Introduction
Aspergillus is a ubiquitous saprophyte in nature found in air, soil and organic matter. Humans normally inhale the spore form of the fungi. However, the disease is usually seen in immunocompromised patients. The immune system plays an important role not only in recognizing inhaled mold and controlling growth but also in regulating the body's allergic and inflammatory response to the infection.[1][2][3]
High mortality rates often accompany systemic Aspergillus fumigatus infections; therefore, early diagnosis and treatment in the immunocompromised population are important.
Etiology
The most common species responsible for infections are A. fumigatus, Aspergillus flavus, and Aspergillus terreus.
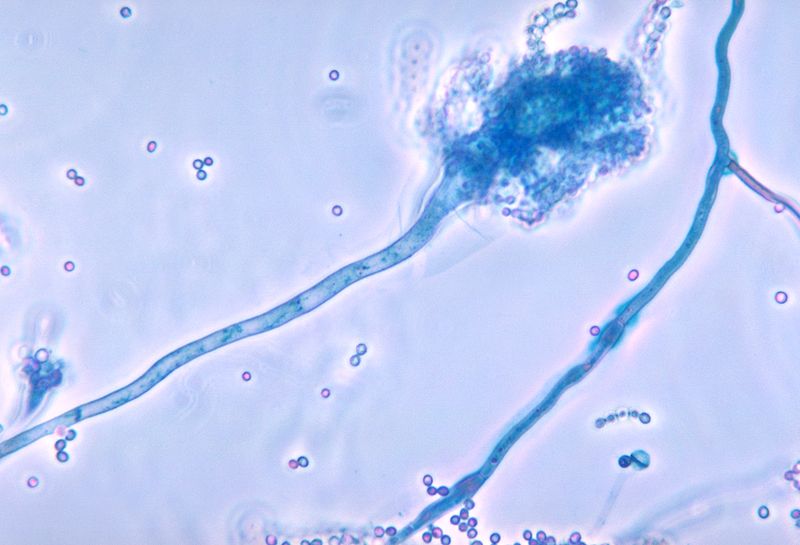
A. fumigatus is a fungus from the family of Trichocomaceae. First described by Fresenius in 1863, it is known to have a stable haploid genome of 29.4 million base pairs.
The life cycle outside of the human host is characterized by asexual reproduction which proceeds conidiophores, structures where the infectious form known as conidia, are produced and released into the air. Conidia are responsible for fungal dispersion and preserving the fungi genome under adverse conditions.
Epidemiology
On average, there are as many as a few hundred conidia inhaled by humans daily.[4][5][6]
Species prevalence has changed over the past decade. A. fumigatus used to be the culprit of 90% of infections. In recent studies, it has been shown that A. fumigatus species complex is responsible for approximately 60% of infections followed in frequency by A. flavus, Aspergillus niger, and A. terreus respectively.
Invasive pulmonary aspergillosis is usually seen in patients with underlying conditions and risk factors such as severe prolonged neutropenia, inherited immunodeficiency, steroid dependency, use of immunosuppressive medications, transplant patients, AIDS.
Other forms of aspergillosis such as allergic bronchopulmonary aspergillosis (ABPA), allergic sinusitis, and saprophytic infection are important causes of morbidity but are seldom life-threatening.
Pathophysiology
Infections caused by Aspergillus are commonly located in the lower respiratory tract, lungs, sinuses, and skin. The central nervous system (CNS) and cardiovascular system may be affected by direct or hematogenous spread.
Human-host defense against the inhaled spores begins with the mucous layer and the ciliary action (compromised in diseases such as cystic fibrosis, asthma, Kartagener) located in the respiratory tract. Macrophages normally react upon recognizing fungi key cell wall components such as beta-D-glucan, secreting inflammatory mediators that ultimately attract neutrophils to initiate cellular immunity.
Many species of Aspergillus are known to produce toxic metabolites (aflatoxins, mycotoxins 3-nitropropionic acid, and ochratoxin A) which inhibit the action of macrophage and neutrophil phagocytosis.
Underlying immunosuppression is directly proportional to neutrophil dysfunction and reduced number of neutrophils. Patients on chronic steroid treatment also have associated macrophage and neutrophil function. In these cases, the risk of disease along with the type of disease is secondary to impaired phagocytosis, suppressed T cell function and oxidative cascade.
Vascular invasion can also occur if fungal cell surface components bind to the vessel wall components ultimately resulting in necrosis, infarction, or hemorrhage.
Chronic necrotizing pulmonary aspergillosis is characterized by granuloma formation and alveolar consolidation.
Histopathology
Aspergillosis is defined as infection with histopathological confirmation and a positive result of the specimen from a normally sterile site.
Biopsies carry the risk of bleeding, the reason for which noninvasive testing is usually done as the initial step. These include serum biomarkers and sputum analysis.
If a biopsy is warranted, it is usually guided by imaging such as bronchoscopy, video-assisted thoracoscopy surgery, or CT.
History and Physical
Clinical presentation of Aspergillus-related infections manifests on a large spectrum. There are two important variables: underlying immune status and underlying pulmonary disease.
This spectrum can range from acute bronchopulmonary aspergillosis, chronic pulmonary aspergillosis, bronchitis, acute community-acquired, chronic cavitary nodules/aspergilloma to invasive disease in those severely immunocompromised.
Allergic bronchopulmonary aspergillosis, most commonly found in patients with underlying asthma/cystic fibrosis, presents as asthma (shortness of breath with associated wheezing) with recurrent exacerbations which could in some cases be complicated by systemic symptoms such as fever, malaise, bronchial obstruction, or brown mucous plugs. This can be associated with allergic fungal rhinosinusitis characterized by common symptoms of sinusitis but associated with dark-colored nasal discharge.
Chronic pulmonary aspergillosis presents as a progressive course over months of fatigue, malaise, fever, night sweats, shortness of breath, weight loss, cough, hemoptysis, and sputum production. Its presentation also ranges from a spectrum of aspergilloma, aspergillus nodule, chronic cavitary aspergillosis, chronic fibrosing aspergillosis, and subacute invasive pulmonary aspergillosis formerly known as chronic necrotizing aspergillosis.
Of note, subacute invasive aspergillosis is present in patients with evidence of immunosuppression, however, whereas invasive presentations have a short progression of 4 weeks, subacute presentation progresses over the course of 1 to 3 months.
Invasive aspergillosis is commonly seen in states of severe immunosuppression such as organ transplanted patients, AIDS, prolonged neutropenia, advanced cancer, prolonged use of steroids. It most frequently presents as a pulmonary infection after airway inoculation of conidia, however gastrointestinal and skin forms are also seen. Suspicion for pulmonary aspergillosis in the setting of the comorbidities mentioned above should arise if any of the following present: fever, shortness of breath, hemoptysis, cough, pleuritic chest pain. Tracheobronchitis is commonly seen in organ transplant patients. Rhinocerebral aspergillosis is seen in the setting of hematological malignancies in neutropenic patients. Disseminated infection correlates with poor prognosis, and it can be seen affecting organs such as the brain, (brain abscesses and infarction), eye (endophthalmitis), skin (cutaneous aspergillosis), liver, heart (endocarditis), and kidneys.
Evaluation
Evaluation of suspected aspergillosis infection varies depending on the patient's presentation and immune state.[7][8]
Initial management should include laboratory studies such as:
- Complete blood count with differential to determine eosinophil count (which is usually elevated more than 500 cells/microliters), serum IgE (elevated more than 1000 IU/mL).
- Aspergillus skin test positivity or detectable IgE against Aspergillus
- Sputum analysis Gram stain plus culture: with findings of eosinophils, Charcot-Leyden crystals, and Aspergillus in culture.
- Imaging: Aspergillus bronchopulmonary infection can be evidenced on chest x-ray with findings of mucous plugs or central bronchiectasis. Upper lobe parenchymal opacities with atelectasis secondary to bronchial obstruction are also commonly seen. Imaging can be further assessed with high-resolution CT scan which can also detect mucous plugging, tree-in-bud opacities, ground-glass attenuation, and atelectasis. In cases of early invasive aspergillosis, CT scan can provide an early diagnosis when detecting focal lesions in the presence of fever: nodules with ground glass infiltrates are seen in neutropenic patients (halo sign). CT head is warranted in cases of suspected CNS aspergillosis with evidence of ring-enhancing lesions (abscesses) and cortical or subcortical infarction.
Aspergillomas are radiologically characterized by a rounded mass (fungal ball) in a pulmonary cavity associated with a positive culture or positive IgG. Nodules can also be a form of radiological presentation after lung cancer is excluded with biopsy. Chronic cavitary/fibrosing forms present as 1 large or more than 2 cavities without a fungal ball associated with the previously mentioned chronic symptoms and positive cultures/IgG.
- In cases of severe invasive aspergillosis an emerging tool has been used especially in intensive care unit patients, beta-(1,3)-d-glucan which is a cell wall component of Aspergillus and useful in cases where the onset of treatment is essential to improve prognosis. This component is also present in other organisms such as Candida, Fusarium, and Pneumocystis.
- Serum galactomannan is another Aspergillus cell wall component released into the bloodstream during intravascular hyphal growth. However, as it is captured by a neutrophil concentration that may be falsely low which makes its sensitivity lower in non-neutropenic patients.
- The key test for chronic pulmonary aspergillosis is a positive Aspergillus immunoglobin (IgG) serum test. Only a minority of patients have positive cultures (less than 10%). Elevated galactomannan assay from bronchoalveolar lavage fluid yields higher sensitivity in these cases. Other nonspecific markers are elevated CRP and ESR.
Treatment / Management
Treatment of acute bronchopulmonary aspergillosis consists of a glucocorticoid regimen plus itraconazole. Voriconazole is another alternative in cases where itraconazole is not well tolerated. Systemic glucocorticoids are the mainstay of treatment followed by a slow oral taper over the course of 3 months. The initial dose of prednisone is usually 0.5 mg/kg.[9][10][11]
Monitoring consists of measuring serum total IgE every 1 to 2 months.
In poorly controlled patients, asthma studies have shown that omalizumab a humanized monoclonal antibody against IgE have suggested benefits in patients without cystic fibrosis.
Chronic pulmonary aspergillosis treatment varies with the manifestations of the disease in the wide range previously described and patient's pulmonary status:
- Aspergilloma: surgical resection with or without embolization can be considered in patients with limited disease and good respiratory function to prevent hemoptysis, along with pre and postoperative antifungal therapy such as Voriconazole to avoid pleural aspergillosis. However, patients with stable radiographic findings, asymptomatic, immunocompetent a conservative management guided by close monitoring is also a feasible option.
- Aspergillus nodules that have been resected to rule out lung cancer should not be treated with antifungal therapy unless the patient is symptomatic. Monitoring with imaging and serum antibody titers is recommended.
- Chronic cavitary/fibrosing pulmonary aspergillosis: require antifungal treatment. Studies have been done with Itraconazole, Voriconazole, Posaconazole, Isavuconazole, Amphotericin B and Micafungin, leaving the latter 2 for severely ill patients who have failed azole therapy. Embolization is reserved for patients who develop hemoptysis. Treatment duration recommended is 6 months, however, if the disease progresses lifelong therapy may be warranted.
- Invasive aspergillosis treatment can either be monotherapy with voriconazole or in combination with an echinocandin. However, it is important to take into account the species of Aspergillus when choosing the right antifungal therapy. If there is no good response to the initial therapy or progression/deterioration of patient's status is noted then salvage therapy with other drug regimens such as isavuconazole, amphotericin B plus echinocandins should be considered. The length of treatment depends on the location of the infection with a minimum duration of 6 to 12 weeks that could be prolonged for months or years. Debridement of necrotic tissue might be required as adjunctive therapy in severe cases.
Differential Diagnosis
The following should be considered as the differential diagnosis in the wide presentation of Aspergillus-related infections:
- Bacterial/viral pneumonia
- Asthma exacerbation
- Lung abscess/bronchogenic carcinoma
- Pulmonary tuberculosis
- Pulmonary embolism
- Sarcoidosis
- Nocardiosis
- Mucormycosis
- Bronchiectasis
- Cystic fibrosis exacerbation
Prognosis
Prognosis depends on the initial presentation of the infection, with allergic bronchogenic aspergillosis being the milder end of the spectrum and invasive aspergillosis being the severe end of the spectrum. Treatment course and response largely depends on the site of infection as well as the patient's immune state. Longer treatment periods might be required for immunocompromised patients who have a slower response to treatment.
Pearls and Other Issues
Prevention of advanced disease starts with reducing mold-exposure and antifungal prophylaxis targeted to high-risk patients with options such as mold-active azoles, echinocandins, and amphotericin B formulations.
Studies have shown that in patients with myelodysplastic syndrome, acute myelogenous leukemia, and severe graft-versus-host disease, posaconazole was an effective prophylactic agent. It is important to state that mold-active azoles have significantly drug-drug interaction rate given their metabolism through CP-450 and that this is taken into consideration when choosing the appropriate drug therapy.
Further investigation is needed to determine the best treatment in cases of prophylaxis failure in patients with invasive aspergillosis, diagnostic tests with higher sensitivity and specificity and detection of polymorphisms in host genes that mediate innate immunity and may play a role in invasive infection in periods of immunosuppression.
Enhancing Healthcare Team Outcomes
Aspergillus infections are best managed by an interprofessional team because of their seriousness. In immunocompromised people, the infection can rapidly turn fatal. In patients with prior lung disease or those who are immunocompromised, it is recommended that one consult with an infectious disease expert for management. The outcomes after an aspergillus infection depend on the patient's comorbidity and immune status. In healthy people, the outcomes are good but in immunocompromised patients, the outcomes are guarded.