Continuing Education Activity
Arachnoiditis is a persistent inflammation of the arachnoid mater and subarachnoid space. Clinical symptoms of arachnoiditis include severe back pain, paresthesia, limb weakness, and bladder or bowel dysfunction. Adhesive arachnoiditis is a severe form of this condition, and it can be painful and debilitating. Possible causes include mechanical, chemical, inflammatory, and infectious sources. Arachnoiditis is a rare, poorly understood, but serious condition. Understanding arachnoiditis can aid in accurate and prompt diagnosis and improve patient outcomes. This activity for healthcare professionals enhances the learners' competence in evaluating and managing arachnoiditis.
Objectives:
Identify the risk factors that may contribute to the development of arachnoiditis.
Determine the clinical presentation of arachnoiditis and differentiate this condition from similar neurologic disorders.
Identify evidence-based arachnoiditis management strategies and create a personalized treatment plan for a patient presenting with this condition.
Collaborate with the interprofessional team regarding short- and long-term, holistic care plans to improve outcomes for patients with arachnoiditis.
Introduction
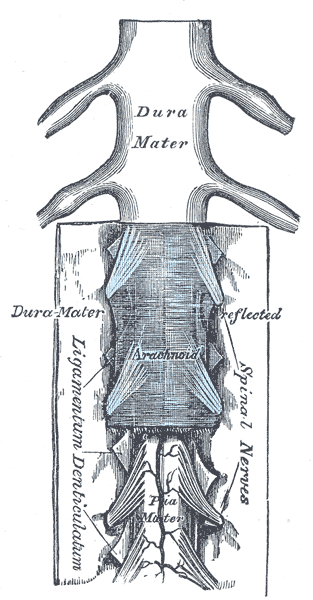
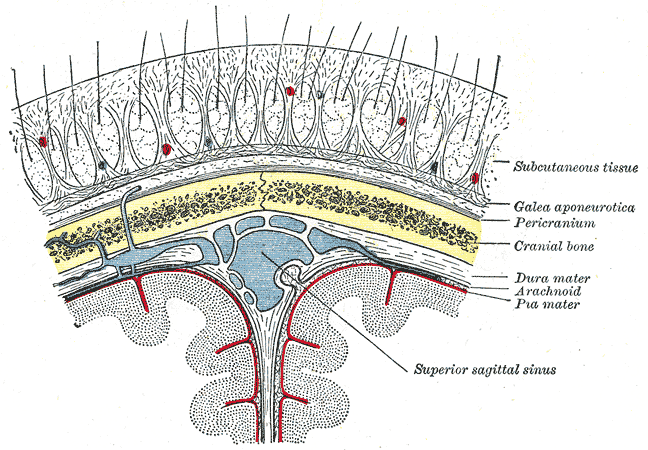
The meninges are membranous intracranial and intraspinal structures protecting the central nervous system (CNS) and providing a framework for the brain and spinal cord's vascular structures (see Image. Relationship of the Meniges to the Skull and Brain). The meninges consist of 3 layers: dura mater (dura), arachnoid mater (arachnoid), and pia mater (pia) (see Image. Spinal Cord and Meninges). The cerebrospinal fluid (CSF) circulates in the subarachnoid space—the space between the arachnoid and pia. This fluid delivers nutrients and helps maintain electrolyte and extracellular fluid balance in the CNS. The choroid plexuses of the 4 brain ventricles produce the CSF. The fluid exits the ventricular system and enters the subarachnoid space, where it acts as a cushion.
The dura mater adheres to the skull and vertebrae's internal aspect and has 2 sublayers: the external periosteal and internal meningeal layers. The external periosteal layer lines the internal periosteal surface. The fibrous internal meningeal layer is a strong membrane that is continuous at the foramen magnum, where the brain and spinal cord's dura layers meet. The epidural space is a potential space between the bone and dura mater that can enlarge with fluid or blood accumulation.
The dural venous sinuses are endothelium-lined cavities separating the periosteal and meningeal dural sublayers. Collections of arachnoid villi called "arachnoid granulations" protrude into the dural venous sinuses through the meningeal dural sublayer, where the CSF enters the venous system. The subdural space is a potential space separating the dura and arachnoid.
The arachnoid and pia mater closely adhere to each other, having developed from a single mesenchymal layer wrapping around the embryonic brain. Thus, these coverings are often referred to as "pia-arachnoid," "leptomeninx", or "leptomeninges." Fluid-filled spaces in these layers give rise to the subarachnoid space. Arachnoid trabeculae passing within the leptomeningeal layers resemble a spiderweb, thus the arachnoid mater's name.
The arachnoid matter contains collagen and elastic fibers and fibroblasts. CSF pressure closely applies this avascular membrane to the meningeal dural layer. The pia mater is a thin, highly vascularized membrane adhering tightly to the brain and spinal cord's surface.
The subarachnoid space is the space separating the arachnoid and pia. Unlike the epidural and subdural spaces, the subarachnoid is an actual space, as it contains trabecular cells and blood vessels. Freely flowing CSF suspends the CNS in this space.
Arachnoiditis is a persistent inflammation of the arachnoid mater and subarachnoid space, mostly in the spinal cord. The condition is poorly understood, though it is often related to prior spinal surgery, infection, subarachnoid hemorrhage (SAH), lumbar epidural injections, injection of oil-based myelographic contrast agents, and chemical irritation. Arachnoiditis may also be idiopathic.[1][2][3]
The condition induces leptomeningeal thickening, dural adhesions, scar tissue formation, and, often, nerve root clumping. Scar tissue can encapsulate the nerve roots, impede CSF flow, and lead to chronic adhesive arachnoiditis.[4] Arachnoiditis ossificans is arachnoid mater ossification that may arise from prolonged inflammation and produce progressive neurological debility (see Image. Arachnoiditis Ossificans). Spinal cord swelling and syringomyelia are some of the manifestations of advanced arachnoiditis.[5][6]
Etiology
The etiology of arachnoiditis is unknown. The time between exposure to a possible insult and the development of clinical symptoms is variable. Inconsistent imaging features also complicate the evaluation process. However, risk factors for the evolution of this condition are categorized as either chemical, mechanical, inflammatory, or infectious. These risk factors include the following:
- Chemical
- Exposures to neurotoxic substances like sulfite-containing preservatives
- Blood, such as from SAH
- Direct local anesthetic toxicity
- Contrast myelography
- Spinal anesthetic agents
- Accidental chemical injection
- Mechanical
- Trauma
- Surgical meningeal manipulation
- Spinal surgery
- Disk herniation
- Inflammatory
- Ankylosing spondylitis
- Guillain-Barré syndrome
- Autoimmune vasculitis
- Infectious
- Syphilis
- Tuberculosis
- HIV
- Viral infection
- Candida and other fungi
Arachnoiditis may also arise without any inciting event.
On exposure to an insult, meningeal scar tissue develops and encapsulates the nerve roots, impairs blood circulation, reduces oxygenation and nutrient delivery, and promotes waste product accumulation. Pain and neurological deficits result from these changes.
Previous trauma, spinal surgery, and SAH are among the most frequently reported causes of arachnoiditis. Chemical exposure may be intentional or unintentional.[7][8][9][10]
Epidemiology
Information about the epidemiology of arachnoiditis is limited. Since Horsley described the condition in 1909 as a disease entity, fewer than 1000 case reports exist in the literature. The true incidence or frequency of arachnoiditis is hard to determine due to its rarity, the diagnostic challenges it brings, and the variety of terms used in the literature to refer to this condition, including “chronic spinal meningitis” and “meningitis serosa circumscripta spinalis.” Arachnoiditis may be subclinical in some patients. Thus, the condition is likely underdiagnosed and underreported. However, the frequency of lumbar arachnoiditis has been recently observed to increase due to the increasing need for lumbar spine surgeries.
Pathophysiology
Exposure to an insult causes inflammation of the subarachnoid or subdural space, precipitating collagen deposits and fibrosis. Scar tissue forms, reducing CSF flow and impairing circulation, toxic metabolite clearance, oxygenation, and nutrient delivery to the neurons. Fibrosis leads to nerve root encapsulation, compression, damage, and atrophy. Arachnoiditis frequently results in pain and may be associated with neurological deficits.[11]
History and Physical
The clinical presentation of arachnoiditis varies widely. History may reveal a slow evolution of back and leg pain with associated multifocal sensory, motor, or reflex deficits. The severity of symptoms ranges from mild to severe and disabling, and the disease course may be static or progressive. The putative cause may be hard to identify, as the time frame from exposure to the onset of symptoms is inconsistent. For example, spinal adhesive arachnoiditis may be reported up to 10 months after an aneurysmal rupture.
Clinical symptoms vary according to the spine levels and severity of the arachnoiditis. Lumbar and thoracic involvement are the most common, followed by lumbosacral disease. Involvement of the entire spine is rare. As for severity, symptoms of severe arachnoiditis include disabling back pain, numbness, paresthesias, myeloradiculopathy symptoms of the lower limb, bowel or bladder dysfunction, sexual dysfunction, difficulty sitting for long periods, and motor weakness.[12]
The most common symptoms of arachnoiditis include back pain, radicular pain, and sensory defects. Motor weakness, gait imbalance, and neurogenic bowel or bladder are less frequent. Urinary symptoms develop late in 23% of arachnoiditis patients and are often characterized by urgency, increased frequency, and less commonly, incontinence. Paraplegia and isolated low-back pain have also been documented.
The neurologic symptoms vary in location and severity. A complete neurologic examination must be performed for all patients suspected of arachnoiditis to guide diagnosis and management.
Evaluation
Arachnoiditis is a clinical diagnosis. Laboratory tests and neurophysiologic modalities like electromyography and nerve conduction studies yield inconsistent results and are not used to formally diagnose the condition.[13][14]
Magnetic resonance imaging (MRI) and computed tomography (CT) myelography have high sensitivity, specificity, and accuracy for chronic adhesive arachnoiditis and may be used to support the clinical findings. However, radiologic features do not always correspond to clinical findings and their severity. Direct visualization by thecaloscopy can help detect loculated arachnoid cysts if MRI results are inconclusive. A spinal cord biopsy is sometimes indicated to exclude the presence of tumors when cord swelling and an intramedullary increased signal are present.[15]
The most frequent MRI findings are loculated arachnoid cysts involving several vertebral bodies or possibly the entire spine. Other common MRI findings include spinal cord swelling with or without increased T2 signal, cord displacement, cord atrophy, nerve root clumping, syrinx formation, and arachnoid septations. Meanwhile, the typical CT myelography findings are myelography spread block, thickened or tethered nerve roots, soft tissue mass within the arachnoid space, and intrathecal calcification.
Of the two, MRI is the imaging modality of choice for adhesive arachnoiditis because it can differentiate between benign meningeal calcification from frank arachnoid tissue ossification. However, non-contrast-enhanced CT is more sensitive than MRI for diagnosing arachnoiditis ossificans.
Treatment / Management
Arachnoiditis has no definitive cure and is often challenging to treat. The management is primarily supportive, focusing mainly on alleviating the symptoms and improving the patient's quality of life. Pain can cause functional limitations. Thus, multimodal and interprofessional pain management strategies are recommended. Medical management may include nonsteroidal anti-inflammatory drugs and opioids. Adjuncts like duloxetine, gabapentin, and pregabalin and muscle relaxants like baclofen may be combined with analgesics.[16]
Physical therapy and psychological strategies like cognitive behavioral therapy, biofeedback, and imagery can modulate a patient's pain perception and help improve symptoms. Individuals who experience difficulty sitting due to pain may benefit significantly from motorized assistive devices like standing wheelchairs. These devices can help improve mobility and quality of life. However, standing acceptance and vibration endurance should be evaluated before proceeding.
Thecaloscopy with dissection of cysts and adhesions and pain-modulating neurostimulation can help alleviate the symptoms, though arachnoiditis can recur afterward. Intrathecal therapy has also been used, though it can worsen the condition.
Surgery's role remains unclear. However, surgery can release a tethered cord and restore CSF flow. Reported surgical interventions include shunting, cyst fenestration, myelotomy, duraplasty, adhesiolysis, and laminectomy.
However, the long-term prognosis after surgery is poor. Surgery can produce immediate improvement, often followed by relapse and progressively worsening symptoms. Decompressive resection of isolated ossified plaques in arachnoiditis ossificans can provide temporary relief, but the condition's outcome remains poor. Various treatment options can restore CSF flow in advanced chronic adhesive arachnoiditis with CSF flow obstruction. However, these interventions do not prevent recurrence.
Preventing arachnoiditis by treating an epidural infection early may be the only case where early surgical intervention is beneficial. Local reduction of the infection can prevent inflammation from passing through the dural sac and causing severe adhesive arachnoiditis.
Improvement after epidural steroid injections has been reported. However, this modality is generally not recommended, as chemical spinal injections can exacerbate the condition. Oral corticosteroids have not shown any therapeutic benefit.
Differential Diagnosis
The differential diagnosis of arachnoiditis includes various conditions affecting the spinal cord, including the following:
- Spinal cord tumors
- Disk herniations
- Postlaminectomy pain syndrome
- Multiple sclerosis
- Cauda equina syndrome
- Syringomyelia
- Epidural abscess
- Epidural hematoma
- CNS infection [17]
A thorough clinical evaluation supported by imaging findings can help distinguish arachnoiditis from these conditions.
Prognosis
The course of arachnoiditis is highly variable, as this condition can be stable for some individuals but progressive for others. Most patients with arachnoiditis have a relatively stable functional disability with neither significant symptom exacerbation nor improvement from the time of diagnosis. However, symptom severity can fluctuate.
Some individuals may experience a progressive course, developing significant pain, disability, and poor quality of life in the advanced stages. Surgery often does not help and can even aggravate the condition.
Arachnoiditis may cause permanent disability, though the condition itself is usually not life-threatening. Still, the manifestations of severe arachnoiditis can be psychologically detrimental to affected patients. A long-term follow-up study of 50 individuals with arachnoiditis revealed death by suicide in 2 patients and death from causes not directly related to arachnoiditis. The condition tends to shorten patients' life span by an average of 12 years.
Complications
The possible complications of arachnoiditis include the following:
- Chronic pain
- Debilitating neurologic deficits
- Syringomyelia
- Hydrocephalus
- Arachnoid cysts
- Sexual dysfunction
- Loss of bladder and bowel control
Supportive measures, physical therapy, and psychosocial support can help mitigate this condition's manifestations and improve patient outcomes.
Deterrence and Patient Education
Preventing arachnoiditis primarily involves minimizing the risk factors associated with its development. While not all cases of arachnoiditis are preventable, especially in instances where it may result as an unforeseen complication of a procedure or another medical condition, certain precautions can help reduce the likelihood of its occurrence. Here are some general preventive measures:
- Minimizing invasive spinal procedures
- Preventing infections
- Avoiding intrathecal injections
- Using spinal medications and myelogram dyes carefully
- Regular monitoring of individuals undergoing multiple spinal procedures
- Seeking expert spinal care
- Educating patients about healthy lifestyle habits to prevent obesity-related spinal conditions like SAH and disk herniation
These measures may help reduce the risk of arachnoiditis but do not guarantee prevention. Since many arachnoiditis cases arise from iatrogenic causes, spinal procedures' risks and benefits must be thoroughly explained to patients to ensure they make an informed decision before giving consent.
Pearls and Other Issues
The key points about arachnoiditis evaluation and management are the following:
- The diagnosis of arachnoiditis is clinical.
- Spine MRI is the modality of choice for chronic adhesive arachnoiditis.
- Arachnoiditis has no definitive cure. Treatment primarily focuses on managing symptoms, improving quality of life, and preventing further progression.
- Tailored pain management strategies may include medications, physical therapy, and interventional procedures.
- Managing arachnoiditis requires collaboration among healthcare professionals from various specialties, including neurology, pain management, physical therapy, and mental health.
- Minimizing spinal procedures and CNS infection risk can reduce the risk of developing this condition.
- Mental health support, including counseling and coping strategies, can significantly improve a patient's well-being.
- The condition presents variably. Treatment plans should be tailored to address specific patient needs.
Arachnoiditis can be challenging to diagnose early on, as symptoms may be nonspecific and overlap with other spinal conditions. A detailed clinical evaluation that includes patient history and appropriate imaging studies is crucial.
Enhancing Healthcare Team Outcomes
An interprofessional approach offers patients with arachnoiditis the best chance of improving their functionality and quality of life. The members of the interprofessional team should include the following:
- Primary care physicians: responsible for the initial patient evaluation, diagnosis, and care coordination. These providers may prescribe medications for pain management and refer to specialists as needed.
- Radiologists: interpret imaging studies to aid in diagnosing and monitoring arachnoiditis.
- Neurologists or neurosurgeons: share their expertise in specialized evaluation of neurological symptoms and potential surgical interventions.
- Pain management specialists: develop and manage pain control strategies, which may include medications, nerve blocks, or other interventional procedures.
- Physical therapists: develop rehabilitation strategies to improve patient mobility, strength, and flexibility. These professionals may also educate patients with arachnoiditis on proper body mechanics and exercises to enhance functional capacity.
- Occupational therapists: focus on enhancing the patient's ability to perform daily activities. These providers may recommend adaptive techniques, assistive devices, and modifications to the living environment.
- Mental health professionals: counsel patients on coping strategies and mental health management.
- Urologists and gastroenterologists: manage bladder and bowel dysfunction associated with arachnoiditis.
- Nurses: monitor and manage symptoms, communicate with other team members, and educate the patient on self-care.
- Pharmacists: Collaborate with the healthcare team to manage medications effectively.
Regular communication and collaboration among these team members are essential for providing comprehensive care to individuals with arachnoiditis. The interdisciplinary approach ensures that the diverse aspects of the condition, including pain management, rehabilitation, psychological well-being, and overall quality of life, are addressed.