[1]
Hafezi F, Nouhi A. Safe abdominoplasty with extensive liposuctioning. Annals of plastic surgery. 2006 Aug:57(2):149-53
[PubMed PMID: 16861993]
[2]
Hunecke P, Toll M, Mann O, Izbicki JR, Blessmann M, Grupp K. Clinical outcome of patients undergoing abdominoplasty after massive weight loss. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2019 Aug:15(8):1362-1366. doi: 10.1016/j.soard.2019.06.001. Epub 2019 Jun 12
[PubMed PMID: 31296446]
Level 2 (mid-level) evidence
[3]
Frank K, Hamade H, Casabona G, Gotkin RH, Kaye KO, Tiryaki T, Freytag DL, Bialowas C, Koban KC, Cotofana S. Influences of Age, Gender, and Body Mass Index on the Thickness of the Abdominal Fatty Layers and its Relevance for Abdominal Liposuction and Abdominoplasty. Aesthetic surgery journal. 2019 Sep 13:39(10):1085-1093. doi: 10.1093/asj/sjz131. Epub
[PubMed PMID: 31056694]
[4]
Gupta V, Winocour J, Rodriguez-Feo C, Bamba R, Shack RB, Grotting JC, Higdon KK. Safety of Aesthetic Surgery in the Overweight Patient: Analysis of 127,961 Patients. Aesthetic surgery journal. 2016 Jun:36(6):718-29. doi: 10.1093/asj/sjv268. Epub 2016 Feb 9
[PubMed PMID: 26895958]
[5]
Ho W, Jones CD, Pitt E, Hallam MJ. Meta-analysis on the comparative efficacy of drains, progressive tension sutures and subscarpal fat preservation in reducing complications of abdominoplasty. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2020 May:73(5):828-840. doi: 10.1016/j.bjps.2019.11.066. Epub 2020 Feb 1
[PubMed PMID: 32057746]
Level 2 (mid-level) evidence
[6]
Vallim MG, Calderoni DR, Bueno MA, Motta MM, Basso RC, Kharmandayan P. Patient Versus Surgeon Preferences Between Traditional and Neo-omphaloplasty in Post-bariatric Abdominoplasty. Aesthetic plastic surgery. 2017 Feb:41(1):102-107. doi: 10.1007/s00266-016-0753-3. Epub 2016 Dec 28
[PubMed PMID: 28032175]
[7]
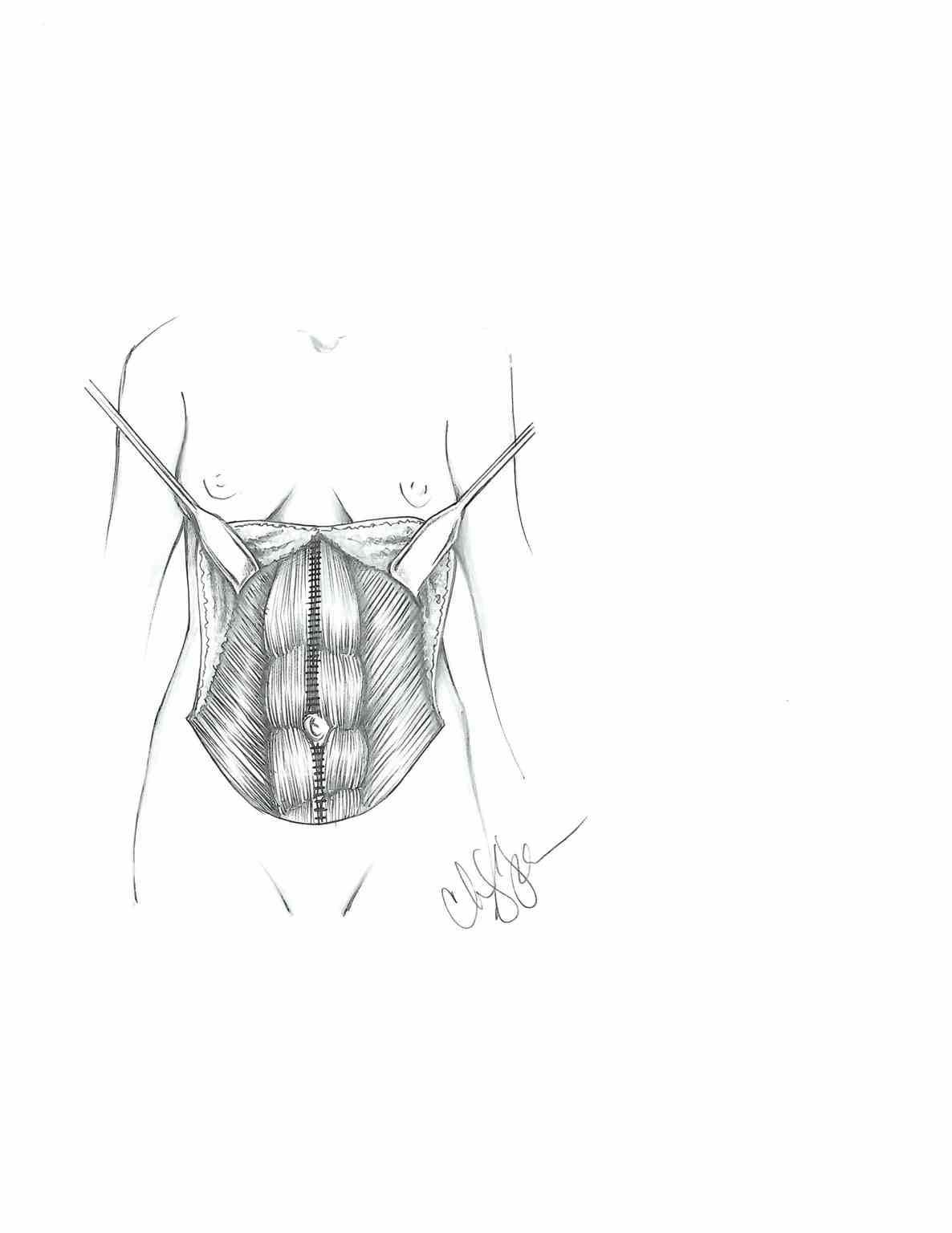
Hoyos AE, Perez ME, Castillo L. Dynamic definition mini-lipoabdominoplasty combining multilayer liposculpture, fat grafting, and muscular plication. Aesthetic surgery journal. 2013 May:33(4):545-60. doi: 10.1177/1090820X13484493. Epub
[PubMed PMID: 23636628]
[8]
Ariyan S, Martin J, Lal A, Cheng D, Borah GL, Chung KC, Conly J, Havlik R, Lee WPA, McGrath MH, Pribaz J, Young VL. Antibiotic prophylaxis for preventing surgical-site infection in plastic surgery: an evidence-based consensus conference statement from the American Association of Plastic Surgeons. Plastic and reconstructive surgery. 2015 Jun:135(6):1723-1739. doi: 10.1097/PRS.0000000000001265. Epub
[PubMed PMID: 25724064]
Level 3 (low-level) evidence
[9]
Pallara T, Del Buono R, Marangi GF, Langella M, Toto V, Persichetti P. Outcomes of traditional cosmetic abdominoplasty in a community setting: a retrospective analysis of 1008 patients. Plastic and reconstructive surgery. 2013 Nov:132(5):863e-864e. doi: 10.1097/PRS.0b013e3182a4c3e8. Epub
[PubMed PMID: 24165640]
Level 2 (mid-level) evidence
[10]
Bertheuil N, Carloni R, Herlin C, Watier E, Chaput B. Abdominoplasty: Risk Factors, Complication Rates, and Safety of Combined Procedures. Plastic and reconstructive surgery. 2016 Jun:137(6):1051e-1052e. doi: 10.1097/PRS.0000000000002197. Epub
[PubMed PMID: 26890513]
[11]
Massenburg BB, Sanati-Mehrizy P, Jablonka EM, Taub PJ. Risk Factors for Readmission and Adverse Outcomes in Abdominoplasty. Plastic and reconstructive surgery. 2015 Nov:136(5):968-977. doi: 10.1097/PRS.0000000000001680. Epub
[PubMed PMID: 26505701]
[12]
Gutowski KA. Evidence-Based Medicine: Abdominoplasty. Plastic and reconstructive surgery. 2018 Feb:141(2):286e-299e. doi: 10.1097/PRS.0000000000004232. Epub
[PubMed PMID: 29373443]