Continuing Education Activity
Argyll Robertson pupils describe the physical exam findings associated with advanced stages of syphilis. Characterized by bilateral small pupils that fail to constrict in response to bright light but exhibit constriction during near vision tasks, Argyll Robertson pupils are a diagnostic marker for tertiary syphilis. This activity provides participating clinicians with an in-depth explanation of the neurological and ophthalmological aspects of Argyll Robertson pupils, facilitating a comprehensive understanding of the pathophysiology and clinical significance. Participating clinicians will enhance their proficiency in evaluating these findings, equipping them with the knowledge to recognize and differentiate this clinical sign within the context of late-stage syphilis. The course emphasizes the collaborative role of the interprofessional healthcare team in managing patients with tertiary syphilis, emphasizing a holistic approach to patient care. Through case studies and interactive discussions, participants will gain insights into the appropriate diagnostic and therapeutic interventions, contributing to improved patient outcomes.
Objectives:
Identify the pathophysiology of Argyll Robertson pupils.
Determine the physical exam of a patient with Argyll Robertson pupils.
Apply the treatment and management options available for Argyll Robertson pupils.
Implement interprofessional team strategies for improving care coordination and outcomes in patients with Argyll Robertson pupils.
Introduction
Argyll Robertson pupils describe the physical exam finding of small bilateral pupils that do not constrict when exposed to bright light but do constrict when focused on a nearby object.[1] This finding is highly specific to late-stage syphilis. Scottish ophthalmologist and surgeon Dr. Douglas Argyll Robertson first described Argyll Robertson pupils in the mid-1860s.[1] However, the root cause remains unknown till today, and the light reflexes are visibly affected.
The condition usually occurs with other features of tertiary syphilis, which is how it is diagnosed and treated. As the underlying etiology is an STI, syphilis is spread from contact with the bodily fluids of a person with syphilis, typically during sexual contact with a sore (chancre) or from a mother to a fetus. Less common routes of transmission exist as well.
Since the prevalence of syphilis is still rising, clinicians from emergency, primary, and internal specialties may encounter the presentation. In the tertiary stage of syphilis, the risk of morbidity is high, and this pupillary finding should be taken seriously. The underlying cause, if correctly identified, is easily treatable with antibiotics. Some complications relating to cardiac or nerve damage may be irreversible.
Etiology
Argyll Robertson pupils are found in late-stage syphilis, a disease caused by the spirochete Treponema pallidum.[2] Neurosyphilis occurs due to an invasion of the cerebrospinal fluid (CSF) by the spirochete, which likely occurs soon after the initial acquisition of the disease. However, the exact pathophysiology leading to the Argyll Robertson pupils remains unknown.[2]
Epidemiology
The exam finding of Argyll Robertson pupils has been rare in the developed world since the advent of penicillin. Still, in the modern era, the number of cases of primary and secondary syphilis has been increasing every year since 2001 and continues to rise. According to the CDC, 30,676 cases of late and late instances of latent neurosyphilis were reported in the United States in 2016.[1] The CDC acknowledges, however, that the disease is likely under-reported. From 2000 to 2016, the rise in reported syphilis cases is primarily due to increased cases in men who have sex with men (MSM) population. This may be because syphilis is more common in MSM, many of whom concurrently also have HIV, or it could reflect 2 separate groups with increased susceptibility. A high co-infection rate with HIV exists in those MSM patients who have contracted syphilis. The US CDC data estimates that 5% of MSM with syphilis are also infected with HIV. Additionally, reports have indicated that syphilis has been rising with the global HIV/AIDs epidemic. [3]
Pathophysiology
The exact pathophysiology of Argyll Robertson pupils remains unknown. Thompson and Kardon (2006) propose the current leading theory that syphilis leads to a "dorsal midbrain lesion that interrupts the pupillary light reflex pathway but spares the more ventral pupillary near the reflex pathway."[1][4][5]
Their research implicates a portion of the rostral midbrain (brainstem) near the Sylvian aqueduct as the most likely location of the syphilitic lesion. Damage to this specific area would impact the efferent pupillary fibers located on the dorsal aspect of the Edinger-Westphal nucleus (EWN). These fibers are a crucial component of the light reflex. Fibers associated with the accommodation reflex, situated more ventrally to the EWN, are unaffected.[4][5]
History and Physical
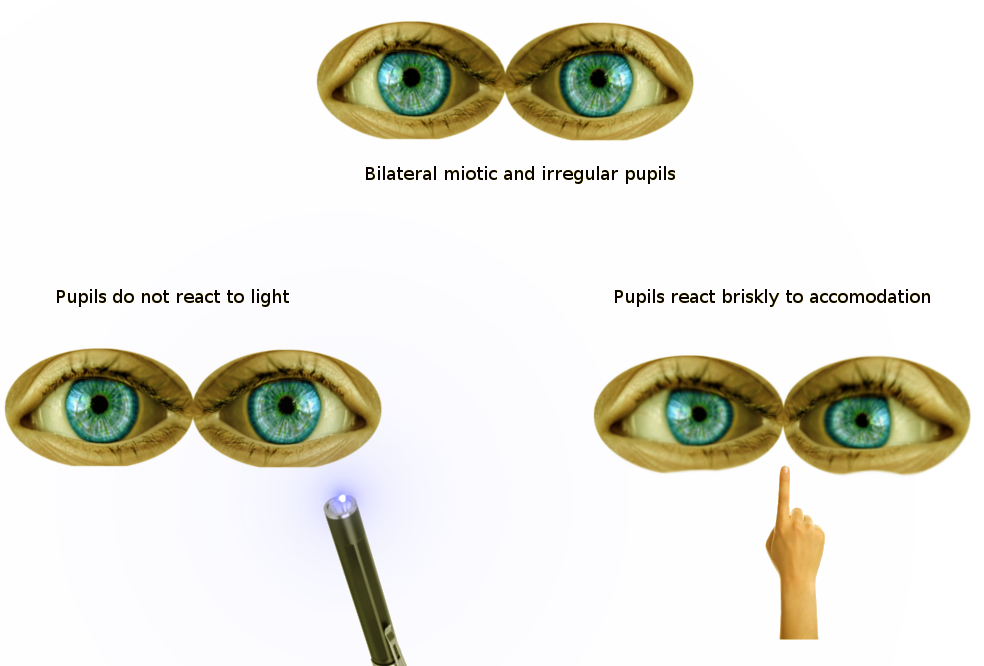
The patient with Argyll Robertson pupils will show small, irregular pupils with light-near dissociation: absent light reflex, prompt constriction with near accommodation (see Image. Findings of Argyll Robertson Pupils on Pupillary Reflex Exam). Symptoms are usually bilateral and have a gradual onset of months to years.[2] The pupils will initially have a sluggish response to light, progressing eventually to a complete absence of the light reflex. Close examination may show an atrophied iris with radial folds and crypt loss. Additionally, pupils will dilate slowly with atropine (or other mydriatics).[5]
Other findings to correlate the diagnosis of Argyll Robertson pupils are those suggestive of late-stage syphilis, such as:
- Tabes dorsalis: The posterior columns of the spinal cord and its dorsal root become affected in this stage of syphilis.
- Sensory ataxia: Lack of coordination due to a loss of sensory input into the control of movement (not from cerebellar pathology).
- Lancinating pains: Sudden, brief, and severe pains over the face, back, and limbs that can last minutes to days.
- Pupil irregularities: 50% of which will be distinctive Argyll Robertson pupils.[6]
Evaluation
Various tests can diagnose syphilis. The gold standard remains the visualization of spirochetes on darkfield microscopy.[7] More commonly, however, non-treponemal blood work for VRDL (venereal disease research laboratory) or RPR (rapid plasma reagin) is sent to rule in the disease. Then confirmatory testing assessing for FTA-ABS (fluorescent treponemal antibody absorption), TPPA (Treponema pallidum particle agglutination assay), or EIAs (syphilis enzyme immunoassays) is obtained.
A lumbar puncture is useful in the diagnosis of neurosyphilis in a patient with an unknown syphilis history who is presenting with a neurologic and ocular disease that could be consistent with the disease. Lumbar puncture is required to evaluate a patient with known syphilis presenting with these symptoms. Furthermore, a lumbar puncture is suggested in all HIV patients with syphilis, regardless of their presenting symptoms. CSF findings indicative of neurosyphilis will show greater than 20 WBC/microL and return positive for VRDL and intrathecal pallidum antibody index.[8]
Treatment / Management
No treatment for Argyll Robertson pupils is recognized; however, the progression can be controlled with the treatment of the underlying disease, syphilis. Treatment is with penicillin G benzathine IM. Alternatively, doxycycline (100 mg PO) can be used for patients with a penicillin allergy.[9][10] Ceftriaxone is also a safe alternative.[9] The treating clinician may have to distinguish which antibiotic to use based on the patient's history.
Differential Diagnosis
Several other conditions may present similarly to Argyll Robertson pupils, as they also demonstrate a light near dislocation. Either input or output failures can cause light-near dissociation. Bilateral pre-chiasmal lesions of the optic nerves, chiasmal lesions, or bilateral optic tract lesions could cause input failure, leading to a false light-near dissociation.
The light reflex will be reduced under these conditions, and the near reaction will be unaffected. Output failure is the cause of Argyll Robertson pupils, Adie’s pupil, the Miller-Fisher variant of acute idiopathic demyelinating polyradiculopathy, and in the setting of uncontrolled diabetes mellitus and certain peripheral neuropathies. The pupillary size can differentiate Argyll Robertson pupils from these conditions. These pupillary findings present with small pupils; the other diagnoses all demonstrate large light-dissociated pupils.[11]
Prognosis
The presence of Argyll Robertson pupils strongly indicates the diagnosis of neurosyphilis. This is a disease with a multi-organ impact and carries high morbidity. When Argyll Robertson pupils have been diagnosed, patients should begin immediate and potent treatment to eliminate the infection and halt the progression of the disease. The sooner the diagnosis is identified and treated, the better the prognosis for the patient.
Complications
Argyll Robertson pupils are found in the tertiary and final stage of infection with syphilis.[3] These patients are afflicted with neurologic and cardiovascular diseases. Such complications include an aortic aneurysm, insufficiency of the aortic valve, meningitis, and tabetic disease. While treatment can arrest the progression of the disease, the resolution of symptoms depends on the extent of the underlying disease. The damage is irreversible for those with cardiac or nerve involvement, and these patients carry the poorest prognosis.[12]
Deterrence and Patient Education
Prevention of the disease is through primary prevention. No vaccination for syphilis exists. Sexual education is recommended to prevent the transmission of syphilis.[13]
Enhancing Healthcare Team Outcomes
Patients with Argyll Robertson pupils implicating a late-stage syphilis infection can require a team of healthcare professionals to aid in their treatment and recovery. If presenting within an emergency or primary care setting, an infectious disease specialist should be consulted for the underlying infection or co-infections, and consultation with ophthalmology is strongly recommended. Patients may require cardiology and neurology depending on the extent and breadth of other symptoms.[13] Patients should be educated on safe sex practices to prevent transmission and re-infection.