
- Upright position - Place the patient in anteroposterior position, cone down to the hypopharynx, and video record(~4 frames/second) while patient swallows a mouthful of thin barium. Acquire a spot distension images while the patient phonates the sounds "aaaaa" and "eeee." A "trumpet Valsalva" spot image can also be obtained and aims to distend the throat with air.
- Horizontal position - While in the horizontal position, place the patient in the right anterior oblique position(ie patient should be prone). Have the patient drink thin barium with a straw and watch the contrast descend down the esophagus. Acquire a spot image of the gastroesophageal junction with and without Valsalva. Closely evaluate for a hiatal hernia, reflux, and for signs of dysmotility. Additional images to evaluate for reflux can be performed in the right posterior oblique position(supine) with provocative maneuvers such as coughing, although this might not be appropriate given the low yield of these maneuvers.
- Upright position - Have the patient swallow a barium tablet with a small amount of water. Observe for uneventful passage to the stomach. Additional sips of water can be consumed if the pill is not transiting to the stomach.
Points to Consider
- While in the right anterior oblique position, the left arm and knee will be flexed and the head rotated left, allowing for some elevation of the left side.
- The barium volume during each swallow is roughly 100 to 200 cc.
- The goal, typically, is to distend the esophagus for the best resolution.
- The contrast media may be further thinned with water if needed to reveal more subtle lesions.
- The exact thickness of contrast and amount will depend on the local radiology protocol and also the reason for the exam.
- Equipment with a still-image X-ray, while limited, can be sufficient.
Complications
Oral barium contrast has relatively few adverse effects in standard practice. Most commonly, patients complain of nausea and vomiting within 30 minutes of ingestion. Hypersensitivity reactions have been reported but are uncommon. Most adverse effects are related to extravasation of contrast into the mediastinum or from aspiration.[13]
Clinical Significance
As stated earlier, the barium esophagram is a quickly performed, readily available study that is useful in the diagnosis and surveillance of a vast range esophageal diseases. In many cases, it is the first and only imaging study that needs to be performed. Additionally, the study may be used to plan surgical intervention by localizing lesions seen in other modalities, such as on endoscopy. The following list of esophageal pathologies (categorized roughly by type) that may benefit from esophagram in workup is not fully inclusive, but it serves to highlight the diversity of clinical situations where it may play some role.
Structural
- Esophageal diverticula (Zenker's, mid-esophageal, and epiphrenic)
- Strictures
- Ulcerations
- Hiatal hernia
Neoplastic, Benign
- Fibrovascular polyps
- Lipomas
- Leiomyomas
Neoplastic, Malignant
- Adenocarcinoma
- Small cell carcinoma
- Gastrointestinal stromal tumor (potentially)
- Leiomyosarcoma
Mobility
- Achalasia
- Hypertensive lower esophageal sphincter
- Diffuse esophageal spasm
- Ineffective esophageal motility/hypotensive peristalsis
Traumatic
- Iatrogenic injury - endoscopy, laryngoscopy
- Perforation - blunt/penetrating trauma
- Perforation - effort (Boerhaave's Syndrome)
- Post-caustic injury stricture
Pediatric
- Esophageal atresia/stricture
- Tracheoesophageal fistula
It is important to note that, regardless of the appearance of a lesion discovered on esophagram, all masses, strictures, and complaints of dysphagia require consideration of endoscopy for a complete workup.
Enhancing Healthcare Team Outcomes
The barium swallow test is usually performed by a radiologist. However, the ordering of the test may be done by a nurse practitioner, primary physician gastroenterologist, surgeon, neurologist or speech therapist. The test is primarily used to assess structural characteristics of the entirety of the esophagus. It may be used in the diagnosis of a wide range of pathologies including esophageal motility disorders, strictures, and perforations. It may also be used to characterize more distal issues such as a hiatal hernia or gastric volvulus. It may also be used in some capacity to evaluate swallowing at the pharyngeal level, but that is a function that is often served by a Videofluoroscopic Swallow Study (modified barium swallow study).
The barium esophagogram is noninvasive and readily performed, requiring only radiographic still-image capability and contrast medium. As such, it is still a useful exam despite the current wide availability of CT imaging. The use of barium, specifically, barium sulfate, is considered to result in a more sensitive study when compared to those utilizing water-soluble agents such as Gastrografin/diatrizoate.