Continuing Education Activity
Mechanical ventilation is a common intervention used to treat patients with acute respiratory failure. Assist-control ventilation is the most common setting used in the ICU and is the only setting with proven mortality benefits in patients with ARDS. This activity outlines the management of patients being ventilated on assist control and describes the importance of the interprofessional team in dealing with issues pertaining to the ventilator.
Objectives:
- Explain the definition of assist control ventilation.
- Summarize how to manage ventilator settings in assist control mode ventilation.
- Review when assist control indications and the potential advantages of selecting this ventilatory mode.
- Identify the interprofessional management of the ventilator and the roles of the different members of the interprofessional team in dealing with ventilated patients.
Introduction
Mechanical ventilation is a lifesaving procedure that is often performed when patients require respiratory support.[1] Assist-control (AC) mode is one of the most common methods of mechanical ventilation in the intensive care unit[2].
AC ventilation is a volume-cycled mode of ventilation. It works by setting a fixed tidal volume (VT) that the ventilator will deliver at set intervals of time or when the patient initiates a breath. The VT delivered by the ventilator in AC always will be the same regardless of compliance, peak, or plateau pressures in the lungs.
When AC mode is selected in the ventilator, four parameters may be quickly modified:
This is the set amount of volume that will be delivered with each breath. Changing the VT will, in turn, change the minute ventilation (VT x RR); an increase in minute ventilation will result in a decrease in carbon dioxide (CO2), by the same token, a decreased VT will result in a decreased minute ventilation and increase in the patient’s blood CO2.
This is the set rate for delivering breaths per minute (bpm). For example, if the set rate is 15, then the delivery is 15 bpm or 1 breath every 4 seconds. This is called time-triggered control. In AC, this set rate can be overturned by the patient, meaning that if the patient inhales, the ventilator will sense the drop in pressure and deliver that breath, even if the patient is breathing above the set rate. For example, if a patient is breathing at 20 bpm and the ventilator is set at 15 bpm, the ventilator will follow the patient and deliver 20 bpm (one each time the patient initiates a breath). This is called patient-triggered breaths. The ventilator will only deliver breaths at the set RR if the patient does not trigger it faster. As with VT, increasing RR will increase minute ventilation and decrease the patient’s blood CO2. A caveat on this is that by increasing the RR, the dead space is also increased, so increasing RR may not be as effective as increasing VT in improving ventilation.
The ventilator in AC mode is programmed to sense changes in the system pressure when a patient initiates a breath. When the diaphragm contracts, the intrathoracic pressure becomes more negative. The negative pressure is transmitted to the airways and then to the ventilator tubing, where sensors detect the change in pressure and deliver a breath to the set tidal volume. The amount of negative pressure needed to trigger a breath is called the trigger sensitivity and is usually set up by the respiratory therapist.
This is the percentage of oxygen in the air mix delivered by the ventilator during each respiratory cycle. Increasing the FiO2 will increase the patient's oxygen saturation.
The positive pressure that will remain in the system at the end of the respiratory cycle (end of expiration) is the PEEP. As with FiO2, PEEP can be used to increase oxygenation. By Henry’s law, we know that the solubility of a gas in a liquid is directly proportional to the pressure of that gas above the surface of the solution. This applies to mechanical ventilation in that increasing PEEP will increase the pressure in the system. This increases the solubility of oxygen and its ability to cross the alveolocapillary membrane and increase the oxygen content in the blood. PEEP also can be used to improve ventilation-perfusion mismatches by opening or “splinting” airways to improve ventilation throughout the system.
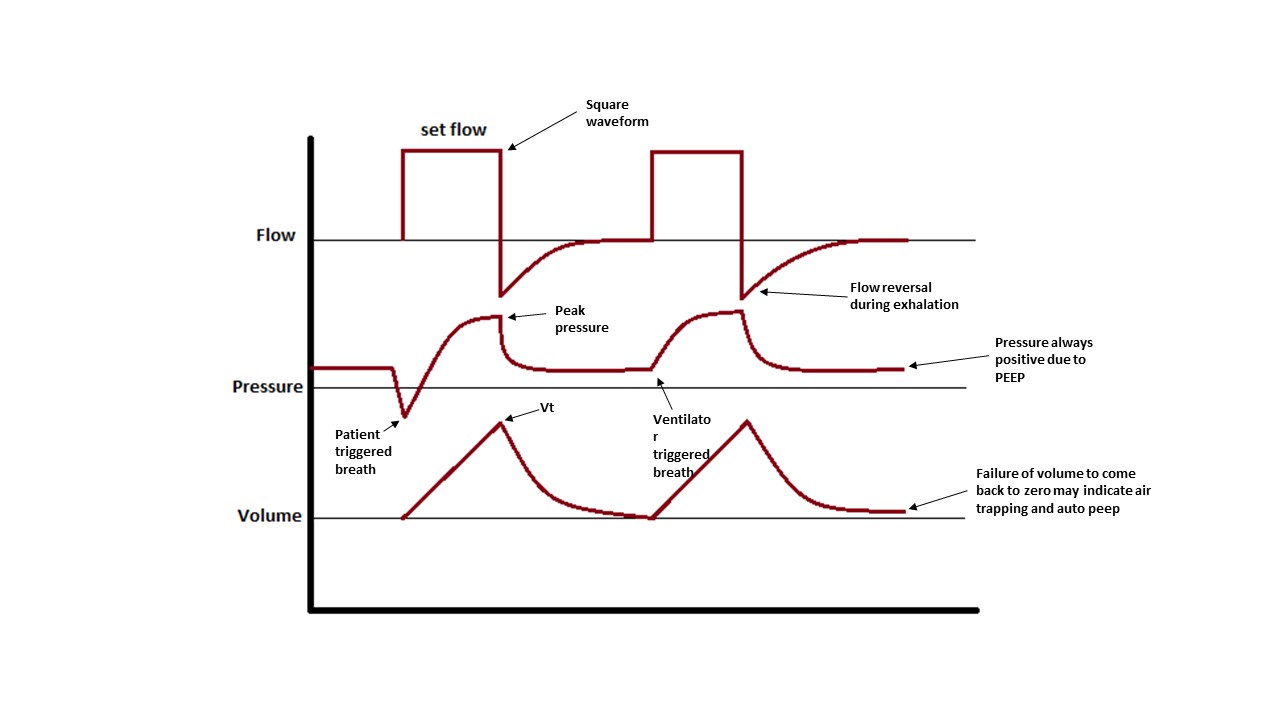
Apart from these four main parameters, the way the ventilation is delivered also can be adjusted. For every setting, regardless of the rate and volume, the breath will always be delivered to the patient in the same way. The ventilator allows flow change; the flow may be constant through the inhalation (square waveform) or decelerating as the breath is delivered (ramp waveform).
- Square waveform will allow for faster delivery of the inspiration, decreasing the inspiratory time and increasing the expiratory time. This can be useful for patients with asthma or chronic obstructive pulmonary disease or in cases of increased RR to prevent auto-PEEP and allow for enough time for exhaling.
- Ramp waveform will decrease the flow as the delivered volume increases. This is usually more comfortable for the patient and allows for a better volume distribution and equalization in patients with heterogeneous lungs, such as ARDS.
The speed at which this flow is delivered also can be controlled by setting inspiratory and expiratory times.[3] This can be adjusted for patient comfort or to prevent auto-PEEP.
After the inspiration is finished, the expiratory valve of the ventilator opens, and the air is allowed to come out until the pressure in the system reaches PEEP. (figure 1)
Function
AC mode is an excellent method to assure good ventilation. It is frequently used in cases of metabolic or respiratory acidosis.
AC was the mode used in the landmark study “Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome,” from where the ARDSNET protocol came to be[4]. For this reason, it is the only proven mode with survival benefit in patients with acute respiratory distress syndrome (ARDS) and should be the mode of choice to use as it allows for the operator to administer low tidal volumes and adjust PEEP as necessary.
Issues of Concern
An important concept to understand in AC mode is that because the system is volume-cycled and a set volume will always be delivered, the pressure that will be generated in the system will be determined by lung compliance. A very compliant lung will generate low plateau pressures, while a stiff lung does not distend well with the set volume and will generate a much higher pressure (i.e., patients with pulmonary edema, ARDS, pneumonia, or pulmonary fibrosis). It is important to understand this to prevent ventilator-induced lung injury or barotrauma.[5][1] Peak pressure in the system is usually determined by airway resistance and not by compliance, while plateau pressure or the pressure in the system at the end of inspiration is determined by compliance and volume delivered.
Other Issues
New ventilator modes are designed to improve some of the shortfalls of AC:[6][1]
- NAVA (neurally adjusted ventilator assist): In this mode, sensors in the diaphragm measure the timing and intensity of the patient’s respiratory effort and couple it with the timing and intensity of the ventilator assist, thereby preventing barotrauma and ensuring ventilator demand fulfillment.[7][8][5]
- ASV (Adaptive support ventilation): This mode automatically adapts inspiratory pressure and respiratory rate with minimum work on the part of the patient to assure a target minute ventilation is reached[9].
- APRV (Airwar pressure release ventilation): This pressure-cycled mode of ventilation delivers a continuous set pressure for a set amount of time and then "releases," giving time for the lung to deflate for a shorter period. In theory, this maintains alveoli inflation to prevent alveolar damage. This mode sometimes is used in patients where AC cannot be effectively and safely continued due to persistently elevated plateau pressures and continuously poor oxygenation[10].
These and other methods currently are being studied as alternative modes of mechanical ventilation, but none have shown clear superiority over the others.
Enhancing Healthcare Team Outcomes
There are several ways to ventilate a patient, and the pulmonologist or the intensivist makes that decision. No other healthcare professional should make changes to the ventilator settings without first getting approval from the physician in charge. In most hospitals, the respiratory therapist will be in charge of the ventilator and will be the one to make changes in the ventilator settings when required physically. The nurse monitoring the patient should be familiar with the ventilator settings, the alarms, and what they mean. When a ventilator setting is made, it has to be noted in the chart. Coordination by the interprofessional team will improve outcomes. [Level 5]