[1]
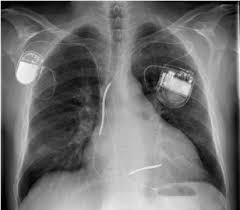
Carrión-Camacho MR, Marín-León I, Molina-Doñoro JM, González-López JR. Safety of Permanent Pacemaker Implantation: A Prospective Study. Journal of clinical medicine. 2019 Jan 1:8(1):. doi: 10.3390/jcm8010035. Epub 2019 Jan 1
[PubMed PMID: 30609668]
[2]
Parkash R, Sapp J, Gardner M, Gray C, Abdelwahab A, Cox J. Use of Administrative Data to Monitor Cardiac Implantable Electronic Device Complications. The Canadian journal of cardiology. 2019 Jan:35(1):100-103. doi: 10.1016/j.cjca.2018.10.018. Epub 2018 Nov 13
[PubMed PMID: 30595171]
[3]
Polimenakos AC, Mathis L, Shafer B, Kamath MV. Selective Use of Temporary Epicardial Pacing Leads in Early Infancy Following Cardiac Surgery: Feasibility and Determinants of Clinical Application. Pediatric cardiology. 2019 Mar:40(3):630-637. doi: 10.1007/s00246-018-2037-y. Epub 2018 Dec 18
[PubMed PMID: 30564866]
Level 2 (mid-level) evidence
[4]
Bob-Manuel T, Nanda A, Latham S, Pour-Ghaz I, Skelton WP 4th, Khouzam RN. Permanent pacemaker insertion in patients with conduction abnormalities post transcatheter aortic valve replacement: a review and proposed guidelines. Annals of translational medicine. 2018 Jan:6(1):11. doi: 10.21037/atm.2017.10.21. Epub
[PubMed PMID: 29404357]
[5]
Kosztin A, Boros AM, Geller L, Merkely B. Cardiac resynchronisation therapy: current benefits and pitfalls. Kardiologia polska. 2018:76(10):1420-1425. doi: 10.5603/KP.a2018.0160. Epub 2018 Aug 9
[PubMed PMID: 30091132]
[6]
Proclemer A, Zecchin M, D'Onofrio A, Boriani G, Facchin D, Rebellato L, Ghidina M, Bianco G, Bernardelli E, Pucher E, Gregori D. [The Pacemaker and Implantable Cardioverter-Defibrillator Registry of the Italian Association of Arrhythmology and Cardiac Pacing - Annual report 2016]. Giornale italiano di cardiologia (2006). 2018 Feb:19(2):119-131. doi: 10.1714/2868.28944. Epub
[PubMed PMID: 29531385]
[7]
Proclemer A, Zecchin M, D'Onofrio A, Botto GL, Facchin D, Rebellato L, Ghidina M, Bianco G, Bernardelli E, Pucher E, Gregori D. [The Pacemaker and Implantable Cardioverter-Defibrillator Registry of the Italian Association of Arrhythmology and Cardiac Pacing--Annual report 2014]. Giornale italiano di cardiologia (2006). 2016 Feb:17(2):95-107. doi: 10.1714/2174.23494. Epub
[PubMed PMID: 27029759]
[8]
Samii SM. Indications for pacemakers, implantable cardioverter-defibrillator and cardiac resynchronization devices. The Medical clinics of North America. 2015 Jul:99(4):795-804. doi: 10.1016/j.mcna.2015.02.008. Epub
[PubMed PMID: 26042883]
[9]
Zartner P. [Antibradycardia therapy : Indication and implementation]. Herzschrittmachertherapie & Elektrophysiologie. 2016 Jun:27(2):88-94. doi: 10.1007/s00399-016-0426-6. Epub 2016 May 24
[PubMed PMID: 27221084]
[10]
Poh PG, Liew C, Yeo C, Chong LR, Tan A, Poh A. Cardiovascular implantable electronic devices: a review of the dangers and difficulties in MR scanning and attempts to improve safety. Insights into imaging. 2017 Aug:8(4):405-418. doi: 10.1007/s13244-017-0556-3. Epub 2017 Jun 17
[PubMed PMID: 28624970]